When aching pain in a tooth appears, a person is simply unable to think about anything else, because this is one of the most unpleasant sensations. Moreover, it often happens that the pain begins at night or at times when dental care is not available (at the dacha, on a trip, etc.), and it is not possible to immediately see a doctor for treatment. Why does pain occur, and how to soothe an aching tooth before visiting the dentist?
What causes aching pain in a tooth?
The main causes of pain are:
- Infectious lesions of dental units: caries, pulpitis, periodontitis. Even in the later stages, these diseases may not give a clearly defined clinical picture and may only manifest as persistent aching pain inside the tooth when exposed to any irritant.
- Too thin enamel layer, cracks and chips in the enamel.
- Periodontitis. In some cases, gum inflammation is accompanied by throbbing toothache.
- Treatment or tooth extraction. Aching pain often appears after the removal of a wisdom tooth or any other tooth - this is a normal reaction to the operation, and usually the painful sensations gradually go away on their own after a few days. Also, aching pain in the tooth often occurs after removal of the nerve - this is a common reaction of the body to treatment and does not require special therapy.
How to soothe an aching tooth?
If aching pain inside a tooth or after the removal of a wisdom tooth prevents you from sleeping peacefully or generally thinking about anything else, you need to take care to reduce it to a minimum. And at the first opportunity, be sure to consult a dentist, because pain relief does not mean that the problem has been eliminated, and there is no need for treatment. You can eliminate pain as follows:
- First of all, thoroughly brush your teeth and remove any remaining food from the interdental spaces.
- Rinse your mouth with a soda-salt solution (a teaspoon of soda and salt per glass of warm boiled water). You can use only saline solution or just warm water if nothing else is available.
- Take a pain reliever (analgin, paracetamol, ibuprofen) if possible.
- If there are no medications at hand, you can relieve pain with folk remedies. Rinsing with decoctions of chamomile, calendula, sage, and calamus root helps to cope well with toothache. You can also use tampons soaked in clove, sea buckthorn or mint oil, which should be applied to the affected area. Rinsing with alcohol-containing liquids - propolis tincture, regular vodka or cognac (sweetened alcohol-containing drinks cannot be used for this purpose!) can help get rid of pain.
It is strictly not recommended to use warming procedures in this case - rinsing should be at approximately room temperature, warm compresses and heating pads should not be applied to the sore area. Heat only accelerates and intensifies the inflammatory process, which can provoke the rapid development of a purulent abscess and the spread of inflammation to nearby tissues.
Ibuprofen belongs to the group of non-steroidal anti-inflammatory drugs (NSAIDs), which represent a large and chemically diverse group of drugs that are widely used in clinical practice.
Despite the fact that in recent years the number of NSAIDs has increased significantly and this group includes a lot of drugs that differ in chemical structure, features of action and application, ibuprofen remains the drug of choice for the treatment of pain and fever, especially in pediatric practice.
History of development
The history of the discovery of the drug began in 1957, when Stuart Adams, together with chemist John Nicholson, began to study the group of phenylpropionic acids. In 1962, the molecule BTS 13621 was created, now commonly known as ibuprofen. During preclinical and clinical studies, the drug showed good efficacy, good tolerability and caused less pronounced side effects from the gastrointestinal tract (GIT) than acetylsalicylic acid (ASA). For clinical use, the drug was registered on January 12, 1962 by the British Patent Office under the name Brufen. It was intended to be prescribed to patients with rheumatoid arthritis by prescription.
In the USA, the drug was registered in 1974 under the trade name Motrin.
Taking into account the accumulated clinical experience and the results of clinical studies, the indications for prescribing ibuprofen have expanded. In the UK, the drug has been marketed as an over-the-counter medicine since 1983 under the name Nurofen. In 1984, the drug acquired over-the-counter status in the USA. And by the end of 1985, more than 100 million people were using Nurofen in more than 120 countries. In 1985, Boots was awarded a Queen's Award in recognition of scientific and technical achievements in the development of the drug ibuprofen.
In 2006, based on data on the safety and effectiveness of ibuprofen obtained in clinical studies, a new indication for the drug was added - use in children over 6 years of age.
A drug with the trade name “Nurofen” (200 mg tablets) appeared on the Russian market in 1997; in subsequent years the following forms of ibuprofen were registered in Russia:
1998 – “Nurofen for children” (ibuprofen, 100 mg/5 ml);
2001 – “Nurofen Plus” (ibuprofen, 200 mg + codeine phosphate, 12.8 mg);
2002 – “Nurofen” effervescent tablets – the first soluble ibuprofen in Russia;
2003 – “Nurofen UltraCap” – capsules with ibuprofen solution inside;
2005 – “Nurofen forte” (ibuprofen, 400 mg);
2005 – “Nurofen” gel;
2006 – “Nurofen for children” with strawberry flavor;
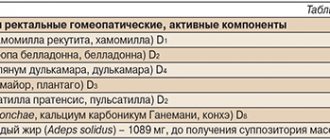
2008 – “Nurofen for children” rectal suppositories, registered in Russia.
Currently, the drug has many names and is used among both adults and children to relieve pain and fever. For children, an ibuprofen suspension (20 mg/ml) is used – “Nurofen for Children”, which does not contain sugar and is approved for over-the-counter use in children aged 6 months and older, as well as suppositories indicated for children aged 3 months and older [1].
Pharmacokinetics of ibuprofen
When taken orally, ibuprofen is partially absorbed in the stomach and then completely in the small intestine. The time to maximum plasma concentration (Tmax) is approximately 1–2 hours after oral administration of ibuprofen tablets or pediatric suspension, although a higher Tmax (3 hours) has been reported in infants 6–18 months of age. In human plasma, ibuprofen is 99% protein bound. The high degree of protein binding results in a relatively low volume of distribution (0.1 l/kg).
Ibuprofen is metabolized in the liver and is rapidly cleared from plasma with a relatively short half-life (about 2 hours). Less than 10% is excreted unchanged in the urine. The two main metabolites, 2-hydroxyibuprofen and 2-carboxyibuprofen, which are formed as a result of hydroxylation and subsequent oxidation, do not have pharmacological activity. Urinary excretion of metabolites is usually complete within 24 hours of the last dose. The total urinary excretion of ibuprofen and its metabolites is linearly dependent on dosage [2].
Mechanism of action of NSAIDs
The mechanism of action of NSAIDs is the ability to inhibit cyclooxygenase (COX), an enzyme that catalyzes the conversion of free polyunsaturated fatty acids (arachidonic acid) into prostaglandins (PGs), as well as other biologically active substances, in particular thromboxanes (TPA2) [3].
PGs have versatile biological activity:
- are mediators of the inflammatory response: they accumulate in the focus of inflammation and cause local vasodilation, edema, exudation, migration of leukocytes and other effects (mainly PGE2 and PGI2);
- sensitize receptors to pain mediators (histamine, bradykinin) and mechanical influences, lowering the sensitivity threshold;
- increase the sensitivity of the hypothalamic thermoregulation centers to the action of endogenous pyrogens formed in the body under the influence of microbes, viruses, toxins (mainly PGE2);
- perform the function of protecting the mucous membrane of the gastrointestinal tract (increasing the secretion of mucus and alkali; maintaining the integrity of endothelial cells inside the microvessels of the mucous membrane, helping to maintain blood flow in it; maintaining the integrity of granulocytes and, thus, maintaining the structural integrity of the mucous membrane);
- affect kidney function: cause vasodilation, maintain renal blood flow and glomerular filtration rate, increase renin release, sodium and water excretion, participate in potassium homeostasis.
In recent years, it has been recognized that there are two major cyclooxygenase isoenzymes that are inhibited by NSAIDs. The first isoenzyme, COX-1, controls the production of PGs, which regulate the integrity of the gastrointestinal mucosa, platelet function and renal blood flow; and the second, COX-2, is involved in the synthesis of PG during inflammation. Moreover, COX-2 is absent under normal conditions, but is formed under the influence of certain tissue factors that initiate the inflammatory response (for example, cytokines) [4]. In this regard, it is assumed that the anti-inflammatory effect of NSAIDs is due to inhibition of COX-2, and their adverse reactions are due to inhibition of COX-1 [5].
Studies modeling the interaction of ibuprofen stereoisomers with the corresponding COXs have shown the high affinity of this drug for the active center of COX-2, which explains its low ulcerogenic activity and high degree of safety in over-the-counter doses [6].
The severity of the anti-inflammatory properties of NSAIDs correlates with the degree of COX inhibition. Among them, the following order of activity is noted: meclofenamic acid, suprofen, indomethacin, diclofenac, mefenamic acid, flufenamic acid, naproxen, phenylbutazone, acetylsalicylic acid, ibuprofen.
Ibuprofen, when used in low (“over-the-counter”) doses, 800–1200 mg/day, has an analgesic and anti-inflammatory effect, with a safety profile comparable to paracetamol. When used in high doses, 1800–2400 mg/day, especially for a long time in patients suffering from severe diseases of the musculoskeletal system (osteoarthritis), ibuprofen exhibits a therapeutic effect similar to that of coxibs. This property of ibuprofen is explained by its moderate activity in inhibiting COX-1 and COX-2, as well as the short half-life of the drug [7].
There are several mechanisms of analgesic action of NSAIDs: central and peripheral [8]. The peripheral mechanism is mediated by the effect on PGs, which increase the sensitivity of pain receptors to physical and chemical stimulants, such as bradykinin, which in turn promotes the release of PGs from tissues [9].
The central mechanism is determined by the ability of NSAIDs to influence the thalamic centers of pain sensitivity (local blocking of PGE2, PGF2α in the central nervous system), resulting in inhibition of the transmission of pain impulses to the cortex [10].
The analgesic effect of NSAIDs is more pronounced for pain of mild and moderate intensity, which is localized in the muscles, joints, tendons, nerve trunks, as well as for headaches or toothaches. For severe visceral pain associated with injury, surgery, or a tumor, most NSAIDs are less effective and are inferior in pain relief to narcotic analgesics. At the same time, a number of controlled studies have shown a fairly high analgesic activity of ibuprofen, ketorolac, ketoprofen, metamizole for colic and postoperative pain. Based on the results of one of these studies, a comparative characteristic of the analgesic effect of the most commonly used NSAIDs in clinical practice was derived [11]: ketorolac 30 mg < (ketoprofen 25 mg = ibuprofen 400 mg, flurbiprofen 50 mg) > (ASA 650 mg = paracetamol 650 mg = fenoprofen 200 mg = naproxen 250 mg = etodolac 200 mg = diclofenac 50 mg = mefenamic acid 500 mg) > nabumetone 1000 mg. Based on the data presented, it can be noted that propionic acid derivatives have a higher analgesic activity: ketoprofen, ibuprofen, flubiprofen.
The effectiveness of NSAIDs for back pain of both vertebrogenic and non-vertebrogenic nature has been well studied and proven by numerous studies. Ibuprofen is one of the most preferred NSAIDs for the relief of back pain of various origins due to its more favorable spectrum of side effects compared to other representatives of this group. The large-scale randomized comparative clinical trial PAIN [12], which included more than 1400 patients, showed that ibuprofen at a dose of up to 1200 mg/day is characterized by similar tolerability as paracetamol and is superior to ASA in this regard.
Clinical experience of use for tension-type headaches shows [13] that the choice of ibuprofen in this situation is justified not only from the point of view of relieving painful episodes, but also in course prescription.
A clinical experimental study of the effectiveness of ibuprofen at a dose of 800 mg/day for 12 days shows a decrease under its influence in both the intensity of the pain syndrome (by 4.4 points on a visual analogue scale) and the degree of the negative impact of pain on the life activity of patients, an increase in the threshold of perception pain, as well as a decrease in the severity of accompanying pain manifestations. The pathogenetic justification for the use of NSAIDs in an acute attack of migraine cephalgia has clinical confirmation. The antimigraine effectiveness of ibuprofen in doses of 200 and 400 mg was studied in a double-blind, placebo-controlled study [14], which showed that the drug affects not only painful manifestations, but also the accompanying symptoms of nausea, photo- and phonophobia. Two hours after taking ibuprofen, these effects were observed in almost half of the cases (compared to 28% of controls). In this case, to relieve severe headaches, the use of 400 mg of ibuprofen was required. The effectiveness of a small dose of ibuprofen (200 mg) in relieving a mild to moderate migraine attack, assessed 2.5 hours after dosing, was equivalent to the effectiveness of 500 mg ASA, but the reduction in headache intensity occurred more quickly [15]. A study of the clinical effectiveness of ibuprofen (800 mg/day) in the preventive (course) treatment of migraine (for 14 days) demonstrated some features of its action [13]. Along with a decrease in the intensity of painful attacks, a slight decrease in their frequency was noted; The greatest changes were observed in the duration of a cephalalgia attack.
The trigger for the hyperthermic reaction is exogenous pyrogens (bacteria, viruses, toxins, allergens, medications), which, when entering the body, affect the thermal center of the hypothalamus through fever mediators. The first and most important of them is endogenous pyrogen - a low molecular weight protein produced by leukocytes (monocytes, macrophages) after activation by lymphokines. Endogenous pyrogen is specific for fever and acts on thermosensitive neurons of the preoptic region of the hypothalamus, where the synthesis of PGE1 and PGE2 is induced with the participation of serotonin. The essence of the antipyretic effect of NSAIDs comes down to inhibition of the transmission of excitation in the nuclei of the hypothalamus. Since PGs are not involved in maintaining normal body temperature, NSAIDs do not affect the normal temperature. The inhibitory effect of NSAIDs on thermoregulation is also expressed in a decrease in the release of serotonin, adrenaline and acetylcholine by the cells of the hypothalamus.
Ibuprofen at a dose of 400 mg is effective in reducing fever. Of the 2626 patients who took part in the randomized trial, 94% confirmed the high effectiveness, 91% confirmed the rapidity of action and 81% confirmed the duration of action of the drug [16].
Clinical studies have found that ibuprofen is more effective than paracetamol in reducing very high body temperature in children [17]. This effect was demonstrated in a double-blind, parallel-group study in children treated with single doses of ibuprofen 5 and 10 mg/kg, paracetamol 10 mg/kg, and placebo for fever. Ibuprofen at a dose of 10 mg/kg was more effective in reducing body temperature than paracetamol at a dose of 10 mg/kg, both in the subgroup of children with very high fever (39.2 °C; p < 0.05) and in the entire group in overall (p < 0.05).
The rapid metabolism and excretion of ibuprofen goes some way to explaining the relatively low toxicity of this drug compared to some other NSAIDs. A study that included more than 84 thousand children aged 6 months to 12 years showed that the risk of serious side effects with ibuprofen was no higher than with paracetamol [18].
Undesirable effects
The meta-analysis by D. Henry et al. focused primarily on serious upper gastrointestinal complications associated with NSAID use, which are the most common adverse effects of treatment with these drugs. Based on the data obtained, the authors arranged widely used NSAIDs in a certain sequence and concluded that long-term use of all these drugs leads to the development of gastrointestinal complications. At the same time, taking ibuprofen in a dose of up to 2400 mg/day is associated with the lowest risk of developing severe gastrointestinal complications and according to this indicator, NSAIDs are ranked as follows: ibuprofen < ASA < diclofenac < naproxen < indomethacin < piroxicam [19].
A number of studies have analyzed the risk of myocardial infarction in patients taking NSAIDs [21, 22]. In the group of patients using a therapeutic dose of ibuprofen in treatment, the risk of developing a heart attack was minimal compared with diclofenac and rofecoxib: 1.07 (95% confidence interval [CI] - 1.02–1.12) versus 1.44 (95% CI – 1.32–1.56) and 1.26 (95% CI – 1.17–1.36), respectively [21].
The safety of ibuprofen in children was demonstrated in a large, randomized, double-blind study [23]. We assessed the increased risk of hospitalization in children receiving ibuprofen 5 or 10 mg/kg for fever (n = 55,765) compared with children receiving paracetamol 12 mg/kg (n = 28,130). Of the 83,915 children whose data were analyzed, 795 (1%) were admitted to hospital within 4 weeks of study entry. Ibuprofen, compared with paracetamol, did not increase the risk of hospitalization associated with any of the 4 serious treatment outcomes of gastrointestinal bleeding, development of renal failure, anaphylaxis or Reye's syndrome. To date, not a single case of the development of Reye's syndrome has been reported in children with viral diseases treated with ibuprofen [2].
Data from a meta-analysis (2009), which included 24 randomized clinical trials, showed that the tolerability and safety of ibuprofen in children under 18 years of age is similar to that of placebo and higher than that of paracetamol [24].
It has been established that after the age of 2 months, the kidneys in children are well enough developed to cope with the elimination of ibuprofen through glomerular filtration. A study including 49 children aged 3 months to 12 years showed no age-related differences in the rate of absorption and elimination of ibuprofen [20].
In 2010, data were published on the use of intravenous ibuprofen for the treatment of postoperative pain, acute pain and fever as a safe and well-tolerated NSAID, in particular in children, patients with cystic fibrosis, and elderly patients [25]. This makes it possible to use ibuprofen in a hospital, providing higher bioavailability, speed of onset of effect and effectiveness.
A study was conducted on the tolerability and safety of the use of ibuprofen in rectal suppositories in children. Children who were in 11 children's departments and clinics in Israel and needed antipyretic medications were prescribed ibuprofen suppositories (5–10 mg/kg). Treatment was carried out for 3 to 7 days. During the study, a physical examination of children was performed, body temperature was monitored, and parents were interviewed to identify adverse reactions during therapy and assess the child’s condition. A total of 490 children completed the study. The study noted high parental satisfaction with the therapy (4.5 ± 0.47 points on a scale of 1–5), with 92.2% of respondents saying they would use the medicine in the future. Adverse reactions were reported in 8 patients (1.63%), the most common of which was diarrhea, which did not require discontinuation of the drug [26].
A Russian multicenter open study was also conducted [27], the purpose of which was to evaluate the clinical effectiveness, tolerability and safety of the drug Nurofen for children (ibuprofen) rectal suppositories in the treatment of hyperthermic conditions in children with acute respiratory diseases. When assessing the effectiveness of ibuprofen compared to paracetamol during the first 30 minutes and 1 hour, no significant differences were noted between the groups: the average decrease in temperature in the observation group was 0.6 ± 0.2 and 1.3 ± 0.6 °C , in the control group – 0.7 ± 0.3 and 1.2 ± 0.5 °C, respectively. However, within 1 hour after using the antipyretic drug in the observation group (children receiving ibuprofen), temperature normalization occurred in 10% (3) of patients, while in the control group all children remained hyperthermia. During the first three hours, temperature normalization occurred in a third (10 children) of the group receiving ibuprofen, which was significantly higher than in the control group (3.3% - 1 child). During the first 6 hours, this trend persisted and normalization of temperature was achieved in 63.3% (19) of children in the observation group versus 36.7% (11) of patients in the control group. 72 hours after the use of antipyretic drugs, the number of children who did not have hyperthermia was equal in both groups and amounted to 86.7%.
According to the study results, the intensity of the intoxication syndrome decreased faster (within 3–6 hours) in the observation group (children receiving ibuprofen) compared to the control group.
Ibuprofen (Nurofen) meets all the requirements for an “ideal” over-the-counter analgesic: availability in various dosage forms (tablets, capsules, suspensions) that are quickly absorbed in the stomach and intestines; rapid creation of peak plasma concentrations; relatively short half-life and at the same time long-lasting effect; minimal spectrum of side effects with occasional and short-term doses, good range of safety and tolerability in children. The benefits of this drug have been demonstrated in international multicenter and randomized clinical trials. These facts are very important from the point of view of choosing the most optimal NSAID for the treatment of pain and fever. It is necessary to take into account the fact that the main side effects of NSAIDs, including gastrointestinal ones, are dose-dependent. And relief of pain and fever involves the use of ibuprofen (Nurofen) in analgesic and antipyretic doses, which are lower than anti-inflammatory doses and, accordingly, less dangerous for the patient.
Information about the author: Erofeeva Svetlana Borisovna – Candidate of Medical Sciences, doctor, clinical pharmacologist, City Clinical Hospital No. 61. E-mail