Sometimes in dentistry a moment arises when a regular filling is not enough, but covering a tooth with a crown is still blasphemous. Then a diverse group of tabs comes to the rescue. Diverse in types and manufacturing methods. Inlays are prostheses (or microprostheses) that restore defects in the hard tissues of teeth, and as a result, the function and aesthetics of individual teeth and the entire dental system.
But they are not common. Not that they are extremely rare, but like marginals, they are on the border of two large restoration paths, and each of them is trying to occupy a large niche. On the one hand, these are fillings that are made here and now, quite quickly and cost-effectively. Another niche is crowns, which are used for more significant defects, and also occur in cases where an inlay can be used, but due to their higher functional qualities, longer service life and better aesthetics, they are more widespread among doctors.
Then why do we need them? But because they are more perfect than fillings in functional terms, and are more tolerant of tooth tissues than crowns, but in a harsh market they find themselves in the background.
Types of tabs
Among a number of classifications of inlays, the classification of the American Dental Association ADA stands out. On the one hand, this is due to the big name of the organization that has entered itself above the classification. On the other hand, it divides different types of inlays in a way that is more significant from a practical point of view than simply referring to the location of the hard tissue defect.
So, according to ADA, tabs are classified into 4 types:
- Inlay
- Onlay
- Overlay
- Pinlay
Inlay
The simplest type of tab, in which one or more surfaces are restored, but the main thing! without restoration of the tubercles. According to the name “inlay”, the tab lies inside the tooth. From a functional point of view, this is important, since in this case the tab is, as it were, sandwiched between the tubercles. In this case, even when the side surfaces are restored, the load on the tab falls at an angle close to a straight line and does not lead to displacement of the structure, which determines its high viability. But it is precisely this type of inlay that is most severely oppressed by fillings. It is not difficult to restore such defects with filling material, and the price between a filling and an inlay varies significantly, which, while welcomed by the patient, also requires more time for its manufacture, which negatively affects medical preferences.
Onlay
In situations where one or more cusps are destroyed or do not represent functional value, they are covered with an inlay. Then some of the cusps of the tooth remain their own, and some are replaced by an inlay. And this is the main design feature of Onlay tabs. But alas, not a plus.
The biomechanics of the dental system is such that the cusps almost never take the load at a right angle. Unlike the occlusal surface in the fissure area, where the inlay is conditionally driven even further into the tooth, inlays with an overlapping cusp perceive the load in completely different directions. This provokes a capsizing moment. A conventional artificial crown, taking pressure on the cusps on one side, has a kind of anchoring on the other side, expressed in the overlap of the cusps, which are not subject to load at the moment. As a result, Onlay-type structures are in a kind of decompensation, when the pressure exerted is not counteracted by sufficient fixation. This causes significant damage to the reputation of this type of tab.
Overlay
A type of inlay in which all the cusps of the tooth are covered, which is why some authors equate them to crowns. The so-called equatorial crowns. The advantages in comparison with the previous type of crowns are obvious, and are due to the overlap of all the cusps. And here crowns are already competing with Overlay tabs.
The bottom line is that the larger the surface of the contacting surfaces, the stronger the fixation of the structure, which we remember from the school physics course. Crowns and overlays completely cover the occlusal surface of the tooth, and here they can only compete in the complete coverage of the lateral surfaces. This indicator is obviously better for crowns. And given that the crown is a cylinder, all the walls are united and close to parallelism, which significantly potentiates the mechanical adhesion of the artificial crown and the tooth stump. It simply doesn’t cost the doctor anything to prepare the walls a little more, place the preparation border under the gum or at its level and achieve significantly better fixation of the structure.
Pinlay
Pinlay is a special type of inlay that has a pin in its design, with the help of which there is better fixation in the hard tissues of the tooth. As a result, it can be applied to any type of inlay, on any tooth, is functionally justified, requires a little more skill, is a little more difficult to manufacture, and is rare.
My opinion is that the use of a pin can improve the fixation of a tooth inlay, and, provided that when a regular inlay becomes uncemented and falls out, the inlay with the pin will remain in place, and the lack of cement will be gladly filled by microorganisms and the carious process. And it turns out that de-cementation, acceptable in terms of regularity, will be a kind of prevention, provided that the dropped insert does not end up in the patient’s lungs or gastrointestinal tract.
In addition to the ADA classification, there are other classifications that involve linking the tab to the location of the defect. For example, to:
- Black classification with grades 5-6
- Boyanov classification with designation of mesial (M), distal (D) or occlusal (O) localization of the defect or their combination
- Kurlyandsky classification with 3 types of defect localization, intersecting with the previous classification.
Tabs are also classified depending on the material from which they can be made. They can do many things:
- Plastic
- All metal
- Combined metal-plastic or metal-ceramic
- All-ceramic
- Composite
But from the point of view of functional, aesthetic and economic value, the last two types of inlays currently have value. And here we are in a convenient position to compare the inlay and filling from two angles. By comparing a filling and a ceramic inlay, it is convenient to evaluate the difference in structures created from materials with different functional qualities. And when comparing a filling and a composite inlay, let’s see how structures made from the same materials, but under different conditions, differ.
Ceramic inlays
It’s quite funny when, comparing a composite filling and a ceramic inlay, you sing odes in honor of the latter, but in fact, in the vast majority of cases, we work with a composite filling.
However, ceramic masses, no matter what they are, and inlays made from them are superior in functional qualities to composite fillings. And this is due not only to the qualities of the material, but also to the various manufacturing processes. When making a filling in the laboratory, the technician has privileges, such as significantly greater mobility during modeling. This is, of course, better to compare in the context of composite indirect restorations, however, computer modeling, which is increasingly being introduced into everyday routine practice, in theory should significantly increase the percentage of the use of ceramics when replacing defects in hard dental tissues.
The main difference between ceramics and composites is the greater strength of the former, which obviously leads to a longer service life of indirect restorations. Today, there are many works and articles indicating that modern ceramics are harder than natural tooth enamel, which in turn prevents the physiological wear of the restoration, contributes to the rapid wear of one’s own teeth, and increases the risk of chipping from such disharmonies. However, after their wear, composite fillings still remain on the teeth and do not cause inconvenience to the patient. It is good if a motivated and responsible patient regularly visits the dentist and the fillings are maintained in satisfactory condition, but the percentage of return patients is high. In this case, fillings of unsatisfactory quality lead to changes in the dental system. First compensated, then subcompensated, etc.
This may sound exaggerated, but it is reality. Modern composite fillings have excellent aesthetic and functional qualities, but require greater responsibility from the patient, while the higher cost of the inlays, and the very fact of a more advanced design in the patient, will stimulate him to be more conscious of the condition of his oral cavity.
Composite Tabs
As mentioned earlier, in this section it is useful to consider the differences between a filling and an indirect restoration, that is, a composite inlay.
So, current treatment concepts and modern filling materials make it possible to create excellent restorations, incredibly aesthetic, with high strength properties, but more than two decades ago the main reasons for the failure of composite restorations in the future were formed:
- Open dentinal tubules
- Polymerization shrinkage
- Under-polymerized composite
- Undercured dentin adhesive
- Increased occlusal contact
- Microbial contamination of the treated surface
- Microbial contamination during depressurization
- No binding agent
- Insufficient strength of dentin adhesive
- Gap in the area of the pulpal floor
- Crown crack
- Overdried dentin
- Open proximal contact
And if many of these points depend on the scrupulousness and responsibility of the doctor and the correct choice of materials, the rest can be quite significantly affected by the production of a composite restoration indirectly.
Making the inlay indirectly, as I said before, gives us greater mobility and ease of use, which is especially important when creating an adequate contact point between the teeth and the filling-tooth boundary. Literally, this is already the filling-plaster boundary, but this can be found in such a plus as good visualization of the boundary, and as a result the creation of a neat marginal fit. Thus, we have a greater opportunity to avoid at least two complications - depressurization and open proximal contact.
Next, by polymerizing the inlay indirectly, after a short exposure, we can remove the restoration and continue polymerization from different sides, or from all of them at once when using a photobox. This is important to reduce the degree of shrinkage, which in any case occurs, to avoid the C-factor and the risk of under-polymerization of the composite. In a quick calculation, we reduce the risk of such complications as polymerization shrinkage, under-cured composite, depressurization (a lower degree of shrinkage directly affects this) and a gap in the area of the pulp floor (caused by polymerization shrinkage).
On the one hand, it may seem that adhesive preparation for indirect restoration has a high risk of complications associated with under-polymerization of the adhesive and all the ensuing consequences, but that’s what modern lamps, powerful lamps and the doctor’s understanding of the manipulation he is performing are for.
By modeling the inlay using the indirect method, it is undoubtedly easier for the doctor to correctly recreate the anatomy, but it will most likely require correction after fixation. However, before this, the patient did not sit with us for some time with his mouth open while we modeled the filling for him, and therefore he does not have that fatigue in the joint, sprains, and we can more accurately correct the occlusal contacts. And just correct it, since when using articulators we had an excellent opportunity to create them exactly as we needed in a specific clinical situation.
As a result, we have that indirect restorations can seriously exceed fillings in quality, but the latter are still much more popular. Of course, the point is that it is more labor intensive, and the seemingly small increase in quality is not worth the extra effort.
But what if we could combine the advantages of filling speed, design quality of indirect restorations and material quality of ceramic restorations? Today, progress does not stand still and, again, is being increasingly introduced into everyday routine practice. I'll touch on this in the next section.
How the structure is made
Manufacturing methods and stages may differ slightly depending on whether the structure is solid or collapsible. In any case, preparation is required in the form of treatment and filling of canals, taking impressions. Next, in the laboratory, dental technicians carry out modeling and direct production of the microprosthesis. Below is a general description of how stump inlays are made:
- after administering anesthesia, the doctor expands the root canals, cleans and fills them,
- then takes impressions of the patient’s jaws and sends them to the laboratory,
- during the manufacture of a permanent structure, a temporary model, including one made of composite, can be fixed,
- the finished inlay is sent first for fitting, then for adjustment,
- As soon as the microprosthesis is completely ready, it will be fixed with cement in the root system. Then, immediately or after some time, a permanent crown will be fixed, or a composite build-up will be carried out.
Only until December 25 South Korean implant Osstem - from 18,500 rubles.
Hurry up to sign up for a free consultation and lock in promotional prices.
Call now or request a call
Opening hours: 24 hours a day - seven days a week
It should be taken into account that the nerve may first need to be removed. Treatment is carried out necessarily based on the results of an x-ray examination. At the same time, a collapsible design usually requires more fittings and, accordingly, frequent visits to a specialist.
Making a tab
Preparation for the manufacture of an inlay differs quite significantly from preparation for a composite direct restoration. We're not talking about a free cavity design. We need smooth, slightly diverging walls and a flat bottom, which can be leveled with a thin layer of restoration material. The angle between the walls and the bottom should be rounded to reduce stress on the material and hard tooth tissue in these areas. The cavity must be of sufficient size; weakened tooth tissues are excised to avoid further chipping. There are a huge number of these rules, which depend on the restoration material and the location of the defect, but there are the basic rules stated above. And the rest are determined by the doctor’s experience and the correct ability to assess the relevant clinical situation.
Next comes the impression. Modern materials make it possible to obtain two-layer one-stage prints of excellent quality, but this applies specifically to the materials. But with regards to modern technological solutions, we are taking a significantly different path and transferring the real state of affairs in the oral cavity into digital. To do this, we use intraoral optical scanners and the optical impressions they produce.
Next, we also model the inlay, pay special attention to the preparation border, proximal contacts, carefully check the occlusal contacts and remember the last century.
Today we will do it differently. Computer modeling will allow us not only to accurately model boundaries and contacts, but also to copy a tooth of the same name from the opposite side of the jaw, modify it to suit the situation in this area, create not just multiple occlusal contacts, but create them in the place we need, with the area and height required at micro levels. Yes, experienced doctors can do this with filling materials in the oral cavity, but not every one of us is a doctor with many decades of experience behind us. Moreover, ease of working with digital data and speed in working with digital data will definitely lead to a change in priorities in dentistry. Already leading. The modeled inlay is milled and sent to the office, or to the chair, since a milling machine in the office itself becomes commonplace.
If there are no such possibilities today, then we either polymerize the modeled composite inlay, or send a wax model of the inlay to replace it with ceramics.
Next, the tabs are fixed and the satisfied patient goes to stop chewing nuts.
When is this method contraindicated?
Prosthetics with this method are not performed in dentistry if the nerve is still alive. For such cases, traditional filling is recommended, which will help hide the aesthetic defect. Among other contraindications, experts identify the following conditions:
- the root is severely damaged and does not adhere well to the periodontium,
- the channels are not treated, inflammatory and purulent processes continue in them,
- the teeth are too loose, and it is no longer possible to fix them in one position, which means it is useless to install inlays,
- There is a pronounced recession of gingival and bone tissue around the affected element.
Don't know what type of prosthetics to choose?
We will help in the selection, advise where to read more information and compare types of prosthetics.
Consultation with an orthopedic doctor in Moscow clinics is free! Call now or request a call
Working hours: from 9:00 to 21:00 - seven days a week
You need to understand that the pin structure goes deep enough into the root. If the patient is intolerant to metals, an allergic reaction may occur. Therefore, it is better to take an allergy test in advance or choose an option made from a different material.
What is better to put under the crown: an inlay or a filling on a pin?
Sometimes the concept of “pin inlay for a crown and filling” is used. This is a wrong definition. It is understood as the usual restoration of a tooth using filling materials on a pin.
This is what the anchor pin looks like
Confusion is caused by the fact that some orthopedists cover the units restored on the pin with crowns and bridges. Although this is strictly forbidden, because... restoration materials cannot withstand the loads from prostheses and distribute them unevenly on the root system. This threatens:
- if the anchor pin falls out along with the filling and crown, you will have to throw out the old prosthesis and restore the tooth again;
- a root fracture - the unit will begin to hurt, wobble, and all that remains is to remove it.
But unscrupulous doctors still use prosthetic teeth with pins. They do this to reduce ongoing costs - not wanting to quarrel with a patient who has had a unit restored by the GP since a couple of weeks ago. But in the future, this approach will lead to big waste.
The only case when it is possible to cover a tooth with a pin with a crown is if at least 50% of your own tissue remains. But even with this option, most orthopedists prefer to restore the stump with an insert to ensure greater strength.
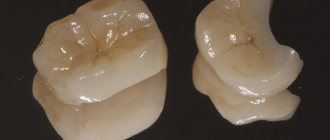
A metal inlay is installed under a metal-ceramic crown
Price
The stump model of the prosthesis is not a cheap dental structure. Its cost may vary from one dental office to another. The most inexpensive is the metal model (on average from 2,000 to 3,000 rubles). A prosthesis made of pressed ceramics costs about 12,000 rubles. And most of all you have to pay for the zirconium dioxide inlay (about 15,000 rubles).
If your tooth is damaged, but its root is not damaged, do not worry! Modern designs in the form of a stump tab will help you preserve and strengthen a hopeless tooth.
Sources used:
- I. Yu. Lebedenko, Orthopedic dentistry, 2012
- Seifollahi M. Preparation of lateral teeth for all-ceramic inlays
- https://medicine.wustl.edu/
Care after prosthetics
Caring for your teeth after installing a core prosthesis differs little from normal oral hygiene. This should include brushing your teeth twice daily. In this case, it is better to use a brush with soft bristles.
After each eating session, it is advisable to rinse your mouth with warm water, herbal infusions (chamomile, sage) or special ready-made mouth rinses.
To clean the interdental spaces, use floss or a brush.
It is advisable to visit a dentist every six months.
How the installation occurs - step-by-step description of the process
Before the installation procedure, it is important that the roots are properly healed and sealed. Typically, the remaining tissue from the visible part of the tooth is removed. Let's take a closer look at how the structure is put together in stages:
- after a detailed study of the x-ray image, the specialist unfills the canal by about half or slightly less than the length of the root - forms a small groove in which the tab will be fixed,
- Next, the doctor makes silicone impressions of both jaws - these will become the basis for recreating the exact anatomical shape of the product, so that the restored tooth can fit organically into the jaw system,
- The casts are sent to the laboratory. In the meantime, the doctor fixes a temporary prosthetic product to hide the aesthetic defect and prevent excessive gum growth,
- the finished product with its lower part is placed in the root system and fixed with dental cement. If it is dismountable and requires the installation of additional pins in the root canals, they are also covered with cement1. During the procedure, patients usually do not experience pain, because the nerve is removed, and all manipulations are performed under local anesthesia,
- At the final stage, an artificial crown is fixed to the stump. In this case, it serves as a support, just like a ground tooth if there is sufficient volume of its visible part.
Sometimes doctors incorrectly determine the optimal vector of treatment and decide to use pins to restore severely damaged elements. Such a mistake is fraught with fracture of the structure and the root. A natural consequence of this will be the need to completely remove the tooth along with the root system. After this, for a full recovery, an implant will have to be implanted.
Single-channel and multi-channel microprostheses
Stump inlays can be cast or with a split design. A one-piece product is manufactured under extreme temperatures and under high pressure. It is used to restore teeth with 1-2 canals. It is a single design – visible and in-channel.
A collapsible or multi-root system is created for molars with 3-4 canals. Once installed, it will not be possible to remove it. Like a solid cast one, such a microprosthesis is created using casts of the patients’ jaws, but usually requires more fittings.
Minuses
Like any other type of prosthesis, the stump tab has some disadvantages in technology and manufacturing time:
- High cost and longer production time (requires several visits to the orthodontist).
- Duration of treatment (preparatory stage for installing the “inlay + crown” complex after the second visit to a specialist).
- Cutting down a significant amount of bone and tissue for maximum docking during installation.