Short frenulum of the tongue - parents encounter this problem around the time their baby turns 3-4 years old. He has been trying to speak for a long time, knows a lot of words, knows how to construct complex phrases, but does not pronounce some words accurately.
Grandmothers assure that in another year the child will “speak out”; mothers work with their children using special methods for early development, but the problem is not solved. If your child is still babbling at 4 years old, it is time to visit the pediatric dentist.
The frenulum of the tongue externally resembles a thin membrane, consisting mainly of connective tissue, the function of which is to attach the tongue to the bottom of the oral cavity.
In other words, a short frenulum of the tongue in a child is some kind of defect in the oral cavity that interferes with the joint movement of the tongue.
In some cases, the frenulum does not look thin at all, which significantly aggravates the situation. Almost half of all parents face this problem. And although a short frenulum can be noticed by a specialist even in newborns, parents learn about it when the baby begins to talk.
Pathology of the frenulum of the tongue can be congenital and hereditary. It should be understood that these concepts are completely different. If a congenital pathology is already present at birth, then a hereditary pathology is most often already present in one of the family members.
The concepts of complete and partial short frenulum of the tongue in a child are also distinguished. The level of discomfort of the child and the type of treatment chosen (surgical intervention or corrective exercises) depend on the type of pathology.
With a full frenulum, the child's tongue is practically immobilized, which makes it much more difficult to pronounce most speech sounds. With this type of pathology, muscle cords form. In the case of partial pathology of the frenulum of the tongue, the role of muscle cords is performed by connective tissue.
Why is a short frenulum dangerous?
A short frenulum is a congenital pathology in which the development and functionality of the ligamentous connection between the tongue and the lower jaw is disrupted. At the same time, the mobility of the tongue in the oral cavity is limited so much that it causes speech problems in the child.
Problems with the frenulum of the tongue in a child can occur in two ways. Young children who are breastfed or bottle-fed and have this pathology may have problems with sucking. This occurs due to the fact that the frenulum of the tongue is so short that it simply does not allow the tongue to function adequately.
With a short frenulum of the tongue, the baby cannot be fully breastfed, due to the fact that it is difficult for him to suck out a sufficient amount of breast milk. Therefore, in this case, immediately after the birth of the baby, he has real difficulties with feeding.
The second option for realizing the problem associated with a pathological frenulum of the tongue is speech defects and they arise much later. Partial immobility of the tongue leads to the fact that the child is not able to pronounce certain sounds correctly; his speech remains similar to babbling, “lisping.”
Short frenulum of the tongue
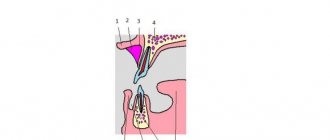
The frenulum of the tongue (frenulum linguae) is a fold of the oral mucosa that runs along the midline and connects the floor of the mouth with the lower surface of the tongue (encyclopedic dictionary of medical terms, 1984). Sometimes the terms lingual ligament and sublingual ligament are used. The function of the tongue frenulum is to fix the tongue to the soft tissues of the oral cavity, prevent tongue retraction and glossoptosis, especially during the neonatal period. Normally, the frenulum of the tongue comes from the middle of the lower surface of the tongue and is attached to the mucous membrane of the floor of the mouth in the area of the excretory ducts of the sublingual salivary glands (Fig. 1). By the age of 18 months, the free tip of a child's tongue should reach at least 16 millimeters. Measuring the absolute dimensions of the lingual frenulum has not found widespread use in clinical practice. It is believed that the length of the frenulum of the tongue during the period of mixed dentition should be at least 21 mm, and the width no more than 4 mm.
Fig.1. Variants of attachment of the frenulum of the tongue are normal. The permissible place of attachment to the lower surface of the tongue is highlighted in black. Green – to the mucous membrane of the floor of the mouth.
A short frenulum of the tongue is one of the most common MINOR DEVELOPMENTAL ANOMALIES of the oral cavity. This pathology is sometimes called ankyloglossia. Ankyloglossia (ankyloglossia) is a developmental anomaly: shortening of the frenulum of the tongue from Ankilos - (Greek, crooked, curved) a component of complex words, meaning 1) “curvature”, hook-shaped 2) “stiffness or fusion of parts” and Glossa - (Greek. ) – language (encyclopedic dictionary of medical terms 1982). This term is not widely used in the domestic medical literature and clinical practice, although it reflects some clinical manifestations (curvature of the tongue and its stiffness).
According to various authors, a short frenulum of the tongue is diagnosed in 2.3-19% of subjects, and in boys, a short frenulum of the tongue occurs significantly more often than in girls with a frequency of 1: 300 in newborns. Such a significant scatter of statistical data indicates the vagueness of the applied diagnostic criteria and different principles of classification. The length of the short frenulum of the tongue is no more than 1.7 cm, but this does not always cause dysfunction of the tongue, especially if the anatomical frenulum is located correctly.
Etiologically, a short frenulum of the tongue is often caused by a hereditary predisposition. There is also information about the significance of intrauterine trauma to the frenulum of the tongue (from thumb sucking).
Clinical manifestations of a short frenulum of the tongue.
During the period of toothless oral cavity (up to 6 months), with the jaws closed, the tongue occupies the entire oral cavity, its edges extend beyond the gums. Normally, in the anterior part of the oral cavity there is a gap between the gingival ridges of approximately 3 mm. the tip of the tongue is located between them. The mobility of the tongue root is small and increases to normal by 3-6 months. During this period, the child’s sucking and swallowing is infantile , i.e. When swallowing, the tongue pushes away from closed lips, and there is visible tension in the facial muscles of the perioral area. Subsequently, the infantile type of sucking and swallowing is replaced by a somatic one , when the tongue is pushed away from the palatal surface of the teeth and the anterior surface of the hard palate. During the formation of a temporary bite, the tongue is normally located behind the teeth.
With a short frenulum, when the tongue is tense, its tip is forked in the form of a stylized heart, the edges of the tongue are raised (Fig. 2).
Fig.2. Short frenulum of the tongue. The length of the frenulum is 1.3 cm - 8 mm less than the norm. The tip of the tongue is forked.
The child cannot lick the upper and lower lips. When you try to stick it out, the back of the tongue rises, the tongue becomes curved, “humpbacked”. The short frenulum starts from the tip of the tongue or in its anterior third and is attached to the mucous membrane of the alveolar process of the mandible (Fig. 3). There are variants of ankyloglossi, when the frenulum is attached in the area of the excretory ducts of the sublingual salivary glands, and then, changing direction, is woven into the mucous membrane of the alveolar process in the form of a “crow’s foot” (Fig. 4).
Even with a short frenulum (less than 1.5 cm), if it is attached to the soft tissues of the floor of the mouth, functional disorders do not always occur - difficulty sucking during breastfeeding and disturbances in sound pronunciation during the formation of phrasal speech.
Fig.3. Options for attaching the frenulum of the tongue in ankyloglossia. The place where the frenulum attaches to the tip of the tongue and its anterior third is highlighted in black. Green – to the mucous membrane of the alveolar process and the transitional fold of the mucous membrane of the floor of the mouth.
Rice. 4. The short frenulum of the tongue is attached to the mucous membrane of the alveolar process in a fan-shaped manner - in the form of a “crow’s foot”. The back of the tongue bends when trying to lift it.
As a result of the stiffness of the tongue caused by a short frenulum, malocclusions can form, the first signs of which during the period of temporary occlusion are the rotation of the central lower incisors to the lingual side.
Functions of the language.
The functions of the tongue can be divided into two large groups: sensory and motor (mechanical). In some animal species, the tongue plays a significant role in thermoregulation.
Sensitive functions include taste, temperature, tactile, and pain. Pathology of the frenulum of the tongue does not affect sensory functions.
The motor functions of the tongue, in turn, can be divided into nutritional, speech and aesthetic.
The tongue, as an organ of the digestive system, is involved in providing nutritional functions - chewing, swallowing, sucking, licking, lapping, cleansing the mouth (spitting). A short frenulum of the tongue can interfere with the implementation of these mechanical functions, mainly sucking. Licking and lapping are rudimentary nutritional functions for humans.
The tongue is one of the main articulators providing the function of speech. Speech is unique to humans; its physiological basis is the second signaling system. Pathology of the frenulum of the tongue does not affect the formation of speech in general, but only the formation of some sounds.
The aesthetic meaning of language plays a significant role in the socialization of an individual. Various “teases”, showing the tongue, are characteristic of people of different ages, social status, races and nationalities.
Sucking.
Currently, the importance of the implementation of the sucking instinct during the newborn period and breastfeeding (natural) feeding is beyond doubt - “...it is in natural feeding that real ways and opportunities are laid for achieving biological perfection within the framework of one’s own species, the implementation and adjustment of the genetic fund, species-specific forms of initial socialization... The work of the muscular sucking apparatus when feeding a child determines the occurrence of efforts and tensions that most adequately regulate the anatomical formation of the dentoalveolar system, the cerebral skull, as well as the sound reproduction apparatus" (Vorontsov I.M., Fateeva E.M. Khazenson L.B., 1993 ).
Sucking is an innate unconditioned reflex (instinct) that is formed during intrauterine development. In an 18-week fetus, sucking movements of the lips are observed, at 21-22 weeks - spontaneous sucking, at 24 weeks - searching and sucking reactions. The sucking reflex is one of the most stable, the absence or significant suppression of which is extremely rare. Thus, the sucking reflex is observed even in mammals with aencephaly. Excitation from the receptors of the lips and tongue is transmitted through the centripetal nerves (trigeminal) to the center of sucking, located in the bulbar region, the centrifugal nerves (trigeminal, facial, hypoglossal) transmit excitation to the tongue, chewing and facial muscles that ensure the act of sucking. In the first weeks of a child's life, sucking is an unconditioned reflex, which is gradually replaced by a mixed and then a conditioned reflex.
An unrealized sucking instinct often leads to various types of obsessive-compulsive neuroses, sometimes manifesting throughout life.
When breastfeeding, the act of sucking is divided into two stages - suction and compression. The child clasps the areola of the breast with his lips and gums, more from below than from above; the nipple is at the level of the soft palate and does not participate in sucking. At the same time, the velum palatine descends. The tongue, taking the form of a groove descends together with the lower jaw downwards and backwards, a muscle wave is formed, passing from the front to the middle part of the tongue, thus creating a negative pressure in the oral cavity - 2-4 mm. mercury column. Tightness is also ensured by transverse folds on the mucous membrane of the lips and palate, and Bisha's fatty lumps in the cheeks. Then the lower jaw rises and the alveolar arches compress the chest, allowing the sphincters of the milk ducts to relax. Thus, alternating negative pressure during suction and positive pressure during compression ensures a dosed and rhythmic flow of milk. The tongue does not have an exclusively independent role in sucking ; its movements are strictly coordinated with the movements of the lower jaw, chewing and facial muscles.
Bottle sucking is different from breastfeeding. When sucking a bottle, the child makes mainly retracting movements, which are provided by the muscles of the cheeks and forward movements of the tongue. In this case, the flow of milk is continuous.
Difficulties in feeding during the newborn period.
Contraindications to breastfeeding.
The mother has: especially dangerous infections (smallpox, hemorrhagic fevers, etc.), open form of tuberculosis, syphilis, decompensation of chronic diseases of internal organs, malignant neoplasms, acute mental illnesses, treatment with certain medications. Contraindications to early breastfeeding are surgical delivery, large blood loss.
The child has: phenylketonuria, galactosemia, “disease with the smell of maple syrup.” Contraindications to early breastfeeding are Apgar scores below 7.
Difficulties in natural feeding.
On the maternal side: primary hypolactia, significant hyperlactia, abrasions, cracks, changes in the shape of the nipples (Fig. 5), incorrect feeding technique, alternating breast and bottle feeding. Changes in the taste and smell of milk when eating certain foods and medications.
Fig.5. Types of nipples. Difficulties or even impossibility during feeding are caused by a depressed, poorly stretchable nipple. In such cases, a nipple corrector (usually vacuum) is used in the prenatal period. A long nipple can also affect the quality of feeding during the formation of the so-called. “Nipple sucking”, when the baby does not latch onto the breast, but sucks mainly on the nipple.
On the part of the child: the child’s diseases, both acute (ARVI, rhinitis, etc.), and congenital, birth trauma, etc.. The child’s rapid fatigue when sucking is often associated with neurological problems. The presence of microgenia and cleft palate create significant problems during feeding. There is a category of children who suck poorly and do not show anxiety from hunger from the very beginning of feeding. An in-depth examination of both mother and child does not reveal any pathology. The terms “lazy suckers” and “hungry suckers” describe this problem quite accurately. According to I.M. Vorontsova (1993) in such children the maturation of the hypothalamic hunger centers may be delayed.
In itself, the presence of a short frenulum of the tongue during the neonatal period and breastfeeding does not affect or only slightly affects the quality of feeding. Especially if the short frenulum of the tongue is attached to the soft tissues of the floor of the mouth, without causing stiffness of the tongue. In this case, the functionality of the tongue necessary for sucking is not impaired. Healthy children, with the correct feeding technique and the absence of other reasons, adapt quite quickly.
The only exceptions are extreme variants of ankyloglossia, when the frenulum of the tongue starts from the very tip and is attached to the top of the alveolar process. In any case, the decision on surgical treatment is made only after examination by a neonatologist, pediatrician and other specialists.
Speech
At birth, a child has only the potential ability to form speech. The articulators are not sufficiently developed, the larynx is located much higher than in an adult, the speech-motor analyzer is not able to provide accurate articulatory movements of the lips, tongue, etc. In the second month of life, the first articulatory movements appear in the form of babbling, not connected by conditioned reflex with primary signal radiators. By the end of the first year of life, the first words used by the child for the purpose of verbal communication with other people are formed. A second signaling system is being formed. The child learns to form an image abstracted from circumstances. Abstraction and systematization of complex concepts allow you to create first a passive and then an active vocabulary. At 2-3 years of age, the development of phrasal speech begins. Coordination of the functioning of the speech apparatus is ensured by the cortical part of the speech-motor analyzer, located in the left hemisphere of the brain in the posterior part of the third frontal gyrus. The motor center of speech (Broca's center) in its work is connected with the centers of auditory (Wernicke's center) and written speech, as well as with extensive mnestic fields in the frontal and posterior parts of the cerebral hemispheres, providing the semantic and content aspects of speech.
There are three critical periods in speech development. The first (up to 2 years) is the formation of the prerequisites for speech, the foundations of communicative behavior. The second (2.5-3 years) is the transition from situational to contextual speech. Third - (6-7 years) the beginning of the development of written speech. The influence of unfavorable environmental and hereditary factors (acute and chronic diseases of the child, central nervous system lesions, articulator anomalies, insufficient socialization, etc.) can lead to speech development disorders.
Here are the definitions of some speech disorders.
Agrammatism is a violation of the understanding (impressive side of speech) and use (expressive side of speech) of the grammatical means of the language.
Agraphia and dysgraphia – impossibility (agraphia) or partial specific impairment of the writing process (dysgraphia).
Alalia is the absence or underdevelopment of speech due to organic damage to the speech areas of the cerebral cortex in the prenatal or early period of a child’s development.
Alexia and dyslexia – inability (alexia) or partial specific impairment of the reading process (dyslexia).
Dyslalia is a violation of sound pronunciation with normal hearing and intact innervation of the speech apparatus. Synonyms: tongue-tiedness, sound pronunciation defects, phonetic defects, phoneme pronunciation defects. Dyslalia can be mechanical (improper structure of articulators) and functional (no visible anatomical causes).
Dysarthria is a violation of the pronunciation aspect of speech caused by insufficient innervation of the speech apparatus. In mild cases of dysarthria, when the defect manifests itself mainly in articulatory-phonetic disorders, we speak of its erased form.
Stuttering is a violation of the tempo-rhythmic organization of speech, caused by the convulsive state of the muscles of the speech apparatus.
Mutism is the cessation of verbal communication with others due to mental trauma.
Speech underdevelopment is a qualitatively low level of development of a particular speech function or the speech system as a whole.
GSD (general speech underdevelopment) is a variety of complex speech disorders in which children have impaired formation of all components of the speech system related to the sound and semantic aspects. OHP can be level I, II, and III. ONR can be complicated by dysarthria, rhinolalia, alalia, etc.
Rhinolalia (nasality) is a violation of voice timbre and sound pronunciation, caused by anatomical and physiological defects of the speech apparatus.
FFN (phonetic-phonemic underdevelopment) is a violation of the process of formation of the pronunciation system of the native language in children with various speech disorders due to defects in the perception and pronunciation of phonemes.
Stiffness of the tongue caused by a short frenulum does not affect the overall development of speech. A short frenulum of the tongue can only contribute to the formation of some variants of dyslalia.
Treatment of patients with a short frenulum of the tongue.
Indications for surgical treatment.
1. During the neonatal period and breastfeeding.
Severe sucking disorders. The child is not gaining weight. Significant stiffness of the tongue with extreme shortening of the frenulum (goes from the tip of the tongue to the top of the alveolar process). At the same time, the child is somatically and neurologically healthy. There are no reasons that make breastfeeding difficult for the mother.
Indications for surgical treatment are jointly determined by a dentist, neonatologist or pediatrician, neurologist, and other specialists, if necessary.
We believe that there are no absolute indications for surgical treatment of a child with ankyloglossia at this age. Especially when the short frenulum of the tongue is attached to the soft tissues of the floor of the mouth.
2. During the period of formation of phrasal speech (from 2.5 years onwards).
Mechanical dyslalia is a violation of the pronunciation of certain sounds (mainly R, L).
Indications for surgical treatment are jointly determined by the dentist and speech pathologist-speech pathologist if it is impossible to “stretch” the frenulum of the tongue with the help of speech therapy massage and speech therapy is ineffective. In this case, it is necessary to clearly differentiate the types of speech disorders, because Surgical treatment of ankyloglossia with OHP, dysarthria, and delayed psychomotor development can significantly aggravate the existing pathology.
We consider it not only inappropriate, but also harmful to carry out surgery for a short frenulum of the tongue in order to prevent possible speech disorders, especially at an early age.
3. Indications for surgical treatment of patients with dentofacial anomalies and a short frenulum of the tongue are determined by the orthodontist. Bite disorders, caused, among other things, by the unfavorable influence of a short frenulum of the tongue, are characterized by a lack of tendency to self-regulation. In such cases, surgical treatment is also indicated from a preventive point of view, starting from the period of formation of the temporary occlusion.
Anesthesia. We consider it unacceptable to perform surgical treatment of patients with a short frenulum of the tongue without pain relief.
When using local anesthesia, both application and infiltration, it is necessary to remember the phenomenon of sublingual absorption. The toxic or allergic effect of the anesthetic when introduced into the sublingual area increases significantly. In addition, the floor of the mouth is a powerful reflexogenic zone. The secretory and motor activity of the gastrointestinal tract can be inhibited or activated when exposed to the mucous membrane of the middle part of the tongue. Stimulation of the tip and sides of the tongue has a reflex effect on the cardiovascular and respiratory systems.
We consider the use of local anesthesia during operations for short frenulum of the tongue to be inappropriate under the age of 7-8 years and in children with various behavioral disorders, hyperactivity, etc.
The decision on the choice of general anesthesia method is made by the anesthesiologist, and it is necessary to remember the possibility of aspiration of blood and saliva during surgery.
Types of surgical treatment of patients with a short frenulum of the tongue.
Any option for surgical treatment of patients with a short frenulum of the tongue requires a preliminary laboratory examination (clinical laboratory minimum - clinical blood tests, urine tests, ALT)!
Frenulotomy is a dissection of the frenulum of the tongue (what is often called “cutting the frenulum”). The tongue is lifted with tweezers or the back of a grooved probe at the site of attachment of the frenulum to the lower surface of the tongue. The frenulum is cut with scissors. No stitches are required. This type of operation is used during the neonatal period. Some authors, justifying this technique, write about the so-called. “avascular zone” of the thin and transparent frenulum of the tongue during the newborn period. We believe that with this type of tongue frenulum, surgical treatment during breastfeeding is not indicated, because in this case, there is no pronounced dysfunction of sucking. We do not recommend using this method due to possible complications. Bleeding, despite the widespread belief about the “avascular zone,” is possible and can lead to serious consequences. Long-term complications of frenulotomy performed without sutures include the formation of scar shortening of the frenulum and scar stiffness of the tongue (Fig. 6).
Rice. 6. Cicatricial shortening of the frenulum of the tongue. Child 5 years old. At the age of three months, frenulotomy was performed (without sutures) to prevent speech disorders. Severe mechanical dyslalia. Emerging progeny. Chronic desquamatous glossitis.
Frenuloplasty is a local plastic lengthening of the cortical frenulum of the tongue.
There are two types of frenuloplasty.
First way. The frenulum at the place of its attachment to the tongue is fixed with tweezers and cut with scissors by about 2-3 mm. the resulting wound is sutured with catgut or other quickly absorbable suture material. The remaining ends of the ligature are used as a holder. Using the ligature, the tongue is pulled upward and anteriorly, while cutting the frenulum at the point of attachment to the lower surface of the tongue to the mouth of the excretory ducts of the sublingual salivary glands. The underlying fibrous cords are dissected and the tongue is mobilized. The resulting diamond-shaped defect is sutured “on itself” with catgut. This operation option is a type of VYplasty (Fig. 7).
Rice. 7. The diamond-shaped defect is sutured “on itself” while constantly pulling the tongue upward and anteriorly by the holder. If the frenulum is fan-shapedly woven into the mucous membrane of the alveolar process, you can additionally cut it with an electrocoagulator at the point of attachment to the alveolar process.
The second method differs from the first in that additionally, after partial suturing of the surgical wound, plastic surgery is performed using the figures of opposing triangular flaps 600 x 600.
When applying rough sutures in the area of the excretory ducts of the sublingual salivary glands, acute retention of saliva may occur - the so-called. "salivary colic". This rare complication associated with a violation of surgical technique develops during the first hours after surgery. In such cases, 1-2 sutures are removed and antibacterial therapy is prescribed to prevent sialodochitis.
Frenulectomy - excision of the frenulum of the tongue. The frenulum of the tongue is excised wedge-shaped and sutures are applied. An option for frenulectomy is laser ablation. The disadvantages of this method include the lack of mobilization of the tongue.
The postoperative period usually proceeds smoothly . In rare cases, pain relief is required. A gentle diet is prescribed for one to two days, and rinsing the mouth with antiseptic solutions. 3-4 days after the operation, you can begin classes with a speech therapist and conduct special classes.
Reasons for the development of tongue frenulum pathology in a child
The formation of an anomaly associated with a short hyoid membrane begins before the birth of the child. This is preceded by negative factors, which include:
- genetic predisposition;
- infection of the fetus during pregnancy;
- viral and infectious diseases suffered by the mother during pregnancy;
- mechanical injuries to the expectant mother’s abdomen;
- the age of the expectant mother is over 35 years;
- unfavorable environmental conditions;
- the influence of other factors of unknown etiology.
How to prepare for frenuloplasty
In the process of preparing for surgery, you should consult with a urologist, who will draw up a complete list of recommendations based on the individual characteristics of the patient and the results of the tests performed. A week before the planned procedure, it is necessary to avoid taking any aspirin and non-steroidal anti-inflammatory drugs.
On the day of surgery, you need to perform a number of simple steps:
- carry out a thorough toilet of the genitals and hygienic cleaning using special products for the care of the intimate area;
- shave the scrotal area;
- give up caffeine in the morning, and breakfast should be as light as possible, without fatty foods;
- Bring a set of sterile wipes and spare linen with you to the clinic.
If the patient is allergic to various drugs, you must inform your doctor about this, and take an antihistamine the day before frenuloplasty. In cases of a negative reaction of the body to general anesthesia, it is required to notify the anesthesiologist.
Compliance with all general recommendations for preparing for the correction procedure contributes to the most effective implementation of all surgical procedures with minimal risks of subsequent deviations.
How to recognize pathology in a child
A neonatologist, pediatrician, or the mother herself can recognize a pathological frenulum of the tongue in a newborn. If during the first and subsequent breastfeedings the baby experiences difficulties and cannot grasp the nipple correctly, then there is a reason to consult a doctor.
The second common sign of a pathological frenulum of the tongue in children is the occurrence of a speech defect when they begin to speak in phrases, namely at 3-4 years. Most often, with this anomaly, children do not pronounce several letters: “zh”, “sh”, “sch”, “ch”, “z”, “l” and “r”. Moreover, the sound “l” is easily pronounced if it is followed by a soft vowel, for example, “i”, “yu”, “e”, “e”, “ya”, in other cases it is simply “swallowed”. If there is incorrect pronunciation of sounds, then an examination by a speech therapist is necessary.
The most common symptoms of a tongue tie in a child are the following:
- the child is not able to reach the front teeth of the upper jaw or palate with the tip of his tongue;
- the child may have difficulty moving the tip of the tongue from one side to the other;
- the front teeth of the lower jaw may have a gap between each other;
- when the tongue is pulled forward, its tip remains flat, square or heart-shaped (that is, the front edge of the tongue seems to bifurcate);
- feeding problems in newborns.
It is important to understand that if the problem of the tongue frenulum exists, then sooner or later it will have to be solved. The sooner measures are taken, the easier and more painlessly the baby will endure them.
Operation techniques
There are two methods of performing tongue frenuloplasty: traditional (classical) and laser. This is a more modern and safer method. The laser allows the operation to be performed with great precision and does not cause bleeding after the procedure. In addition, there is no need for stitches, and healing time is significantly reduced. This is especially important if you need to perform laser frenuloplasty on a child: the baby will tolerate the procedure much easier.
Depending on what pathology of the frenulum is detected, the doctor uses one of three techniques: cuts the frenulum, removes it, or changes the attachment site. The number of cuts and their shape depend on the choice of technique.
In what cases is it necessary to trim the bridle?
The operation of cutting the frenulum of the tongue is called frenulotomy . It is classified as simple and requires only local anesthesia.
Heavy bleeding during frenulotomy is very rare; after a couple of hours the child will be able to return to the usual rhythm of life.
If a short frenulum interferes with the newborn baby's ability to receive nutrition, it must be trimmed. The decision about surgery is made by a pediatric neonatologist.
For infants, as a rule, the operation is performed without anesthesia, since only the sublingual film of connective tissue is dissected, which has practically no blood vessels or nerve endings.
For children aged 3-5 years, surgery to cut the frenulum is performed under local anesthesia. The dentist decides whether surgery is necessary, and the speech therapist prescribes the referral.
Before the operation, the child needs to donate blood for a detailed analysis, which will display numerous indicators, including the number of platelets and the rate of blood clotting.
Surgical intervention is performed provided that the pathology is moderate or severe with limited tongue mobility. After surgery, speech therapy sessions are necessary.
There are a number of indications for frenulotomy, and limited tongue mobility is not the only one. The formation of malocclusion in a child, displacement and disturbances in the formation of the dentition, low effectiveness of speech therapy and articulation gymnastics, as well as the need to install dental implants or orthodontic structures for the child.
Pathology of the tongue frenulum does not always require surgical intervention. If the child does not experience any discomfort during breastfeeding, and his pronunciation of sounds is satisfactory, then it is likely that a speech therapist will help solve the problem. In this case, the child attends special classes, performs speech therapy exercises, articulation gymnastics, etc.
Frenum trimming with laser
Laser frenulum trimming is a simpler, faster procedure that does not cause bleeding. Laser procedures are distinguished by their antibacterial effect, comfortable perception of the procedure by the patient, and the absence of a long recovery period. The laser beam instantly seals the vessels of the frenulum of the tongue, which does not require sutures. Pain relief is usually done using a gel or spray.
Don't be afraid to sign your child up for surgery. By solving the problem with the length of the frenulum, you will give your baby freedom of diction and free him from the feeling of constraint. Make an appointment at the Mira clinic for a consultation by phone.
Treatment methods
Problems associated with a short frenulum of the tongue can be solved with medicinal and non-medicinal methods.
Medicinal methods involve surgical intervention of varying degrees.
If the sublingual membrane requires dissection, but it is quite thin and elastic, then the doctor dissects it right at the appointment. In this case, anesthesia is not provided, since the procedure is classified as mild.
More complex types of dissection of the frenulum of the tongue include frenulotomy, which is indicated for children with thicker frenulums. Frenulotomy is performed under local anesthesia with tissue dissection and subsequent suturing.
Complications of this operation may include stomatitis, prolonged bleeding from the wound, infection in the wound, etc. After frenulotomy, the child should receive pureed food for some time, as chewing may be painful.
Non-drug treatment methods include special types of massage, exercises to correct the frenulum of the tongue, and individual sessions with a speech therapist.
Non-drug methods are recommended when the condition of the child’s tongue frenulum is not critical and allows refusal of surgery. The decision on this is made by a speech therapist, pediatrician and dentist. Classes with a speech therapist include various exercises, articulation gymnastics, tongue twisters and poems.
Since a short frenulum of the tongue causes some speech defects, classes with a speech therapist are necessary both in the postoperative period and as a correction.
A massage aimed at stretching the frenulum of the tongue includes a list of special exercises. It is important that the classes are systematic so that they give a positive result.
Massage instead of cutting the frenulum is recommended for children in two cases: if the condition of the frenulum is not so critical and the problem can be solved with non-drug treatment methods; if the frenulum is cut when the child is older (over 5 years old) and the surgery will not solve problems with speech impediment.
Circumcision and removal (excision) of the frenulum
Surgical intervention to circumcise the frenulum of the foreskin is not considered mandatory if there are no alarming symptoms. But most experts advise carrying out this procedure as a preventive measure.
Carrying out the procedure
- in circumcision of the foreskin followed by frenuloplasty, mainly for phimosis;
- in excision of the frenulum followed by plastic surgery to restore the anatomical length;
- in excision of the frenulum of the foreskin.
Circumcision of the foreskin and frenulum together is carried out for medical reasons or for religious reasons. If circumcision is performed for medical reasons, the most common reason for the procedure is phimosis - this is a pathological narrowing of the foreskin, which makes it difficult to expose the head of the penis. Phimosis can also be either congenital or acquired as a result of diseases or injuries.
In its presence, the patient may experience difficulties during sexual intercourse, urination, and also very often suffers from swelling and inflammatory processes.
The main danger of this disease is the formation of cracks in the frenulum and foreskin, which can turn into scars and welts after healing. In some cases, the tissues of the glans penis adhere to the foreskin, which can cause pain when trying to open the glans. During the operation, the foreskin and frenulum are excised, which can lead to the return of anatomical functions. Also, phimosis can be operated on with subsequent preservation of part of the foreskin. Circumcision can also be performed simultaneously with frenuloplasty.
Indications for frenulum circumcision
The operation of circumcision of the foreskin and frenulum, in contrast to frenulotomy, is performed not only in adults, but also in children and infancy, if indicated.
Operation techniques
At the moment, circumcision of the frenulum of the foreskin can be carried out using a standard method using a scalpel, as well as using laser technologies.
The operation is carried out over thirty to forty minutes. The likelihood of complications is minimal, and in most cases there are none at all.
During the recovery period, it is very important not to violate hygiene, and also to follow all established instructions and doctor’s advice. The scar after surgery can heal very quickly and becomes almost invisible. Stitches are usually applied using special self-absorbable threads; they can disappear after ten days. After healing and rehabilitation, it will take fourteen to twenty-one days, after which you can continue to be sexually active.
Exercises for correcting the frenulum of the tongue and in the postoperative period
Postoperative frenulum stretching and correction exercises are aimed at developing new muscle movements of the tip of the tongue inside and outside the mouth. Regular practice will increase the range of movement of the tongue.
Articulation exercises by themselves will not improve speech and will not be able to correct the defect, so it is very important to carry them out in conjunction with individual speech therapy sessions.
The most common and universal exercises for stretching and correcting the frenulum of the tongue are given here in the article. Following them, you can study at home with your child on your own:
- Stretch your tongue forward, then stretch the tip up to your nose, then down to your chin. Relax, repeat the exercise several times (at first, up to five repetitions are enough, gradually the number of repetitions must be increased, bringing them to twenty).
- The exercise is performed by analogy with the previous one, moving the tongue left and right. The number of repetitions is also gradually increased to twenty.
- Open your mouth wide. Use the tip of your tongue to touch the upper incisors and try to press on the teeth with all your might, not allowing your mouth to close. During each execution, mentally count to ten. The number of repetitions is the same as the previous ones.
- The exercise is performed in front of a mirror. The mouth is wide open. When performing the exercise, it is important to monitor the movements of the tongue. Pronounce the syllables “dar-dar-dar”, “nar-nar-nar”, “tar-tar-tar”, etc.
- Sticking your tongue forward as much as possible, alternately “lick” your upper and lower lips.
- Closing your mouth, move your tongue from right to left and back, forcefully pressing the inside of your cheeks with the tip of your tongue.
To achieve good results, exercises should be performed daily, in several approaches, for 15-20 minutes . The articulation of specific sounds can be gradually corrected.
Important! You can begin to perform exercises for the frenulum of the tongue only after the wound has completely healed.
Speech therapy classes should include exercises to improve the functioning of the speech apparatus and oral kinesthesia, without which it is difficult to claim significant improvements in the development of a child’s speech. Many young patients, after cutting the frenulum, begin to speak more quietly and more quickly, trying to “drown out” speech problems.
Treatment - In most cases, treatment is surgical.
When diagnosing a short frenulum, an operation of cutting the frenulum, or frenulotomy, is performed in the maternity hospital. At this age, the procedure is completely painless. It is performed without the use of anesthesia, since the frenulum itself does not contain nerve endings.
If correction for one reason or another was not carried out in infancy, it is usually done at an older age (preschool and school).
There are two methods of treatment: plastic surgery of the frenulum of the tongue and so-called stretching, which is carried out by a speech therapist. Please note that it is the dentist who makes the decision on surgical treatment or stretching of the hyoid frenulum.
Complications after frenuloplasty
The procedure is a simple operation and is carried out quite quickly; on average, all surgical procedures take from 15 to 30 minutes. The number of risks is minimal.
Among the undesirable consequences are:
- infection in the wound, which contributes to the formation of balanoposthitis;
- allergic reaction of the body to the use of various anesthetics;
- suture dehiscence and subsequent bleeding;
- painful sensations in the area of the lower part of the penis;
- swelling of the foreskin;
- purulent discharge from the wound formed after the intervention;
- increase in body temperature.
Infectious infections occur quite rarely due to the use of antimicrobial drugs, which are prescribed to the patient for the rehabilitation period. The maximum duration of pain after the correction is two months.
Manipulation technique
In medicine, two directions of correction of the frenulum of the genital organ are used:
- frenulotomy, dissection of the connecting tissues of a previously intact frenulum;
- frenuloplasty, restoration of the length of the frenulum when a scar forms after its rupture.
The manipulation technique involves dissecting the tissues of the frenulum in the transverse direction, followed by stitching them longitudinally, increasing its length. The operation is performed using local anesthetics and takes no more than a quarter of an hour; the patient remains under observation for about half an hour, after which he is sent home. The period of complete recovery takes from two weeks to a month.
Immediately after the operation, no extraneous sensations are observed; during the next 24 hours after the intervention, some discomfort and pain persist:
- this is due to the presence of a wound surface that comes into contact with urine when the bladder is emptied;
- as well as during spontaneous erection at night, when, with an increase in the size of the organ, tension occurs in the unhealed tissues.
After healing, a neat suture remains, which runs along the lower zone of the organ. Restoring the length of the frenulum allows you to fully and painlessly open the head, without causing pain and discomfort during erection and sexual intercourse.
Symptoms and diseases of the frenulum of the penis:
- Rupture of the frenulum of the penis
- Removal of the frenulum of the penis
- Growths on the frenulum of the penis
- Soreness of the frenulum of the penis
- Papillomas on the frenulum of the penis
- Rash on the frenulum of the penis
- Itching of the frenulum of the penis
- Frenum of the penis
- Inflammation of the frenulum of the penis
- Swelling of the frenulum of the penis
Where to have plastic surgery of the frenulum of the penis?
Our clinic uses modern equipment and has all the necessary tools for safe interaction with the patient. The consultation is conducted by doctors with extensive experience and knowledge in various branches of urology, who will give practical recommendations on preparing for the procedure, and then draw up the most effective plan for the rehabilitation period.
Our clinic has:
- specialized rooms for conducting hardware diagnostics;
- own laboratory for prompt research of the obtained tests;
- a modern operating room equipped with the required equipment and the necessary additional technical components.
During the operation, high-quality asepsis is used, which minimizes the risk of possible infectious complications later. A delicate approach that allows you to solve all intimate problems in a strictly confidential manner.