Pulpitis accounts for approximately a quarter of all dental diseases. Pulpitis is an inflammatory process of the internal tissues of the tooth (pulp). The pulp is a unique tissue in the human body. It is a complex of connective tissue, blood vessels and nerves. The pulp has a complex structure and ensures the normal functioning of teeth. Inflammation of the pulp significantly affects not only the health and aesthetics of teeth, but also the patient’s quality of life. Moreover, without comprehensive treatment, pulpitis is prone to complications, which makes treatment difficult. A timely visit to a doctor will help get rid of the disease and prevent its reappearance.
What is pulpitis and how does the disease progress?
Pulpitis develops when carious destruction of the integrity of the tooth occurs when food and microorganisms penetrate the tooth cavity (pulp). Another way of developing the disease is infection from neighboring affected teeth through blood vessels, which occurs much less frequently and is called retrograde pulpitis. There are other, rare pulpitis:
- Traumatic, develops as a result of a crack, break, or chip of a tooth.
- Concrete occurs when there is excessive deposition of mineral formations that begin to replace the internal tissues of the tooth.
- Inflammation develops due to incorrect treatment, the use of low-quality materials, and accidental opening of the pulp.
Regardless of the type of infection, inflammation requires immediate treatment. Among the factors that increase the likelihood of developing pulpitis are: insufficient hygiene, osteoporosis and diabetes.
There are three stages of pulpitis: acute, chronic and aggravated chronic pulpitis. According to the ICD-10 classification used when making a diagnosis, the disease is divided into several categories.
Pulpitis acute
- K04.00 - initial inflammation of the pulp.
- K04.01 - acute focal pulpitis.
- K04.02 - purulent abscess.
The diagnosis is made when the pulp first comes into contact with infection. This includes the serous form of the disease, focal and purulent abscess.
First, the tooth becomes sensitive to temperature: hot or cold. Unlike caries, pain does not subside when the irritant is removed. Then comes the diffuse phase - the pain intensifies at night, is periodic, and often radiates to the temple or other parts of the face. With the transition to the chronic phase, the pain disappears, or is characterized by the patient simply as an unpleasant sensation.
Chronic pulpitis
- K04.03 - fibrous.
- K04.04 - gangrenous.
- K04.05 - pulp polyp.
Chronic pulpitis occurs after the acute phase of the disease. It is characterized by (irreversible) destructive changes in tissues, divided into three types according to the type of changes:
- Fibrous
- the most common sluggish form of chronic pulpitis. It is characterized by the growth of connective, fibrous-granulation tissue in the pulp.
- Gangrenous
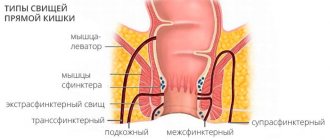
- This is a putrefactive inflammation, which is marked by a characteristic odor from the mouth. The gums often swell, and fistulas may form through which exudate flows out.
- Hypertrophic
- the most rare pulpitis, characterized by the growth and exit of the pulp into the carious cavity.
The chronic form is not painful, but severe pain may occur periodically.
Note! In the acute stage, the infected tooth mainly reacts to cold; in the chronic form, the source of pain is exposure to high temperature.
Complicated forms
- K04.1 - pulp necrosis.
- K04.2 - pulp degeneration.
By complicated course of the disease we mean both inflammation of the entire pulp and simultaneous damage to several canals. When the pulp degenerates, denticles are formed - dense mineral formations (stones). They cause pain when there is a sudden change in body position, as this causes them to shift. For example, such patients experience pain when flying, going up in an elevator, or playing sports.
Necrosis refers to the death of cells in the neurovascular bundle of the dental root. In fact, this is the final stage of the disease. Necrosis can occur due to pulpitis, damage to the blood supply to the tooth, or under the influence of toxic components of the filling material.
Symptoms
Acute pulpitis:
- Severe throbbing pain radiating to neighboring teeth, ear, throat, temple.
- Reaction to hot and cold, including cold weather.
- Painful attacks occur after certain periods of time and intensify in a supine position.
Fibrous pulpitis:
- The pain is aching in nature, worsening in the evening and at night.
- A feeling of “bursting” and heaviness in the affected tooth.
- A sharp temperature reaction that continues after removal of the irritant.
Gangrenous pulpitis with an open lesion cavity:
- Discomfort and heaviness in the area of the affected tooth.
- Pain when biting.
- Reaction to hot drinks and food with prolonged persistence of aching pain.
- The enamel is gray, the gums are red and swollen, there is a fistula.
- Putrid odor from the mouth.
Gangrenous pulpitis with a closed lesion cavity:
- Intense pain attacks.
- Vivid reaction to hot drinks and food with pain persisting for a long period of time.
These symptoms help you pre-diagnose the presence of pulpitis and consult a dentist as soon as possible.
Diagnosis of the disease
During the appointment, the doctor interviews the patient. Determines the nature of pain, the conditions for the manifestation of pain, intensity and duration. Then, he conducts an external inspection and tapping using hand tools. This allows us to identify the presence of a carious cavity, the density or, conversely, softness of the pulp, and assess the condition of the gums. After this, an x-ray is prescribed. It shows the condition of internal tissues and channels, the localization and extent of inflammation.
In some cases, electroodontodiagnosis is prescribed—this is an analysis of the tooth’s reaction to electricity. The study provides insight into the integrity and functionality of the nervous system. Normally, the pulp responds with a slight pain signal to the electricity passing through it. As caries progresses, degenerative processes occur that reduce the sensitivity of nerve receptors.
Why does purulent pulpitis occur?
Precursor of purulent pulpitis in children
and adults is acute pulpitis. The formation of pus occurs from the serous exudate that is present in the nerve. Due to an increase in its volume, metabolic processes occurring in the nerve suffer, which stimulates the accumulation of lactic acid and, as a result of this process, a decrease in the protective function of cells. It is accompanied by tissue breakdown and abscess. The infection that provokes the development of purulent pulpitis penetrates the pulp in different ways:
- from a carious cavity in the absence of treatment;
- during the treatment of periodontitis with dissection of the gums;
- through blood and lymph in infectious diseases.
Treatment of pulpitis
Pulpitis requires repeated visits to the dentist. Treatment of the initial stage of damage to incisors and canines takes 1–2 visits, more complex cases require 3–4 visits to the doctor. With serous pulpitis, complete recovery is possible with preservation of tissue viability. The first stage of therapy is opening the pulp chamber and removing carious areas. Further steps depend on the degree of tissue damage.
1. Conservative treatment
Drug therapy is recommended at the onset of the disease, if it is not aggravated by the inflammatory process. Antibiotics may be prescribed to stop the infection. At the next appointment, using an x-ray, they check whether the inflammation has been eliminated. If the dynamics are positive, a permanent filling is installed. Otherwise, more drastic measures are required: removal of the entire pulp. If you keep the pulp in the canals, the tooth will continue to be nourished and strengthened by dentin.
Devital extirpation
During the first appointment, the carious cavity is opened so that the doctor has access to the pulp. A devitalizing paste is placed there. Namely, today it continues to be briefly called “arsenic”. However, in fact it is a paste based on formaldehyde, resorcinol and paraformaldehyde. They are safe compared to arsenic compounds and are non-toxic. You can walk with a devitalizing paste, which is fixed with a temporary filling, for one week. Usually within 7 days it completely kills the pulp tissue. After the specified period, the dentist removes the paste; it cannot be left in the tooth cavity longer, otherwise it will poison the adjacent tissues, and the tooth will soon crumble.
At the next appointment, the doctor removes the pulp. Large, curved canals are carefully cleaned with special instruments. This procedure is called nerve ablation. Next, the empty canals are disinfected and filled with filling material. It is necessary to fill them completely, otherwise there is a risk of re-inflammation; for this, the doctor measures the length of the canal with apex locator electrodes. They are lowered into each channel, since their length can be different. The obtained data is compared with an x-ray.
The canal is treated, disinfected, and dried. Afterwards, the doctor fills it with special material. Our clinic uses the method of three-dimensional obturation of root canals with thermally modified gutta-percha. Gutta-percha pins are placed in the canals so that the sealer does not reach the upper hole by a few millimeters. Part of the pin is heated and removed. The dentist can monitor the process using x-rays.
When the canals are filled, the dentist again places a temporary filling. It is necessary for the gutta-percha to completely dry out and remove all moisture from it. This takes 4-5 days, after which you can install a permanent filling and restore the tooth.
The main disadvantage of devital extirpation is the duration of treatment, consisting of several visits to the doctor’s office:
- The first step is to open the pulp, remove carious lesions and apply a devitalizing paste.
- The second visit is to remove the nerve, clean the canals and fill them with gutta-percha.
- The final stage is filling and restoration of the tooth.
Pulpitis in children: classification
Depending on the degree of the process, partial or complete gangrene of the tooth is distinguished:
- When the caries process affects only part of the pulp of a given tooth, it is called partial gangrene. The rest of the living tissue is in constant contact with necrotic masses and toxic bacterial products. It is subject to constant destruction and chronic inflammation.
- If the entire pulp inside the chamber and the canals of the tooth are necrotic and also infected with anaerobic bacteria, this condition allows a diagnosis of complete gangrene.
What can happen if pulpitis is not treated?
Since in some cases the disease occurs without pain, many people put off going to the dentist until the last minute. Do not forget that while you are inactive, the disease progresses. Refusal to treat pulpitis can cause serious complications:
- Flux
- periostitis, a pathological inflammatory process developing from the periosteum.
- Periodontitis
- inflammation of the tissue around the root of the tooth with the possible formation of purulent pockets and destruction of the periapical bone tissue.
- Pulp gangrene
(necrosis) is the death of cells in the internal tissue of the tooth.
- Sepsis
- blood poisoning that develops when microorganisms enter the general bloodstream (usually occurs with reduced immunity).
To avoid such dangerous complications, you need to visit the dentist once every six months. Patients at risk should be examined more frequently (once every three months). The risk group includes patients with diabetes, oncology and other diseases that reduce immunity. If you notice symptoms of caries, go to the doctor immediately.
Causes of acute pulpitis
- Complications of caries. Neglected or incompletely cured caries leads to the penetration of streptococci into the pulp through the dentin tubules - bacteria that have an acid-forming function and thereby create the foundation for the development of infection.
- Injuries of a mechanical or chemical nature that violate the integrity of the tooth. Without a protective layer of enamel and dentin, the pulp becomes extremely vulnerable to bacteria and the effects of the external environment.
- Gum disease in which infection spreads through open periodontal pockets.
- Unsuccessful dental treatment (infection, damage to tooth tissue, etc.).
What might you encounter after treatment?
Some patients report discomfort after filling. It is important to distinguish whether this pain is correct (post-filling) or one that requires immediate consultation with a doctor.
Mild pain is almost normal after pulpitis treatment. This is due to the fact that a serious intervention was performed, especially if inflammatory and pathological processes had previously occurred. Temporary pain occurs during the first couple of days and occurs when chewing. There is no need to go to the dentist, wait a while, the pain will go away.
The pain is sharp, intensifying and occurring throughout the week may indicate the continuation of the inflammatory process. Swelling of the gums indicates the same thing. In this case, you need to visit your dentist.
Where to contact?
The “Good Hands” dental clinic has everything necessary for successful treatment of purulent pulpitis. We employ highly qualified specialists who constantly improve their skills. They have modern equipment and effective drugs at their disposal. Treatment is carried out using gentle techniques and high-quality anesthetics, which makes it as comfortable as possible for our patients. You can schedule a free consultation with us and find out all the necessary information right now by filling out an application on our website or calling us by phone.