Dental implantation is a method of implanting a metal implant into the upper or lower jaw for further installation of a crown. This is the best method of prosthetics, which is used in leading dental clinics around the world. During the operation, the titanium rod is tightly fixed into the bone tissue, so that the specialist can use it to install a prosthesis or crown.
Currently, dental implantation is the only correct solution if you require:
- Installation of a prosthesis in the absence of 2-3 teeth in a row.
- Preservation of teeth during prosthetics (no grinding required).
- Restoration of all edentulous teeth.
- Replacement of teeth without the use of dentures due to allergies to the materials used.
In our clinic you can get a free dental consultation!
Our doctors
18 years of experience
Baghdasaryan
Armen Evgenievich
Chief physician, dentist-orthopedist-therapist
Graduated from VSMA named after. N.N. Burdenko. Internship on the basis of MGMSU named after. A.E. Evdokimov in “General Dentistry”.
Clinical residency at the Moscow State Medical University named after. A.E. Evdokimov in “Orthopedics”.
More about the doctor...
5 years experience
Sadina
Ekaterina Vladislavovna
Dental therapist, surgeon
Penza State University Medical Institute, specialty “Dentistry”.
In 2021, she underwent professional retraining in the specialty “Therapeutic Dentistry” at the Moscow State Medical and Dental University named after A.I. Evdokimov.
More about the doctor...
8 years of experience
Arzumanov
Andranik Arkadievich
Dentist-orthodontist
Graduated from Moscow State Medical University. Internship - Moscow State Medical University at the Department of Orthodontics and Children's Prosthetics.
Residency at Moscow State Medical University at the Department of Orthodontics and Children's Prosthetics. Member of the Professional Society of Orthodontists of Russia since 2010.
More about the doctor...
First meeting
The clinical examination begins with questioning the patient. Complaints, medical history, duration and cause of tooth damage are clarified. The patient’s past illnesses and surgical interventions, allergy status, bad habits and other life circumstances are established. Particular attention is paid to determining psycho-emotional status. The latter includes the identification and correction of asthenic, anxious, hypochondriacal and hysterical types of reaction.
The study of dental status begins with an external examination of the face, the condition of the oral mucosa: color, moisture, presence of bleeding, desquamation of the epithelium, ulcers, atrophic or hyperplastic processes. The depth of the periodontal pockets and the manifestation of discharge from them are determined. The presence of hard dental plaque and soft plaque is detected.
A special probe is used to determine the thickness and type of mucous membrane and gum attachment. A dental examination includes the identification of caries and its complications, non-carious lesions of hard tissues, assessment of the stability of the teeth, their relative position, as well as the type of bite. The condition of the tongue, the function of the salivary glands, the degree of mouth opening, and the severity of fatty tissue in soft tissues are checked. A complete sanitation of the oral cavity is carried out and the patient is trained in hygienic skills for oral care.
How is dental implantation planning carried out?
Before the operation, you need to undergo diagnostics and all preparatory procedures:
- Visit a therapist for a comprehensive medical examination and to rule out contraindications.
- During the consultation in advance, clarify allergies and intolerances to painkillers, anti-inflammatory drugs and antibiotics.
- Get an orthopantomogram (panoramic photo of your teeth).
- Take an impression of the jaw and develop a plaster model in the laboratory.
- Conduct an in-depth analysis of the plaster model to determine the position of the implant.
Without fail, the dental surgeon answers all the client’s questions and talks in detail about the operation and the rehabilitation period.
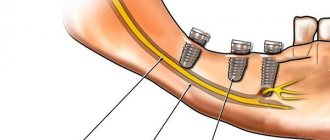
CBCT planning of immediate implant procedures
The implantation procedure requires careful planning of all stages of the surgical intervention to achieve successful osseointegration and further prosthetic rehabilitation of patients. X-ray methods for studying the dentofacial apparatus, including intraoral and panoramic radiography, as well as cephalometry, are now mandatory tools for a dentist planning implantation. However, the nature of such images is two-dimensional, therefore, on their own, they can only provide the ability to assess the mesial-distal and occlusal-apical parameters of the bone bed. But for successful planning, it is simply impossible to do without knowledge of additional vestibulo-lingual parameters of the residual ridge, not to mention the need to assess the level of its inclination.
In addition, panoramic radiographs have been shown to provoke overestimation of implant parameters during planning due to the magnification effect of the imaging process. A similar effect can subsequently provoke injury to adjacent anatomical structures (for example, the floor of the maxillary sinus or the inferior alveolar nerve) during surgical manipulation. So, no matter how hard you try, graphic distortions and the overlap of anatomical objects on one another simply cannot be avoided during planimetric radiography; therefore, to increase the accuracy of the diagnostic stage, it is recommended to use more advanced methods, for example, computed tomography.
Benefits of cone beam computed tomography
Cone beam computed tomography (CBCT) is a reliable tool for clinicians to plan and monitor the dental implant process. This method allows doctors not only to determine the most suitable place to install an implant without the need for additional augmentation, but also to select an implant design of the appropriate size and shape. In addition, the doctor can accurately select the required angle for installing the intraosseous support depending on the morphology, height and density of the surrounding bone tissue. In turn, this will help to avoid such complications as damage to the inferior alveolar nerve, taking into account the proximity of the latter to the lingual concavity in the distal parts of the lower jaw. Research findings indicate that the use of CBCT to assess bone density can help predict future structural stability, not to mention that CBCT can be useful for position confirmation and assessment of osseointegration postoperatively.
Historically, although doctors used CBCT for implant planning, the production of guide templates was carried out manually by dental technicians from plastics with different polymerization mechanisms. Consequently, the possibility of integrating the parameters of prosthetic rehabilitation and implant installation digitally was out of the question. Nowadays, this problem has been completely resolved, and doctors successfully use so-called fiducial markers to compare the parameters of the surgical and orthopedic phases during complex dental rehabilitation. Thus, it was possible to translate manually made guide templates into three-dimensional space in order to further use them during the surgical and orthopedic stages of treatment.
Although CBCT imaging helps to increase the accuracy of planning the procedure for immediate loading of implants, but when using templates made by a dental technician, this accuracy is leveled due to non-precision determination of the depth of insertion of the infrastructure, increased duration of the manipulation, poor visibility of the surgical field, and inconsistency with templates made using CT data -scanning. But based on modern software, it is possible to develop patient-oriented templates, which can additionally be compared with X-ray data, and thus ensure maximum accuracy of future iatrogenic interventions. In addition, modern methods for making templates allow the doctor to choose the type of their fixation depending on the specific clinical situation: supported on bone tissue or supported on teeth. It should not be forgotten that surgical templates modeled using computer software are more reliable in terms of compliance with the desired position and accuracy of placement of the titanium element. This approach helps not only to save time, but also to simplify the implantation procedure itself, as well as provide more complete visualization of the working field during surgery.
Despite all the above advantages of CBCT, choosing an adequate implant for each clinical situation is a rather difficult task for the implantologist. After all, the accuracy of the abutment fit, the rotational interaction of the elements, the level of contact at the interface with the bone tissue in the crestal region, the amount of pressure on the cortical part of the ridge, the stability of the future restoration, as well as its general future prognosis depend on the infraconstruction. The use of implants with an internal hex connection provides a better relationship between the implant and the abutment, minimizing the effect of micromovement and bone resorption, while microthreading in the neck area allows for an increase in the contact area with the surrounding structure of the residual ridge. The combined use of an implant of adequate diameter, a surgical template and modern technologies allows us to achieve the most reliable and predictable results of complex dental treatment.
Clinical case
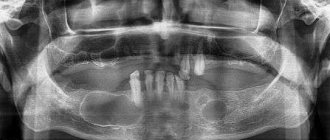
A 60-year-old man with edentulous symptoms sought dental care for problems chewing food (Figures 1 - 2). The patient expressed a desire to restore existing defects using permanent structures supported by dental implants. In the area of the lower jaw, a partial defect in the dentition was discovered, as well as his own frontal teeth, which could not be restored (photo 3).
Photo 1. View before treatment.
Photo 2. Side view: signs of loss of bite height.
Photo 3. View of the lower jaw teeth that cannot be restored.
As a result of the existing pathology, the patient also experienced a loss of bite height. After a clinical examination and X-ray examination, a future treatment plan was developed, which included extraction of existing teeth, immediate implantation, and fixation of provisional structures in one visit. Given the parameters of the residual bone crest, as well as bone density and a favorable general medical history, the patient was an ideal candidate for an immediate implantation procedure (Figure 4).
Photo 4. Orthopantomogram before implantation.
After recording the primary parameters of occlusion, determining the centric relation and vertical parameters of the bite, as well as analyzing the results of the facial arch recording and evaluating the impressions obtained, it was decided to install implants in place of the first molars, first premolars and canines on both sides of the jaw. This approach will help to achieve the correct distribution of occlusal load (photos 5 - 6).
Photo 5. Analysis of CBCT images for planning the position of implants.
Photo 6. The ability to analyze CBCT allows you to plan the position of the implants that would be most advantageous in terms of occlusal load distribution.
A CLC scanner (CS 9300, Carestream) was used to plan the position of the implants, taking into account the available bone density parameters for immediate implantation (Figure 7). Based on the CBCT data, a CAD/CAM analysis was also performed (photo and a surgical template was made (MGUIDE, MIS) (photos 9 - 10).
Based on the CBCT data, a CAD/CAM analysis was also performed (photo and a surgical template was made (MGUIDE, MIS) (photos 9 - 10).
Photo 7. Possibility of taking into account many parameters when planning implantation with CBCT.
Photo 8. Rendering of the obtained CBCT sections.
Photo 9. CAD/CAM analysis for modeling a surgical template.
Photo 10. Virtual model and visualization of the position and inclination of the implants.
After determining the position of the implants, diagnostic impressions from A-silicone were analyzed, as well as the resulting models, which were subsequently sent to the laboratory (MCENTER, MIS) for the production of a guide surgical template supported by bone tissue. After clarifying the positions and inclination of future structures and appropriate modification of the template, it was sent to the clinic before implantation began. To achieve greater accuracy, the studied models were fixed in a semi-adjustable articulator (SAM3, Great Lakes Orthodontics).
Installation of implants
After the usual preparation of the surgical field and premedication, the surgical procedure was started by administering local anesthesia (3% mepivacaine, 2 capsules on both sides of the jaw, and 1 capsule of 3% marcaine with epinephrine 1:100,000 to infiltrate the mental foramen area). The surgical template was then inspected in the mouth (Figure 11), after which the implantation procedure began without soft tissue flap separation (MIS SEVEN implants, MIS Implants Technologies Inc). First, implants were installed in the area of 19 and 30 teeth, after which 22 and 27 teeth were removed and infrastructures were installed in place of teeth 22, 26-28. At the end, the premolars (teeth 20 and 21) were extracted, and implants were immediately installed in their place.
Primary stability of all implants was achieved up to a torque value of 55 N*cm, except for the area of 22-27 teeth, where the torque value did not exceed 35 N*cm. To augment the implantation sites, a mineralized corticocancellous allograft (Rocky Mountain Tissue Bank) was used. After installation, multi-unit abutments were fixed to the infrastructure. During immediate loading of the supports, temporary cylinders (Figure 12) and a screw-retained provisional prosthesis were used (Figure 13). The adequacy of implant placement was verified radiographically. It took 4 months to achieve complete healing of the intervention area, during which the final fixed zirconium prosthesis (Prettau Zirconia, Zirkonzahn USA Inc) was made. Fixation of the final structure was carried out 16 weeks after the primary intervention, the adequacy of fixation was checked using an x-ray method, after which the necessary occlusion correction was carried out (photos 14 - 15).
Photo 11. Trying on a surgical template.
Photo 12. Installation of temporary cylinders.
Photo 13. Loading of implants using a provisional prosthesis.
Photo 14. View after fixation of the final superstructure.
Photo 15. View of the final zirconia restoration.
conclusions
The use of CBCT will not only determine the parameters of the height, width and bone density of the residual crest, but also, in contrast to conventional X-ray diagnostic methods, allows for the most adequate and accurate planning of future iatrogenic intervention, which is extremely important when implementing the immediate implantation approach. The combined use of topographic scans as well as surgical guides helps clinicians achieve the most effective and predictable outcome in the complex rehabilitation of dental patients.
Author: Datta Malyavantham, BDS, DDS, FICOI
Medication support for dental implantation
It is important after the operation to follow all the specialist’s recommendations and take prescribed medications. After implantation, anti-inflammatory, antibacterial, and antihistamine drugs are prescribed. Among them are Chlorhexidine, Nimesil, Serrata, Amoxil. It is necessary to strictly follow all the recommendations of the attending physician in order to speed up regeneration, relieve inflammation and pain.
Additionally assigned:
- Rinsing the surgical area with an antiseptic.
- Applying ice.
- Eating only soft and mushy foods.
- Treatment of gums with antiseptic pastes.
- Cleaning teeth and gums with a soft brush and floss.
Indications for dental implantation
- Replacement of one or more teeth in a row.
- Jaw prosthetics for edentulous patients.
- Installation of outer teeth (fixation of the prosthesis is impossible due to lack of support).
- Allergy to the material from which dentures are made.
- Pain syndrome due to lack of functional occlusion.
Implantation is strictly not recommended in case of curvature or significant darkening of the enamel. There are many treatment methods that eliminate pathology 100% and allow you to maintain healthy teeth.
What's the difference in price?
The difference in price is the cost of producing radiopaque and implantation templates. For assessment, for one jaw, regardless of the number of implants installed, you will need to pay an additional 26,000 rubles. to the planned cost of the implantation operation. Often, when it comes to a simple case of installing a single implant, we can do without making templates. An implantological template is used when installing 2 or more implants, then the price increase will be 13,000 per implant. If there are even more implants, the cost of the template ceases to play a significant role in the price of treatment.
Trust the beauty of your smile to professionals
Dentistry in Lyublino “Good Hands” has been operating on the Moscow market for more than 5 years and has earned a huge number of positive reviews from regular customers. We carry out:
- Comprehensive diagnostics.
- Taking impressions and creating a plaster model.
- Selection and installation of implants.
- Monitoring results and assistance in the rehabilitation process.
We use the best implants from manufacturers from Switzerland, Germany, and Israel. To make an appointment for diagnostics, call us during business hours.
Toilet bone wound
Curettage of a bone wound is indicated only if granulating periodontitis is detected or the presence of a fibrous formation or granuloma at the apex of the tooth root. Use a curettage spoon with extreme caution. It is necessary to especially carefully evacuate the mucous membrane that has grown into the root cavity due to the inflammatory process. Granulations, if they are found in the inner surface of the gum edge, are also thoroughly cleaned. The hole must be disinfected. For disinfection, an antiseptic solution of gentamicin, chlorhexidine or saline solution (9%) is used.
The choice of implant size occurs after measuring the root diameter at different levels. Implant selection criteria (see photo 12):
- the length of the implant should be 2-5 mm longer than the hole;
- width - 1-2 mm larger than the hole.