Halitosis or bad breath is a symptom of pathological processes occurring in the body.
According to statistics, in 80% of cases, the cause of halitosis is dental problems, 10% are diseases of the ENT organs, and 10% are diseases of internal organs.
Having felt an unpleasant odor coming from their mouth, people most often turn to a dentist for advice. Often, upon examination, it is discovered that the source of the stale smell is a tooth rotting under the crown.
The main reasons why a tooth under a crown begins to smell bad
Wearing a prosthesis longer than expected . Over time, when wearing a denture for a long time, the gum tissue atrophies, and the area of the neck of the tooth is exposed. A loose connection of the crown to the gum causes the formation of a gap into which food debris gets trapped. It is impossible to remove accumulated substrate from under the crown using traditional methods: toothbrush, rinsing. As a result, an environment favorable for the growth of bacteria is formed under the crown, which in the course of their life emit foul-smelling sulfur dioxide gases.
Violation of the seal between the crown and the tooth . The reason is most often the incorrect installation of the prosthesis or the resorption of the material that was used to fix the artificial crown to the supporting tooth. Pathogenic microflora, penetrating into the formed cavities, causes secondary caries and inflammation of the gums.
If the crown is metal-ceramic, then under the influence of salivary secretions and oxygen in the air, the metal in its composition undergoes oxidation, which causes an unpleasant odor. In addition, the resulting oxides irritate the mucous membranes of the gums and can provoke allergic reactions.
Lack of tooth protection after grinding . One of the stages of preparation for prosthetics is preparation - removal of the enamel coating, which protects tooth tissue from mechanical damage and the action of microbes. If, before installing a permanent prosthesis, the ground tooth is not covered with a temporary crown or treated with cement, then bacteria settle on it and continue their destructive activity under the prosthesis.
Violation of the technological process of manufacturing and installing a prosthesis . If a crown is installed incorrectly, regardless of the reason (insufficient experience of dental technicians and orthopedists, use of low-quality materials), soft tissue injury occurs, followed by infection and the development of inflammation.
Poor oral hygiene . Artificial structures - dentures require special care and cleaning. If you neglect the rules of hygiene, pathogenic microorganisms begin to actively multiply, causing putrefactive processes.
Poor quality dental treatment . One of the main conditions for successful prosthetics is the absence of infection in the oral cavity. If teeth that are subject to prosthetics have a defect in filling the dental canals, a granuloma or cyst filled with pus may form at the apex of the root.
When teeth affected by caries appear under the crown, the decay process continues and ends with complete destruction and death of the tooth.
What to do if a tooth is rotten
Rotten teeth - what to do? The first step is to make an appointment with a dentist and get ready for long-term treatment:
- Complete diagnostics of the oral cavity. A comprehensive X-ray examination will indicate changes in dental tissues, even if this is not visible during a routine examination.
- Identification of the main rotten areas. The doctor will determine the number of affected teeth and the stage of decay for each unit.
- Coordination of the treatment plan. Dental protocols are aimed at preserving each dental unit, so an experienced dental therapist will guide the patient towards treatment and filling cavities. If the decay process has gone very far and the root is affected, then the dental unit will have to be removed followed by prosthetics or implantation.
- Carrying out treatment. A rotten tooth usually indicates pulpitis, so the patient will have the dental nerve removed, the cavities cleared of pus, and the crown restored with high-quality composite materials.
- Professional hygiene. This is a mandatory stage in the fight against rotten teeth, so the patient will be referred for the removal of soft plaque and tartar.
- Identification of the causative agent of the pathological process. The doctor will make a smear for analysis, and after laboratory testing, will select therapy for the patient’s quick recovery.
Dental treatment of rotting units is always comprehensive, aimed at physical restoration and elimination of the causes of decay.
Symptoms of tooth decay under the crown
The first sign of an inflammatory process under a prosthesis is not pain, as many people think, but an unpleasant odor. This happens because at the stage of preparation for prosthetics, the tooth is usually depulped, that is, the neurovascular bundle, which is responsible for sensitivity, is removed.
- An unpleasant taste first appears in the mouth, then a putrid odor is added, which cannot be masked by any chewing gum or mouthwash.
- The patient discovers a gap between the crown and the gum, where food debris gets in, which becomes a breeding ground for microbes.
- Often, inflammation of the gums develops near the tooth with the formation of soft tissue swelling.
- If the tooth has not been pulped, then severe pain is present.
- Blackening of the tooth under the crown.
All these symptoms indicate an advanced putrefactive process in the tooth covered with a crown. You should immediately seek medical help from a dentist.
Ignoring the problem leads to dire consequences:
- formation of a purulent cyst at the apex of the root;
- complete tooth destruction;
- the formation of periostitis or gumboil;
- spread of purulent infection along with blood or lymph flow to other organs.
A tooth has rotted under the crown: what to do?
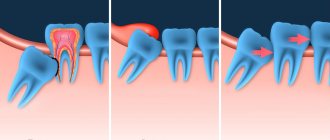
If a tooth rots under the crown, then you need to keep in mind that this process is no longer reversible. It will continue until the tooth tissue on which the crown rests rots completely, after which the crown falls out (Fig. 4). Signs that the tooth is rotting are the following symptoms:
- bad smell from under the crown,
- food getting under the crown,
- root caries is visible at the lower edge of the crown,
- the tooth under the crown has turned black (if the crown is made of metal-free ceramics, then its darkening can serve as a symptom of carious damage to the tooth tissue under the crown).
Caries of the tooth root under the crown on an x-ray (Fig. 5-6) –
The best diagnosis of this process is to contact a dentist, who will be able to detect caries even on surfaces that are difficult to inspect. The onset of carious lesions on the root surface at the lower edge of the crown can be difficult to diagnose if caries occurs on the lateral surfaces of the tooth root, i.e. in the interdental space (24stoma.ru).
In the latter case, a targeted photograph of the tooth is taken (Fig. 5-6), in which caries under the crown looks like intense darkening, unusual for healthy tooth tissue. Keep in mind that early contact with the dentist in such a situation can sometimes allow the tooth to be treated and a new crown installed. Late treatment, on the contrary, brings you closer to tooth extraction.
Tooth rotting under the crown: video
Why does the taste of blood appear in the mouth?
Inflammation of the gums under the denture is manifested not only by a specific smell from the mouth, but also by the appearance of a blood taste.
Inflammation of the gums around the crown is called gingivitis. Often the cause of gingivitis is rubbing of the mucous membrane due to the irregular shape of the prosthesis. For example, when the lower edge of the crown extends too deeply behind the gum, which leads to injury and bleeding. Blood is an excellent breeding ground for pathogenic microbes that readily multiply, causing inflammation of the soft tissue around a tooth with a poorly fitting denture.
Broken prosthesis that goes unnoticed. The bridge structures scratch the mucous membrane, leaving cuts and abrasions on it.
Bleeding is also the result of poor-quality tooth treatment before prosthetics. Against the background of inadequate filling of the dental canals or incomplete removal of the pulp, pathogenic microbes inside the tooth provoke a purulent process, which is accompanied by tissue destruction with the release of blood.
Infectious disease - when a nerve is removed
There is a small risk that a tooth after root canal treatment may become infected, like other teeth. If, after treating a tooth with root canal treatment, you notice symptoms of infection (inflammation of the gums, pain “inside the gum” or “above/below the tooth,” etc.), you should immediately contact your dentist for re-treatment.
Some precautions to take after tooth nerve removal and root canal treatment
Have you treated your tooth with root canal treatment? So you must take the following precautions. Most of these instructions apply to all people, even those unlucky enough not to have undergone a root canal procedure.
- Avoid chewing foods that are too hard, such as raw nuts, on a tooth that has had a root canal.
- Brush your teeth twice a day and use dental floss or floss.
- Don't forget to rinse your mouth after meals or snacks.
- Maintain good oral hygiene (periodically changing toothpaste, visiting the dentist for teeth cleaning)
- Get rid of bad habits such as smoking tobacco.
What to do to get rid of the smell
Some patients, even having discovered that the cause of such bad breath was a tooth rotting under the crown, for some time they hope to cope with the problem on their own: they rinse their mouth with decoctions of chamomile, calendula, and sage.
Antibacterial rinses and traditional medicine give a temporary effect and are not able to eliminate the root cause of the problem. In addition, frequent rinsing can disrupt the normal microflora of the oral cavity, when beneficial microorganisms die along with harmful ones.
It should be understood that no home remedies will stop the inflammatory process in the tooth, which will only progress and lead to its complete destruction and loss.
Symptoms and need for treatment
If the gums smell rotten, but there is no pain, a person often ignores this symptom for a long time, trying to hide the deficiency with chewing gum, lollipops, and toothpastes “for fresh breath.” However, if the problem is started, additional symptoms will arise that should not be ignored:
- swelling of soft tissues, the appearance of compactions or formations that are soft inside, and their contents gradually increase;
- fever without cold symptoms;
- sharp or aching pain radiating to the jaw and temple area;
- loss of appetite, insomnia, worsening mood;
- obvious facial asymmetry associated with edema;
- difficulties in chewing food, talking;
- loosening of teeth, exposure of roots.
It is important not to ignore these symptoms, but to consult a doctor immediately. The danger is that the smell of pus indicates infection of the areas. Fistulas can form on the mucous membranes, the rupture of which will lead to pus entering the body, which will cause serious damage to internal organs. Treatment of the problem at the initial stage will be as effective as possible, will allow you to avoid unnecessary expenses, and save teeth that can be damaged during purulent processes.
Treatment tactics vary and depend on the following factors:
- stages of tooth decay;
- the degree of spread of the inflammatory process to soft tissues;
- condition of root canals.
Treatment options for a tooth under a crown:
If the tooth stump has been preserved and has not undergone a carious process, the layers inside the crown are cleaned and, depending on the condition, it is either replaced with a new one or returned to its place after restoration.
When the upper part of the tooth is destroyed, but the roots are healthy, the stump inlay method is used. This is an orthopedic structure with “legs” that are fixed in the canals of the tooth, and an artificial crown is installed on top.
If the putrefactive process has gone too far and the tooth is completely destroyed, it is removed. As a rule, with long-term inflammation, the soft tissues surrounding the problematic tooth also suffer. Therefore, before proceeding with prosthetics, periodontitis is treated. There are two ways to restore a lost tooth: implantation or a bridge.
When choosing a dental clinic where you plan to get dentures, be sure to find out whether the medical institution provides guarantees for the treatment performed. If damage to the prosthesis occurs during the warranty period due to a medical error, treatment and restoration of the orthopedic structure is carried out free of charge.
What to do if a crown falls out -
The simplest option is when the crown falls out not because of carious destruction of the tooth tissue underneath, but because of poor cement fixation of the crown on the tooth. The main reasons for the loss in this case: mistakes by the dentist when fixing the crown with permanent cement, low clinical height of the crown (in this case, the crown will always fall out with regularity). In this case, it is enough to immediately contact your dentist to have a new crown fixed on your tooth.
1) What to do if a crown with a pin falls out -
Often, when preparing a tooth for prosthetics, a pin or stump inlay is fixed in the root canal. If your crown and pin fall out, this is again due to poor quality work by dentists. The fact is that severely damaged tooth crowns (before prosthetics with crowns) are restored by good dentists not with the help of pins, but with the help of stump inlays.
How a tooth is restored using a pin and filling -
Therefore, if the crown of your tooth was almost completely destroyed and it was restored with the help of filling material and a pin, the loss of the crown will be a pattern, because such a design is simply not able to withstand normal chewing pressure. By the way, no less often in such situations, the pins lead to a root fracture, after which the tooth is removed altogether.
If such a crown falls out, then the filling material with a pin sticking out of it remains inside the crown. Of course, it is possible to simply cement all this over again in the root canal (and we are sure that you will find dentists who will be ready to do this), but this is absolutely forbidden. Here you need to restore the tooth again - preferably with a stump tab, and then make a new crown. Otherwise, you will simply lose this tooth.
2) If the crown falls out along with the stump tab -
If a badly damaged tooth was restored not with a pin, but with a stump tab, the crown may also sometimes fall out.
This is usually also due to dentist mistakes. The fact is that after fixing the stump tab in the root canal, many dentists, saving time, begin to file it with burs within 15 minutes and take an impression. The fact is that after fixing the stump tab, a whole day must pass before you can begin to adjust it with a drill. If the adjustment is made 10-20 minutes after fixation, which some dentists like to do to save time, then vibration when processing the inlay with a drill will lead to partial destruction of the cement that has not yet fully hardened. This leads to the fact that after a week, a month or six months, the crown falls out along with the stump tab.
How a tooth is restored using a stump inlay -
What to do - unlike the situation when the tooth was restored with a filling and a pin - such a structure can still be re-fixed in the root canal (without the need to replace the crown), but only if you immediately contact the dentist.
The crown lies on the gum: what to do
Very often there are cases when inflammation of the gums begins around the artificial crown - as a result of which the gums swell, grow, and chronic inflammation is constantly maintained in this place. Most often, this is due to the fact that the crown injures the edge of the gum with its overhanging edges (which should not normally exist).
In some cases, the problem can be solved by surgical adjustment of the gingival margin, i.e. when part of the gum near the crown is removed. But according to the rules, the overhanging edge of the crown, which injures the gingival margin, is a warranty case, and you have the right to demand a replacement of the crown (if the warranty period has not yet expired, which is usually 1 year). We hope that our article was useful to you!
Sources:
1. Personal experience as a dentist, 2. “Orthopedic dentistry. Textbook" (Trezubov V.N.), 3. "Orthopedic treatment with fixed prostheses" (Rozenshtil S.F.).
What to do if the tooth under the crown has completely rotted
One type of reconstruction of a severely damaged tooth is a stump inlay. It is a product that replicates the root system of the tooth. A crown is placed on the upper part of the structure protruding above the gum. The method is used only if there are healthy, undamaged roots.
Stump inlays are made of chrome-plated cobalt or alloys with precious metals (gold, silver). Preference is given to gold, as its shade resembles the color of natural enamel. The silver tab, despite its antibacterial effect, is used less frequently, since it shows through the crown as a dark spot.
If the roots are completely rotten and cannot be restored, the tooth is removed.
The choice of one or another method of dentition restoration in case of tooth loss remains with the patient, and his wishes regarding the material, type of structure, as well as financial capabilities are taken into account.
What to do if a crown falls off
The reasons why a crown falls off a tooth can be very diverse:
- With prolonged use, the cement on which the crown was strengthened dissolves.
- Secondary caries, leading to the destruction of the tooth stump and a violation of the tightness of the connection between the tooth and the crown.
- Damage to the denture due to heavy load when chewing solid food.
You cannot try to put the crown in its original place on your own and continue to use the prosthesis. This is very dangerous, since the crown, unexpectedly jumping off the tooth, can enter the windpipe and cause suffocation.
It is impossible to properly strengthen the prosthesis at home; only a dentist can do this.
The dentist, after examination and diagnosis, will decide what to do next.
There are several options:
- If the crown is only slightly damaged, it can be repaired and replaced.
- In case of significant damage or if the service life of the orthopedic structure has come to an end, the prosthesis must be replaced.
- If the cause of crown loss is caries, the tooth is treated, and then a decision is made about the possibility of prosthetics.
- If a tooth is severely damaged and cannot be restored, it is removed, and then implantation or a bridge is installed.
Rules for caring for fixed dentures
High-quality care of crowns in compliance with all hygienic rules can significantly extend the service life of the product.
Since a regular toothbrush is not able to fully clean all hard-to-reach places, additional care products are used to better treat teeth and dentures.
Dental floss (floss). This is a special thread made of nylon, silk, acetate fibers with a flat or round cross-section, designed to clean interdental spaces. To enhance the effect, they are often impregnated with antiseptics.
Floss - disposable toothpicks with a thread on a frame are used for the same purposes as floss.
Bundle brush . The interdental spaces are cleaned using a brush-brush with many long bristles. Dentists recommend alternating cleaning the spaces between teeth with brushes and dental floss, since some of them (floss) are better suited for narrow gaps, and a tuft brush does an excellent job of cleaning wide gaps.
An interproximal brush with a brush is designed to treat hard-to-reach areas between the crown and adjacent teeth.
An irrigator is a device for cleaning the oral cavity using a water jet supplied under pressure. A pulsating stream of water penetrates into the most inaccessible places, cleanses the surface of teeth and artificial dentures from plaque and food debris in the gum pockets and interdental spaces.
Dentists do not recommend using wooden toothpicks at all. Wood particles get stuck between the teeth, begin to rot and cause inflammation. In addition, toothpicks can easily injure your gums without even noticing it.
Preventive crown care
The prosthesis installed in the mouth is influenced by food chemicals, saliva, and microbes. Without systematic proper care of crowns, they become covered with plaque, lose their original color, and become a breeding ground for infection.
Prevention of the development of infection in the oral cavity, especially under fixed dentures, involves strict adherence to the following hygiene rules:
- Teeth should be brushed at least 2 times a day: morning and evening, and if possible, more often. Brushing technique: movements of the toothbrush are performed from the gum to the top of the tooth at an angle of 45°. The procedure time is at least 3 minutes.
- Rinse your mouth with clean water after every meal.
- For better cleaning of teeth and dentures, it is recommended to actively use additional devices: interproximal and tuft brushes, dental floss.
- Use irrigators. To rinse the oral cavity, various agents with an antibacterial effect are used that destroy pathogenic microorganisms.
A well-installed prosthesis with good care will reliably and for a long time protect the tooth from external factors. But if a tooth infection does occur and decay begins, without proper treatment the pathological process will only progress, which will lead to serious complications. To eliminate the consequences, long-term treatment with significant financial costs will be required.
Main reasons
Unpleasant odor from the gums is often associated with caries or pulpitis. When a tooth begins to deteriorate, an unpleasant taste appears in the mouth, as well as a putrid odor that does not go away even after brushing the teeth, using a mouthwash, or eliminating foods with strong aromatic properties from the diet. A similar problem can arise with periodontitis, a disease that affects not only the incisors, but also soft tissues. They begin to fester, causing the above symptoms.
If the patient rarely goes to the doctor for examination, it is possible that the gums smell bad due to the presence of a large amount of tartar. Even the most thorough, regular brushing of your teeth will not help to completely get rid of plaque that forms from food debris along with bacteria settling on mucous surfaces. Gradually they accumulate, harden, and begin to put pressure on adjacent tissues, causing their damage. Infection enters small cracks, which leads to rotting processes.
Sometimes the gums fester due to the fact that pathogenic microflora has penetrated through wounds from dentures and braces. Dentists usually tell patients that during the first few days they may experience not only discomfort in the area affected by the structures, but also small scratches and cracks, since the soft tissues have not yet become accustomed to the new condition. Since the likelihood of infection is extremely high, it is recommended to rinse the mouth with special solutions. But patients often ignore this fact, which leads to infection of the damaged areas.
The presence of chronic ailments associated with pathologies in the functioning of internal organs is another common reason. The mucous membranes are quite sensitive to all processes that occur in the body. Therefore, if there are disturbances in the functioning of the liver, stomach, intestines, kidneys, an unpleasant odor appears. The main task is to eliminate the irritating factor, which will lead to the disappearance of the problem.