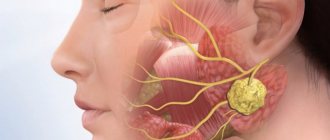
Tooth nerve and indications for its removal
The dental nerve is its main organ, located at the root - the pulp. It is a system of blood vessels and is responsible for the reaction to stimuli. When it is completely removed, the tooth is considered “dead” because its blood supply is cut off. As a result, the enamel darkens, the tooth loses its resistance to irritants and quickly collapses. If, as a result of caries, the dental nerve is damaged - pulpitis - the question arises of complete or partial amputation of the pulp. When pulpitis progresses to the stage of periodontitis, removal becomes inevitable. Indications for removal also include destruction of bone tissue, a wide area affected by caries, persistent toothache.
Consequences of nerve removal
In the first 1–2 days after treatment, the tooth may hurt, but the intensity of the pain gradually decreases. To alleviate the condition, you can take analgesics recommended by a specialist. There are no other consequences of nerve removal.
Since pulpitis is most often caused by caries, during the treatment process the dentist removes the affected crown tissue. Restoring the integrity of the tooth is performed after removing the temporary filling. For correction, a filling material that does not contain toxic substances is used. In some cases, when the area of the carious cavity is too large and there is a risk of the filling falling out, it is recommended to install prostheses (stump or artificial crown.
Many parents mistakenly believe that depulpation implies the absence of a nerve in a permanent tooth. However, this is not at all true. Temporary and permanent teeth have separate systems and tissues that are not interconnected.
Martinka Children's and Adolescent Dentistry treats pulpitis by removing the nerve. Timely and correctly performed removal of the nerve of a baby tooth has no consequences. The integrity of the tooth is restored, and its functionality is preserved.
Removing dental nerve using arsenic
Previously, dental nerve amputation procedures were performed using arsenic. The root canal was enlarged using a drill, then arsenic was applied to the pulp and closed with a temporary filling to “kill” the nerve. The process took 2 days and was accompanied by pain, which could not be suppressed even with the help of analgesics. After the expiration of the period, the temporary filling had to be removed, the nerve removed and the root canal cleaned. The whole procedure was very painful and lengthy, requiring visits to the doctor several times. The main disadvantage of this method is the use of arsenic, known for its strong toxic properties. Both the doctor and the patient had to be extremely careful when using this substance in treatment, because if arsenic remained in a person’s tooth for longer than the permitted period, this led to tissue destruction and even tooth loss. For these reasons, today arsenic is no longer used in medical practice, but new techniques for amputating the nerve of a tooth are being successfully introduced.
Modern treatment of pulpitis without the use of arsenic
Patient K. came to the clinic with complaints of severe pain in the gums in the area of the 47th tooth. The tooth was treated 3 days ago in the self-supporting department of the district clinic for chronic pulpitis.
| PHOTO 1: Visible devitalizing material at the mouth of the root canal and necrotic gums between the teeth against the background of inflamed soft tissues. | PHOTO 2: On the day of contacting our clinic, the canals were processed and sealed, the gums were treated, and a sealed temporary filling was placed (see x-ray). |
| PHOTO 3: Photo after 1 week: inflammation of the gums and soft tissues has been eliminated. | PHOTO 4: a month later, the tooth was completely restored with a ceramic inlay. |
For reference: Treatment methods for pulpitis differ in the method of anesthetizing the pulp. If devitalizing pastes (paraformaldehyde, paste with arsenic, etc.) are used to “kill the nerve,” then the methods are called devitalizing. And if the treatment takes place under anesthesia and without the use of drugs that kill the pulp, then such methods are called vital.
Everyone knows that arsenic is a poison. But it can be used for peaceful purposes. And the older generation probably remembers that arsenic was previously used by dentists to “kill the nerve.” At the same time, with arsenic in the tooth, it was under no circumstances possible to “walk” for more than the appointed time. Why was it used?
To treat pulpitis (inflammation of the “nerve”), the dental pulp must be removed and the cleaned canals of the tooth must be sealed. Since previously anesthetics were not “strong” enough, and the instruments for working in the canals were not thin and flexible enough, the dentist used arsenic to be on the safe side, so that there would be no pain in the tooth during or after the manipulation.
And even then the terms “arsenic periodontitis” and “arsenic periodontitis” arose, and scary pictures appeared in dental textbooks illustrating complications caused by the use of arsenic, such as osteomyelitis and mediastenitis. Every dental office even had an antidote - unithiol in case of an overdose of the drug.
It would seem that everything is in the past. But the incident with which I began the story happened the other day. The photograph (PHOTO 1) shows a “dead” gum.
In order to treat chronic pulpitis, the dentist at the district clinic applied a devitalizing agent (one of the most popular in our time) to the patient’s pulp of the 47th tooth, after which he installed a temporary filling. And on the third day the patient came to me complaining of pain in her gums. The material for the temporary filling turned out to be insufficiently airtight, and the toxic drug “leaked” into the gum, causing necrosis and inflammation of the surrounding tissues. The final consequences will become clear after some time and will depend on whether the toxic drug has had time to act on the jaw bone.
Currently, devitalizing agents (literally can be translated as “depriving life”) contain paraformaldehyde instead of arsenic, the toxic effect of which “poisons” the pulp and leads to its death. But if the drug turns out to be more than required, then in addition to the pulp, other tissues surrounding the tooth will be poisoned. And as a result, toxic periodontitis will develop.
The annotation for such a drug does not indicate exactly how much of the substance to use in a particular case. The manufacturers vaguely wrote: “at the discretion of the doctor.” As a doctor, I understand that every living organism is individual, so a safe amount of a product for one patient may be toxic for another. This depends on many factors: the stage of pulp inflammation, the volume of pulp tissue, the shape of the canal and the age of the patient, etc.
There is a high probability of error when using devitalizing agents.
But the main thing is: why use a potentially dangerous technique?
After all, a modern doctor has a wide arsenal of tools, tools and methods for the safe treatment of pulpitis. The choice of anesthetics allows one or another to achieve anesthesia in any patient; nickel-titanium instruments allow one to climb into curved canals and clean out the pulp under microscopic control, and rinsing the canals with antiseptics dissolves the remaining living tissue inside the canal and neutralizes microorganisms.
If a dentist uses modern techniques, why should he return to devitalizing agents?!
I admit only one reason for using a devitalizing drug - lack of time for the doctor or patient to fully treat the canals during that visit. Fortunately, these are isolated cases in practice.
The author of the article is dentist-therapist Stefanskaya V.V.
How to remove the nerve of a tooth today
Today it has become possible to remove the dental nerve by visiting the dentist just once. Depending on the diagnosis, the nerve is removed completely or partially.
- Complete removal. It is performed under anesthesia. After an anesthetic injection, the doctor removes the affected dental tissue and extracts the pulp with a special tool. The procedure lasts on average half an hour. If the depulpation process was controlled using a microscope, the dental canals and the tooth itself are thoroughly filled after the procedure. Sometimes the dentist first places a temporary filling, and then, after making sure that the procedure was completed successfully, changes it to a permanent one.
- Partial removal. It is carried out when only the coronal part of the pulp is affected. The root is preserved, and the inflamed tissue is removed. If the nerve is partially amputated, tooth decay does not occur as quickly. Therefore, this method is recommended for carious disease of molars in children.
When is depulpation performed before prosthetics?
Until recently, nerve removal was a routine process before the installation of permanent structures. Recently, the views of dentists have changed. The fact is that a tooth without pulp is considered “dead”. There is no tissue exchange, secondary dentin is not produced. He becomes fragile. In addition, when there is no pulp, the inflammatory process can completely destroy the tooth, because there will be no pain for a long time.
On the other hand, if the pulp becomes inflamed under the crown, then an expensive and complex restoration will have to be removed in order to carry out treatment.
There is no consensus among dentists whether it is necessary to remove the nerve during prosthetics. Each point of view has its defenders and opponents. The golden rule of dentistry is to carry out manipulations strictly according to indications.
Causes of toothache after nerve removal procedure
It happens that after depulpation, patients complain of pain in the tooth. Most often, this pain is temporary and is explained by surgery and blocked with analgesics. It is caused by eating cold or hot food and jaw movements. After a couple of days, such pain goes away. But if it was not possible to remove the nerve completely or the root canal was poorly cleaned, inflammation and pain return. In rare cases, the cause of pain is an allergic reaction to the filling material. All this can lead to complications and even tooth loss, so if you have complaints, you should not postpone a visit to the doctor.
Without a doubt, removing the dental nerve is a very unpleasant and frightening procedure, but often it is simply necessary in order to save the tooth. Today, this service is provided by many clinics in which qualified doctors will carry out all the necessary manipulations efficiently and as painlessly as possible.
Complications
The most common complications after nerve removal before replacement are pain and swelling. Normally, these symptoms go away within a day at most. If the pain does not go away, intensifies, or swelling does not subside, you need to consult a doctor. He will conduct diagnostics to identify the causes. It could be:
- Poor quality channel cleaning
. An incorrectly chosen length of the tool does not allow you to go through the canal to the end. Remains of pulp cause inflammation - residual pulpitis. - Root canal perforation
. Through the destroyed apex, the infection penetrates into the periodontium (tissue around the tooth), causing pain. - Missing tooth canals
. All canals are not always visible on the image, and this is the only source of information for the dentist. The remaining pulp becomes inflamed, causing discomfort. - Tooth fracture
. If the anatomical shape of a tooth is not restored immediately, it may break. - Violation of sealing technology
. This may be incorrect proportions for mixing the composition or the filling material getting on soft tissues.
Sometimes, after endodontic treatment, the tooth darkens. Without pulp, no food is supplied to the tooth, and cells are not renewed. Dentin dries out and its color darkens. Another reason is that the enamel becomes porous and pigments penetrate through it more easily. Sometimes, the tooth darkens due to hemorrhage when the nerve is removed before prosthetics.
Don't be afraid, it's not dangerous. The denture will provide a protective barrier and hide discoloration.