1.General information
In otorhinolaryngology, a separate group of pathological conditions is distinguished, which are based on the expansion of the paranasal sinuses (paranasal sinuses). Such cystic cavities form, as a rule, slowly, asymptomatically or with few symptoms, and are gradually filled with one or another content. Thus, a sealed cystic expansion of the paranasal sinus filled with serous fluid is called a hydrocele, mucous contents are called mucoceles, and purulent masses are called pyoceles.
The absolute majority of such anomalies are observed in the frontal sinuses: the mucocele and pyocele of the frontal sinuses together account for at least 80% of the total volume of diagnosed pathological changes of this kind. In second place (about 15%) are expansions of the ethmoidal (ethmoidal) sinus, and the remaining insignificant share is accounted for by expansions of the sphenoidal (sphenoid) and maxillary (maxillary, maxillary) sinuses. The last three options are not considered here, although the mechanisms of formation and the clinical picture are largely similar; in addition, with a long course and thinning of the bone partitions, the cyst-forming process spreads from one sinus to another.
Most often, the formation of a mucocele (pyocele) of the frontal sinus begins at school age and continues for several years before subjective discomfort becomes significant enough to contact an ENT doctor and prescribe an appropriate examination.
A must read! Help with treatment and hospitalization!
Mucocele in the maxillary sinus
According to the pathogenetic classification, all cystic lesions of the paranasal sinuses can be divided into three forms: retention cysts, meningocele and mucocele. Retention cysts are the most common form, the localization of which is usually strictly limited. Meningocele is a hernial protrusion of the meninges that occurs due to the pathological development of the fetal skull. Mucocele is a benign, expansive cyst-like formation filled with mucus and lined with respiratory epithelium of the paranasal sinuses. Mucocele grows slowly and is locally aggressive.
Photo 1. Orthopantomogram
It is believed that a mucocele may cause obstruction of the opening connecting the sinus to the nasal cavity, which leads to the accumulation of fluid. Gradually, producing mucus, the mucocele increases in size and deforms the surrounding bone. The most common causes of mucoceles are chronic infections, allergic diseases, trauma and previous surgical interventions, while the causes of some remain unknown.
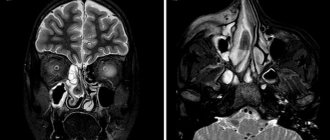
Figure 2: CT scan showing a mass in the left maxillary sinus.
Figure 3. Axial view of MRI showing a mass in the left maxillary sinus.
Most mucoceles are localized in the frontal sinus (60%), followed by the ethmoid sinus (30%) and maxillary sinus (10%). Location in the sphenoid sinus is considered very rare. Despite the fact that this formation is benign, a mucocele in the maxillary sinus can grow to large sizes and cause bone destruction. The symptoms manifested are mainly associated with compression of surrounding tissues. The addition of a secondary infection can lead to aggravation of the condition and cause complications, especially in the orbital area.
Photo 4. Aspiration fluid
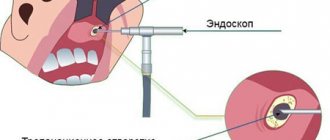
CT is the principal diagnostic method. CT and MRI images allow the specialist to accurately assess the location of the formation. The traditional method of treatment is excision or enucleation using endoscopic intranasal access.
The purpose of this report is to demonstrate a large mucocele of the maxillary sinus, which is considered rare in patients without previous ENT pathologies. The cyst was enucleated using the Caldwell-Luc method.
Description of a clinical case.
A 39-year-old man with a large mass in the left maxillary sinus, asymptomatic, was referred to the Department of Maxillofacial Surgery. The formation was discovered during an X-ray examination. The patient denies any history of trauma, allergic diseases, or interventions on the paranasal sinuses. The patient has an unremarkable medical history, does not take medications, and is a smoker.
Examination of the oral cavity was unremarkable, with the exception of palpable swelling along the buccal sulcus. X-ray and CT scan showed a homogeneous mass filling the left maxillary sinus (Figures 1,2). Approximate size 5x5 cm.
A puncture of the formation was performed under local anesthesia. A light yellowish fluid was aspirated from the mass. After this, the Caldwell-Luke operation was performed, the left maxillary sinus was cleaned and examined (Photo 4,5). Histopathological examination identified the mass as a mucocele. The recovery process was uneventful in a short period. The patient is under the supervision of specialists.
Photo 5. During surgery
Discussion.
The term mucocele was introduced by Rollet in 1896, and the first histological description was made by Onodi in 1901. The most common location of mucocele is in the frontal sinus, somewhat less commonly in the ethmoid and sphenoid. In the maxillary sinus, mucocele also occurs very rarely, about 10% of cases. The symptoms manifested are mainly associated with compression of surrounding tissues. Mucoceles of the frontal and ethmoid sinuses are often associated with headaches and sometimes blurred vision. A mass in the maxillary sinus usually causes symptoms of obstruction and visual defect. Mucoceles are considered benign formations, however, they can have a detrimental effect on the surrounding vital structures of the orbit and skull. In addition, conditions such as sinusitis, nasal congestion and anosmia appear. Although the patient in question had a large mucocele, he was completely asymptomatic.
Differential diagnosis presents certain difficulties. In the absence of bone erosion, mucoceles are distinguished from retention cysts, sinusitis and polyposis of the paranasal sinuses. In cases where bone damage is extensive, it should be differentiated from malignant conditions: spinocellular carcinoma, cystadenocarcinoma, plasmacytoma, melanocarcinoma, schwannoma and tumors of odontogenic origin.
CT scans in axial and direct projections are the optimal method for detecting mucoceles. The sinus is usually darkened, dilated and with damage to the bone walls. The sinus cavity is filled with fluid and soft tissue. It is preferable to perform CT images; MRI can be useful in controversial conditions to determine fluid or tissue in the lumen. In our case, CT showed a homogeneous formation completely filling the maxillary sinus.
Treatment traditionally consists of enucleation or enucleation of the cyst through an external approach. However, Blackwell in 1993 described a successful intervention using an endoscopic technique for antrostomy of the maxilla. Since then, endoscopic techniques have been increasingly developed, and a method of access through the lower nasal meatus has now been described. After surgery, the sinus configuration may remain unchanged, improve slightly, or return to normal. Nkenke suggests evaluating results at least 2 months after the intervention, as he considers this period necessary for recovery. External access involves tissue dissection, sinusotomy and mucocele removal. In our case, the Caldwell-Luc method was used under local anesthesia.
Conclusion.
Mucoceles in the maxillary sinus are considered rare. The present case describes a large mucocele in the maxillary sinus of a patient who had no history of any complaints or problems with ENT organs. The treatment was surgical, Caldwell-Luc surgery. Recovery was uneventful with a short follow-up period.
Authors:
Fidevs Akpek, Researcher, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Abant Izzet Baysal University, Bolu, Turkey
Ismail Akkas, Assistant Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Abant Izzet Baysal University, Bolu, Turkey
Orcum TOPTAS, Assistant Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Abant Izzet Baysal University, Bolu, Turkey
Fatih Ozan, Associate Professor, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Abant Izzet Baysal University, Bolu, Turkey
2. Reasons
The immediate cause of muco/pyocele is mechanical bursting pressure on the walls of the frontal sinus from the inside, from accumulated mucous or purulent masses. If this situation continues long enough, the bone walls begin to thin and become deformed in the direction of stretching.
In turn, a complete or partial blockage (obstruction, obliteration, obstruction) of the canal connecting the sinus with the nasopharyngeal cavity leads to the accumulation of contents. This is facilitated by fibrosing processes - tissue degeneration, stenosis and the formation of adhesions during chronic inflammation, scarring after injuries, etc. Less commonly, the cause is polyposis, a tumor, or severe curvature of the nasal septum.
Infection, if it occurs, is caused by the same mechanisms that lead to the development of frontal sinusitis: the spread of infection from the affected nasopharynx, neighboring sinuses, other adjacent structures, or the penetration of a pathogen through the blood or lymph.
Visit our Otolaryngology (ENT) page
Signs
Quite often, cysts of the paranasal sinuses do not manifest themselves for a very long time, until they reach gigantic sizes, occupying all the free space. A person may be bothered by:
- headache for no apparent reason, has no pattern and cannot be treated with painkillers;
- a feeling of pressure on the eyes, strange discomfort in the upper jaw;
- an unpleasant feeling of mucus running down the throat (mucus flows down the back of the throat);
- smell disorders - occur with a cyst of the sphenoid sinus,
- the release of a clear, light-colored liquid without any admixture of pus or blood during spontaneous rupture and emptying of the cyst.
When a cyst occurs, the emptying of the sinuses may be disrupted, reducing their natural cleansing ability. Then inflammation occurs, which is manifested by constant nasal discharge, increased headaches, the appearance of an unpleasant odor, increased body temperature, and the development of chronic sinusitis.
In the presence of a cyst, allergic manifestations are more severe, losing their seasonality and turning into a permanent problem.
Nasal breathing is rarely difficult, only when the cyst enters the nasal cavity or is inflamed.
Computed tomography of the sinuses
- Cost: 5,000 rub.
More details
Odontogenic cysts have unpleasant manifestations. There is lacrimation, swelling, and acute pain similar to neuralgia. If the cyst suppurates, signs of general intoxication appear: fever, severe headache, nausea or vomiting, loss of appetite, weakness.
3. Symptoms and diagnosis
Between the actual onset of bone deformation and the appearance of tangible manifest symptoms, it can take from a year to 5-6 years or more.
As a rule, the patient pays attention to frequent headaches of a pulling, dull, aching nature, localized in the frontal lobes, less often radiating to the bridge of the nose or temples. Then periorbital pain occurs, deformation of facial proportions becomes noticeable, and a gradually growing bulge appears in the corner of the eye. Palpation examination of this protrusion is usually accompanied by crepitus (dry rustling, parchment crunch). With further progression, exophthalmos is formed, the eyeball also moves downward, visual disturbances appear and increase, which, in the absence of adequate help at this stage, can result in severe complications up to atrophy of the optic nerve head, retinal detachment and loss of vision in the affected eye.
Further accumulation of contents in the muco(pio)cele can lead to the formation of a fistula and the spread of the infectious and inflammatory process to adjacent cavities and structures. The consequences of this can be the most severe - meningoencephalitis, panophthalmitis, periorbital cellulitis (orbital cellulitis), etc.
When contacting in the early stages, such mandatory diagnostic procedures as analysis of complaints, careful history taking and standard examination of ENT organs (rhinoscopy, otoscopy, etc.) may not be enough. Of the instrumental studies, the most informative are radiography, ultrasound, tomography (CT or MRI); Sometimes probing or puncture of the frontal sinus is indicated.
Consultation and examination with related specialists is almost always necessary - first of all, with an ophthalmologist, and also, if indicated, with a neurologist, oncologist, etc.
About our clinic Chistye Prudy metro station Medintercom page!
4.Treatment
It is easy to see that there are no conservative methods for eliminating muco/pyocele of the frontal sinus. Even forced complete drainage of the sinus does not reconstruct the normal anatomy of the bony cranial structures. Therefore, in all cases, the question is raised about frontotomy (opening the frontal sinus) with evacuation of the contents, sanitation of the surgical field, restoration of normal sinus ventilation and, if indicated, plastic surgery. The operation is performed under powerful antibiotic, anti-inflammatory and decongestant cover, drainage is left until the surgical wound is completely healed and scarred.
The prognosis is favorable in the absence of serious complications (see above), which require the use of separate, sometimes emergency care protocols.
How can mycetoma be cured?
Is it possible to do without surgery? It is impossible to get rid of fungus in the maxillary sinus without surgical intervention, I will say this right away. No pills, no drops of “dancing with a tambourine” and everything else will give the desired therapeutic effect. First of all, it is necessary to surgically remove the fungal body, remove this mycelium, remove all the fungus from the maxillary sinus.
This can be done either through a nasal surgical approach or an intraoral approach.
How to remove fungus from the maxillary sinus
With intraoral access, a perforation is made in the vestibular wall of the maxillary sinus - access, and evacuation occurs through this hole, i.e. removal of the fungal body, mushroom mycelium. Then the maxillary sinus is well washed, treated with antifungal and antimicrobial drugs and sutured. Subsequently, the patient is prescribed antifungal therapy.
Surgical removal of mycetoma shows good results today, relapses are extremely rare.