From this article you will learn:
- what is dental pulp and its functions,
- structure and architectonics of pulp layers,
- histological preparations.
Dental pulp (pulpa dentis) is a specialized type of loose fibrous connective tissue rich in blood vessels and nerve fibers that fills the cavity of the tooth, i.e. pulp chamber and root canals. Due to the presence of a large number of receptor nerve endings in it, the pulp provides very high pain sensitivity of tooth tissue to the effects of mechanical, physical, and chemical stimuli.
Inflammation of the pulp (pulpitis) most often develops as a result of pathogenic bacteria entering it. This occurs when the carious process spreads to the deep layers of dentin surrounding the pulp chamber, but in some cases the cause of inflammation can be physical trauma to the tooth or a thermal burn (for example, due to errors when preparing a tooth for a crown). Most often, pulp inflammation occurs acutely, with severe pain, but in some cases the course can be asymptomatic - with a predominance of hyperplastic processes.
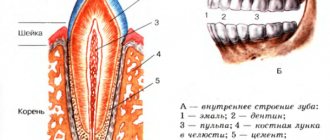
Structure of the dental pulp (diagram) –
Due to the abundance of blood vessels in the pulp, as well as due to the presence of narrow apical openings at the apexes of the roots, with the development of acute pulpitis, inflammatory edema always increases rapidly. Since the volume of the pulp is limited by the walls of the pulp chamber, inflammatory edema leads to compression of the veins and lymphatic vessels, thereby disrupting the outflow of fluid. This leads to the development of necrosis and death of the pulp. In addition, swelling also leads to compression of nerve endings, which actually causes the development of acute pain.
It should be noted that the dental pulp contains entire nerve plexuses, including a large number of receptors that are capable of perceiving stimuli of any kind - pressure, temperature, chemical and physical influences. But at the same time, effector nerve endings are also described in the pulp. Part of the nerve fibers of the pulp (together with the processes of odontoblasts) exits it into the predentin and the inner zone of the peripulpal dentin, located in the dentinal tubules.
The structure of the dental pulp –
Speaking about the structure of the dental pulp, we will first analyze its structural elements - after which we will move on to a description of its layers, which you could see in Fig. 2. You can see the appearance of the pulp removed from the tooth (wound on a pulp extractor) in the photo below.
Video of tooth pulp removal (pulpectomy) –
1) Structural elements of pulp –
The pulp consists of loose fibrous connective tissue (with a large number of nerve endings, blood and lymphatic vessels). Accordingly, its structure will consist of collagen fibers, the main amorphous substance, as well as a large number of various cellular elements. The total collagen content is from 25 to 30% of the dry mass of the dental pulp, and it is mainly collagen types I and III. In the coronal part of the pulp, collagen fibers are located more loosely, but in its root part they form denser clusters.
As for the main amorphous substance located between the collagen fibers, it consists of water, glycosaminoglycans, as well as glycoproteins and proteoglycans. The intercellular substance has a high ability to diffusion, which allows nutrients from the blood to enter the cellular elements, and metabolic products to be excreted into the venous circulatory system. There is also a wide variety of cellular elements in the pulp - primarily odontoblasts and fibroblasts (fibroblasts are responsible for the formation of intercellular substance and the synthesis of collagen fibrils), as well as dendritic cells, macrophages, lymphocytes, mast cells, etc.
Cellular elements of the pulp -
| Cells | Odontoblasts – form dentin and provide its trophism. Neighboring odontoblasts are interconnected by intercellular connections, which allows the layer of odontoblasts to also perform a barrier function (regulating the movement of molecules and ions between the pulp and predentin). Some authors call these cells “dentinoblasts.” |
| Fibroblasts are the most numerous cells in the pulp (their number decreases with age). Their function is to produce and maintain the composition of the intercellular substance of the pulp, as well as to absorb and digest the components of the intercellular substance. | |
| Macrophages - participate in the renewal of the cellular composition of the pulp, capturing and digesting dead cells and components of the intercellular substance. They phagocytose microorganisms and participate in the development of immune reactions as antigen-presenting effector cells. | |
| Dendritic cells – they are antigen-presenting cells whose function is to absorb various antigens, process them and present them to lymphocytes. They also induce the proliferation of T lymphocytes. The content of dendritic cells increases as the pulp matures, as well as with antigenic stimulation. | |
| T-lymphocytes are contained in the pulp in small quantities, but during inflammation their number increases sharply (of all types of this population of lymphocytes, T-suppressors predominate in the pulp). B-lymphocytes are not normally found in the pulp, and appear only when it is inflamed (they synthesize IgG immunoglobulins and provide humoral immune responses). | |
| Mast cells – they are located around blood vessels; are characterized by the presence in the cytoplasm of a large number of granules with biologically active substances (histamine, heparin, eosinophilic chemotactic factor, etc.). The release of these components causes an increase in vascular permeability. | |
| Poorly differentiated cells - can give rise to odontoblasts and fibroblasts. The content of these cells decreases markedly with age. | |
| Fibers and glycoproteins | Type I and III collagen fibers, reticular fibers, fibronectin. |
| Basic intercellular substance | Glycosaminoglycans, chondroitin, proteoglycan. |
Arteries of the tooth
The supply of nerves and blood to the jaws depends on the nerves and blood vessels that supply them. The upper jaw is considered to be part of the middle zone of the face, and the lower jaw is the lower part of the face, respectively, they have a separate blood supply. Although in the alveolar bone the maxillary and mandibular nerves and vessels are mirrored in relation to each other, there are anatomical differences with additional branches and adjacent structures such as the mandibular mental foramen or the greater palatine foramen in the hard palate.
How are teeth supplied with blood?
The maxillary arterial vessel supplies the deep structures of the face, including the teeth. Branching from the external carotid arterial vessel, it approaches the neck of the mandible. The superior alveolar arterial vessels (anterior and posterior) supply the upper teeth. Smaller branches extend from these vessels, providing blood supply to the teeth, gums and socket walls. A branch of the inferior alveolar arterial vessel supplies the lower teeth, located in the mandibular canal, where it forms dental and interalveolar branches. Through the tops of the foramina, dental arterial vessels enter the root canals of the teeth and then branch into the dental pulp.
All arteries are accompanied by veins of the same name, which are responsible for draining blood from the teeth into the pterygoid venous plexus.
Arteries responsible for blood supply to teeth
- Maxillary artery. From a topographical point of view, the maxillary artery has three parts: mandibular, pterygoid and pterygopalatine. The maxillary artery is the large terminal branch of the external carotid artery. Starting below the temporomandibular joint, it runs along the outer or inner side of the lateral pterygoid muscle, after which it branches in the pterygopalatine fossa.
- Inferior alveolar arterial vessel. It lies between the medial pterygoid muscle and the branch of the mandible. Then it goes along the mandibular bone canal, reaching the mental foramen.
- Dental branches. Suitable for tooth roots.
- Masticatory arterial vessel. It goes above the notch of the lower jaw and supplies blood to the muscle of the same name.
- Mylohyoid branch. It originates near the opening of the lower jaw and, together with the mylohyoid muscle, runs in the groove of the same name. This branch connects to the mental arterial vessel.
- Buccal arterial vessel. Located in the buccal muscle. Responsible for blood supply to the cheeks and gums.
- Posterior superior alveolar artery. Entering its branches into the alveolar canals, it supplies blood to the upper molars, gums and mucous surface of the maxillary sinus.
Architectonics of dental pulp layers –
In the coronal part of the pulp, there are several layers that differ in their structure and functions - 1) the outer layer, consisting of odontoblasts, 2) the subodontoblastic layer, which in turn consists of several zones, including the Weil and Rinaggio zones, as well as the Rashkov plexus, 3) central pulp zone. Below we will analyze in detail the structural components of each layer.
Architectonics of dental pulp layers (diagram) –
- The outer layer (peripheral) - consists of several layers of odontoblasts, which are elongated cells with basophilic cytoplasm (24stoma.ru). In “young teeth” the pulp may contain 6-8 layers of odontoblasts, but the older a person gets, the fewer the number of layers will be (at least one layer). Odontoblasts are highly differentiated cells that are specific to the dental pulp.
Long processes (the so-called “Toms fibers”) extend from the odontoblasts, which penetrate the dentinal tubules to the entire depth of the dentin. Odontoblasts and their processes play a very important role in the nutrition of the tooth and the delivery of mineral salts to the dentin and to the enamel-dentin border. In addition, they perform the function of dentin synthesis both during the period of tooth development and throughout a person’s life (we are talking about the synthesis of secondary and tertiary dentin). In the root part of the pulp, a layer of odontoblasts is also present, but it is thinner than in the coronal part of the pulp.Odontoblasts are closely connected to each other by strong intercellular connections, but capillary loops penetrate through their layer, as well as the finest nerve fibers (branches from the Rashkov plexus). These nerve fibers form tree-like branches around the odontoblasts - they are often called the “superodontoblastic nerve plexus”. It is interesting that part of the nerve fibers will end around the odontoblasts, but the other part will be directed along with the processes of the odontoblasts into the dentinal tubules.
- Subodontoblastic layer - morphologically it is usually divided into 2 zones.
The first zone is the more superficially located “light Weil zone” (a layer poor in cell nuclei). This zone mainly consists of collagen fibers, as well as cell processes penetrating from the inner zone of the subodontoblastic layer. This layer contains a large number of capillaries, which form an extensive capillary plexus that nourishes both odontoblasts and the pulp as a whole. Also in this layer there are many myelinated and unmyelinated nerve fibers, forming the so-called Rashkov nerve plexus. The deeper zone of the subodontoblastic layer is the Rinagio zone (a zone rich in cellular elements). This zone consists of a large number of diverse cellular elements, for example, poorly differentiated cells are located here, which can give rise to odontoblasts and fibroblasts. In addition, fibroblasts themselves, lymphocytes, as well as capillaries and nerve fibers are located in this layer.
- The central zone of the pulp is a loose fibrous connective tissue rich in cells (primarily fibroblasts and macrophages). Also contains larger blood and lymphatic vessels, and larger bundles of nerve fibers. In the central zone of the pulp, dendritic cells, lymphocytes, plasma cells, mast cells, and blood granulocytes are constantly present in small quantities.
Summary: below, for convenience, we have arranged the structural elements of the pulp layers - in the form of a single table. Once again, we draw your attention to the fact that the intermediate (subodontoblastic) layer is well developed only in the coronal part of the pulp.
| Peripheral layer | Intermediate layer | Central layer | |
| outer zone (Reil) | inner zone (Rinagio) | ||
| – odontoblasts, – Toms’ processes, – capillary loops, – nerve fibers. | – processes of cells of the inner zone of the intermediate layer, – collagen and reticular fibers, – Rashkov’s nerve plexus. | – fibroblasts, – lymphocytes, – preodontoblasts, – poorly differentiated cells, – capillaries, – myelinated and non-myelinated fibers. | – PBST *, – large blood and lymphatic vessels, – bundles of nerve fibers. |
* PBCT is loose fibrous connective tissue.
Histological specimen (dental pulp and peripulpal dentin) –
Where 1 is dentin (where 1a is calcospherites, 1b is predentin). Where 2 is the dental pulp (where 2a is the peripheral layer consisting of odontoblasts, 2b is a cell-poor zone in the intermediate pulp layer, 2c is a cell-rich zone in the intermediate pulp layer, 2d is the central pulp layer).
Ultramicroscopic structure of odontoblast –
Above you can see what an odontoblast looks like with a branched process, which will be located in dentin and predentin (where 1 is dentin, 2 is predentin, 3 is an odontoblast process located in the dentinal tubule, 4 is the Golgi complex, 5 is the nucleus, 6 is mitochondria, 7 – endoplasmic reticulum.).
Differences between the coronal and root parts of the pulp -
The root part of the pulp has significantly weaker vascularization and innervation compared to the coronal part of the pulp. In addition, the cellular composition of the root part of the pulp is much poorer, and the odontoblast layer, even in the “young pulp,” has only 1-2 rows of cells. Apparently, such differences in structure depend on the characteristics (differences) in the supply of nutrients and calcium salts - in the crown and root parts of the tooth.
In the coronal part, dentin and enamel receive nutrients and calcium salts - almost exclusively from the dental pulp. As for the nutrition of the hard tissues of the tooth root, it occurs not only through the pulp, but also due to the process of diffusion of nutrients from the pericement. Therefore, evolutionarily, a decrease in the importance of root pulp in the nutrition of hard tissues of the tooth root has been formed, and its structure has changed.
| Coronal pulp: | Root pulp: |
|
|
Pulp histology: video
Below in video 1 you can see the histology of tooth tissue in stunning resolution. Video 2 is the best lecture on pulp histology you will ever hear. The video is in English, but if you wish, you can turn on subtitles and select translation from English into Russian in the settings.
Features of the structure of the pulp of temporary teeth -
The structure of the pulp in baby teeth differs little from permanent ones. For example, in baby teeth there are fewer differences in the structure of the coronal and root parts of the pulp, and in addition, the pulp in baby teeth is more abundantly supplied with blood. There are also slight differences in the composition of cellular elements and the number of collagen fibers (Fig. 3).
5.1. Innervation of teeth and jaws
12
ANATOMICAL FEATURES OF THE STRUCTURE AND INNERVATION OF THE MAXILLOFACIAL AREA. GENERAL AND LOCAL ANESTHESIA IN DENTISTRY. Innervation of teeth and jaws. General anesthesia. Local anesthesia. Anesthetics used for local anesthesia. Instruments for anesthesia.
Most dental procedures are accompanied by a painful reaction. It is no coincidence that pain relief was first used in dentistry. Modern dentistry involves the use of anesthesia when performing any dental intervention.
There are general (anesthesia, neuroleptanalgesia) and local anesthesia. A combination of them is possible. To properly perform pain relief, it is first necessary to know the features of the anatomical structure and innervation of the maxillofacial area.
The teeth and jaws are innervated by motor and sensory nerves.
Sensory nerves: trigeminal, glossopharyngeal, vagus and nerves coming from the cervical plexus (greater auricular and lesser occipital) - innervate the skin of the face, soft tissues and organs of the oral cavity, jaw. (SL Sineln T3, P.143, fig. 819) In the face area along the branches of the trigeminal nerve there are five vegetative nodes: 1) ciliary (gangl. ciliare); 2) pterygopalatine (gangl. pterigopalatinum); 3) ear (gangl. oticum); 4) submandibular (gangl. submandibulare); 5) sublingual (gangl. sublinguale). The ciliary ganglion is connected to the first branch of the trigeminal nerve, the pterygopalatine ganglion is connected to the second branch, and the auricular, submandibular and sublingual vegetative ganglia are connected to the third branch.
Sympathetic nerves to the tissues and organs of the face come from the superior cervical sympathetic ganglion.
(SL Sineln. T3, P.135, Fig. 812) Trigeminal nerve (p. trigeminus) mixed. It contains motor, sensory and parasympathetic secretory nerve fibers. The branches of this nerve provide mainly sensory innervation of the organs and tissues of the oral cavity. Three branches depart from the trigeminal ganglion: 1) the optic nerve (n. ophthalmicus), sensitive; does not take part in the innervation of the jaws and oral tissues; 2) maxillary (p. maxillaris); 3) mandibular (p. mandibularis).
The maxillary nerve is sensitive, leaves the cavity of the skull through the round opening (foramen rotundum) and goes to the pterygopalatine fossa (fossa pterigopalatinum), where it gives off several branches: the infraorbital nerve (p. infraorbitalis), the posterior superior alveolar branches (rr. alveolares, superiores posteriores) , middle alveolar branch (r. alveolaris superior medius), anterior superior alveolar branches (rr. alveolares). In addition, the zygomatic nerve (n. zygomaticus), pterygopalatine nerves (nn. pterigopalatini) and palatine nerves (nn. palatine) depart from the maxillary nerve. Let us consider the anatomical and topographical features of each of them in more detail.
The infraorbital nerve (n. infraorbitalis) is a continuation of the maxillary nerve. From the pterygopalatine fossa through the inferior orbital fissure it enters the orbit, where it lies in the infraorbital groove (sulcus infraorbitalis), and through the infraorbital foramen (foramen infraorbitalis) it exits the orbit. It then divides into terminal branches that form the minor crow's foot (pes anserinus minor), which branches in the skin and mucous membrane of the upper lip, lower eyelid, infraorbital region, wing of the nose and the skin of the nasal septum. In the pterygopalatine fossa, the posterior superior alveolar branches (rr. alveolares superiores posteriores) extend from 4 to 8 from the infraorbital nerve. A minority of them are not included in the thickness of the bone tissue, but spread down the outer surface of the tubercle of the upper jaw towards the alveolar process . The branches end in the periosteum of the upper jaw, adjacent to the alveolar process, in the mucous membrane of the cheek and gums on the vestibular side at the level of the molars and premolars of the upper jaw. Most of the posterior superior alveolar branches enter through the openings on the surface of the maxillary tubercle into the bone canals of the upper jaw, taking part in the formation of the posterior section of the superior dental plexus. These nerves innervate the tubercle of the maxilla, the mucous membrane of the maxillary sinus, the molars of the maxilla, the mucous membrane and periosteum of the alveolar process in the area of these teeth on the vestibular side. The posterior superior alveolar branches take part in the formation of the posterior section of the superior dental plexus.
In the pterygopalatine fossa, less often in the posterior part of the infraorbital groove, the middle superior alveolar branch (m. alveolaris superior medius) departs from the infraorbital nerve. It passes through the thickness of the anterior wall of the upper jaw and branches in the alveolar process. This branch takes part in the formation of the middle section of the superior dental plexus and has anastomoses with the anterior and posterior superior alveolar branches. The middle upper dental plexus innervates the bone tissue of the anterior wall of the upper jaw, the alveolar process, the premolars of the upper jaw, the mucous membrane of the alveolar process and the gums on the vestibular side in the area of these teeth.
In the anterior section of the infraorbital canal, the anterior superior alveolar branches (alveolares superiores anteriores) - 1-3 trunks - depart from the infraorbital nerve. These branches form the anterior section of the superior dental plexus. They innervate the incisors and canines, the mucous membrane and periosteum of the alveolar process, and the mucous membrane of the gums on the vestibular side in the area of these teeth. The nasal branch departs from the anterior alveolar branches to the mucous membrane of the anterior floor of the nose, which anastomoses with the nasopalatine nerve. The posterior, middle and anterior superior alveolar branches, passing through the thickness of the walls of the upper jaw, anastomose with each other, form the superior dental plexus (plexus dentalis superior). It anastomoses with the same plexus on the other side. The plexus is located in the thickness of the alveolar process of the upper jaw along its entire length above the apices of the roots of the teeth and near the mucous membrane of the maxillary sinus.
A number of branches depart from the upper dental plexus: a) dental (rr. dentales) to the dental pulp; b) periodontal and gingival (gg. periodontales et gingivales), innervating the periodontium and gum tissue; c) interalveolar, going to the interalveolar septa, from which branches extend to the periodontium of the teeth and the periosteum of the jaw; d) to the mucous membrane and bone walls of the maxillary sinus. From the infraorbital nerve, as it exits the infraorbital foramen, the lower branches of the eyelids (palpebrales inferiores) depart, which innervate the skin of the lower eyelid; external nasal branches (rr. nasales externi); internal nasal branches (rr. nasales interni), innervating the mucous membrane of the vestibule of the mouth; superior labial branches (rr. labiales superiores), innervating the skin and mucous membrane of the upper lip to the corner of the mouth. These branches have connections with the branches of the facial nerve.
In the pterygopalatine fossa, the zygomatic nerve (n. zygomaticus) departs from the maxillary nerve, which penetrates the orbit through the lower orbital fissure, where it divides into 2 branches - the zygomaticofacial (r. zigomaticofacialis) and the zygomaticotemporal (r. zigomaticotemporalis). These branches enter the thickness of the zygomatic bone through the zygomaticotemporal foramen (foramen zigomaticoorbitale), and then exit it, branching in the skin of the zygomatic region, the upper part of the cheek and the outer corner of the palpebral fissure, the anterior part of the temporal and posterior part of the frontal areas. The zygomatic nerve has connections with the facial and lacrimal nerves.
The pterygopalatine nerves (nn. pterigopalatini) depart from the lower surface of the maxillary nerve in the pterygopalatine fossa. They go to the pterygopalatine ganglion, giving sensory fibers to the nerves starting from it. The pterygopalatine ganglion (gang. pterigopalatinum) is a formation of the autonomic nervous system. It receives parasympathetic fibers from the ganglion (gang, geniculi) of the facial nerve in the form of the greater petrosal nerve (n. petrosus major). The node receives sympathetic fibers from the sympathetic plexus of the internal carotid artery in the form of the deep petrosal nerve (p. petrosus profundus). Passing along the pterygopalatine canal, the large and deep petrosal nerves unite and form the nerve of the pterygoid canal. Branches depart from the node, including secretory (parasympathetic, sympathetic) and sensory fibers: orbital (rr. orbitales), upper and lower posterior nasal branches (rr. nasales posteriores superiores et inferiores), palatine nerves. The orbital branches branch in the mucous membrane of the posterior cells of the ethmoidal labyrinth and the sphenoid sinus.
The superior posterior nasal branches (rr. nasales posteriores superiores) enter the nasal cavity from the pterygopalatine fossa through the foramen sphenopalatinum and are divided into 2 groups - lateral and medial. The lateral branches branch in the mucous membrane of the posterior sections of the superior and middle nasal concha and nasal passages, the posterior cells of the ethmoid sinus, the upper surface of the choanae and the pharyngeal opening of the auditory tube. The medial branches branch in the mucous membrane of the nasal septum. The largest of them - the nasopalatine nerve (p. nasopalatinus) - runs between the periosteum and the mucous membrane of the nasal septum down and forward to the incisive canal, where it anastomoses with the nerve of the same name on the other side and through the incisive opening enters the hard palate. Passing along the incisive canal, sometimes before entering it, the nerve gives a series of anastomoses to the anterior part of the dental plexus. The nasopalatine nerve innervates the anterior mucous membrane of the triangular-shaped hard palate from canine to canine.
The lower posterior lateral nasal branches (rr. nasales poteriores inferiores laterales) enter the greater palatine canal (canalis palatinus major) and exit from it through small openings. They penetrate the nasal cavity, innervating the mucous membrane of the inferior turbinate, lower and middle nasal passages and the maxillary sinus. Motor fibers travel from the facial nerve through the greater petrosal nerve.
The palatine nerves (nn. palatini) go from the pterygopalatine ganglion through the greater palatine canal. These include the greater palatine nerve and the lesser palatine nerves.
The greater palatine nerve (n. palatinus major) is the largest branch, enters the hard palate through the greater palatine foramen, where it innervates the posterior and middle sections of the mucous membrane of the hard palate (up to the canine), minor salivary glands, the mucous membrane of the gums on the palatine side, partially mucous membrane of the soft palate.
The lesser palatine nerves (nn. palatini minores) exit through the lesser palatine foramina. They branch in the mucous membrane of the soft palate and palatine tonsil. In addition, they innervate the muscle that lifts the soft palate and the muscle of the uvula (m. levator veli palatini, m. uvulae).
The mandibular nerve (p. mandibularis) is the third branch of the trigeminal nerve - mixed. (SL Sineln. T3, P.141, Fig. 816) It contains sensory and motor fibers, exits the cranial cavity through the foramen ovale and branches into a number of branches in the infratemporal fossa. Nodes of the autonomic nervous system are associated with some of its branches: with the internal pterygoid nerve and auriculotemporal - the auricular node (gangl. oticum), with the lingual nerve - the submandibular (gangl. submandibulare); The hypoglossal node (gangl. sublingualis) is connected to the hypoglossal nerve (gangl. sublingualis) by a branch of the lingual nerve. From these nodes postganglionic parasympathetic secretory fibers go to the salivary glands and gustatory fibers to the taste buds of the tongue. Sensory nerves make up the majority of the mandibular nerve. Motor fibers from the third branch of the trigeminal nerve go to the muscles that lift the mandible (muscles of mastication).
The masticatory nerve (p. massetericus) is predominantly motor; it often has a common origin with other nerves of the masticatory muscles. Having separated from the main trunk, the masticatory nerve goes outward under the upper head of the lateral pterygoid muscle, then along its outer surface and through the notch of the mandible it enters the masticatory muscle. Branches extend from the main trunk to muscle bundles. Before entering the muscle, the masseteric nerve gives off a thin sensory branch to the temporomandibular joint.
Motor nerves of the same name extend from the main trunk to other groups of masticatory muscles. The temporal muscle is innervated by the deep temporal nerves (nn. temporales profundi), the lateral and medial pterygoid muscles are innervated by the nerves of the same name (nn. pterigoidei lateralis et medialis). The mylohyoid muscle and the anterior belly of the digastric muscle are innervated by the mylohyoid nerve (n. mylochyoideus).
The following sensory nerves arise from the mandibular nerve. The buccal nerve (p. buccalis) is directed downward, forward and outward. Separating below the foramen ovale from the main trunk, it passes between the two heads of the lateral pterygoid muscle to the inner surface of the temporal muscle, then, passing at the anterior edge of the coronoid process, at the level of its base it branches along the outer surface of the buccal muscle to the corner of the mouth, in the skin and mucous membrane of the cheek , in the skin of the corner of the mouth. The nerve gives off branches to the area of the mucous membrane of the gums of the lower jaw (between the second small and second large molars). Has anastomoses with the facial nerve and ear ganglion.
The auriculotemporal nerve (p. auriculotemporalis) contains sensory and presympathetic secretory fibers. Separating under the foramen ovale, it runs backward along the inner surface of the lateral pterygoid muscle, then goes outward, bending around the neck of the condylar process of the mandible from behind. Then it goes upward, penetrating through the parotid salivary gland, approaches the skin of the temporal region, branching into terminal branches.
The lingual nerve (n. lingualis) begins near the foramen ovale at the same level as the inferior alveolar nerve. Located between the pterygoid muscles. At the upper edge of the medial pterygoid muscle, the tympanic chord (chorda tympani), which contains secretory and taste fibers, joins the lingual nerve. Next, the lingual nerve passes between the inner surface of the lower jaw and the medial pterygoid muscle, then over the submandibular salivary gland, bending around the outside and below the excretory duct of this gland, and is woven into the lateral surface of the tongue. In the oral cavity, the lingual nerve gives off a number of branches: branches of the isthmus of the pharynx, hypoglossal nerve, lingual branches. The lingual nerve innervates the mucous membranes of the pharynx, sublingual region, lower jaw on the lingual side, anterior 2/3 of the tongue, sublingual salivary gland and papillae of the tongue.
The inferior alveolar nerve (p. alveolaris inferior) is mixed and is the largest branch of the mandibular nerve. Its trunk lies on the inner surface of the external pterygoid muscle behind and lateral to the lingual nerve. It passes through the pterygomaxillary cellular space formed by the lateral and medial pterygoid muscles. Through the mandibular foramen (foramen mandibulare), the nerve enters the mandibular canal (canalis mandibularis) and gives off branches, which, anastomosing among themselves, form the lower dental plexus (plexus dentalis inferior), located slightly above the main trunk. The lower dental and gingival branches extend from it to the teeth, the mucous membrane of the alveolar part and the gums of the lower jaw on the vestibular side. At the level of small molars, a large branch departs from the lower alveolar nerve - the mental nerve (n. mentalis), which exits through the mental foramen and innervates the skin and mucous membrane of the lower lip, the skin of the chin. The section of the inferior alveolar nerve, located in the thickness of the bone in the area of the canine and incisors, after the departure of the mental nerve, is called the incisive branch of the inferior alveolar nerve (g. incisivus n. alveolaris inferioris). The incisive branch innervates the canine and incisors, the mucous membrane of the alveolar part and the gums on the vestibular side in the area of these teeth. It anastomoses with the branch of the same name on the opposite side in the midline region. From the inferior alveolar nerve, before it enters the mandibular canal, a motor branch departs - the mylohyoid nerve (n. mylohyoideus), which innervates the muscle of the same name.
Blood supply to the dental pulp -
Blood circulation and innervation of the pulp are carried out thanks to dental arterioles, venules and nerve branches of the corresponding arteries and nerves of the jaws. For example, the pulp of the teeth of the upper jaw is supplied with blood from the superior alveolar artery, and the pulp of the teeth of the lower jaw - from the inferior alveolar artery. Branching off from the main vascular nerve trunk, the neurovascular bundles penetrate into the tooth cavity through the apical openings located at the apices of the roots and then break up into smaller branches.
However, vessels can enter not only through the apical openings at the root apices, but also through the openings of accessory canals on the lateral walls of the root. These holes may have clinical significance because... through them, infection can penetrate from the deep periodontal canals into the dental pulp (and vice versa). Thus, arterioles with a diameter of 50-150 microns penetrate through the openings of the tooth root and occupy the central part of the coronal and root pulp. In turn, smaller precapillary arterioles (10–12 µm in diameter) depart from the arterioles, which form an extensive capillary plexus in the Weil layer.
Pulp blood circulation diagram –
Capillaries with a diameter of 8-10 microns are usually divided into two groups. The first group is fenestrated capillaries (about 30%), which are located mainly near the odontoblast layer. Their presence facilitates the rapid transport of nutrients to odontoblasts, which is necessary especially during the period of active dentin formation (dentinogenesis). Upon completion of tooth eruption, the number of these capillaries decreases significantly.
The second group of capillaries are the so-called somatic capillaries (about 70% of them). Both types of capillaries provide nutrition to all structural components of the pulp. Moreover, the volume of the capillary bed can vary greatly, which is facilitated by the presence of a large number of collapsed capillaries (they begin to function only during inflammation), as well as arteriole-venular anastomoses. The latter provide the ability to discharge blood from the arterial into the venous (without the participation of capillaries).
From the capillary network in Weil's zone, blood flows into muscle-type venules (they contain smooth myocytes in the wall), which subsequently exit the pulp through the apical openings at the apexes of the roots. Moreover, venules are located more centrally in the pulp, while arterioles are located more peripherally. A unique feature of the blood circulation in the pulp is that the efferent venules have a smaller diameter than the arterioles entering the pulp. Therefore, even in the absence of inflammation in the pulp there are always phenomena of hyperemia and blood stasis.
Moreover, this same feature is very high intrapulpal pressure (about 20–30 mm Hg), which is much higher compared to interstitial pressure in other organs. All this ensures a fairly slow rate of blood flow through the pulp, and apparently is important for the nutrition of tooth tissue (trophic function of the pulp).
Lymphatic vessels of the dental pulp -
Lymphatic capillaries begin in the peripheral and middle layers of the pulp - in the form of sacs with a diameter of 15 to 50 microns.
They are distinguished by several features - first of all, a thin endothelial lining (with wide gaps between endothelial cells of more than 1 micron), as well as the absence of a basement membrane over a larger extent. Lymphatic capillaries are surrounded by a thin network of reticular fibers. With traumatic or inflammatory swelling of the pulp, lymphatic drainage increases. This is manifested by an increase in the diameter of the lymphatic capillaries, and a sharp widening of the gaps between endothelial cells also occurs (plus a sharp drop in the content of micropinocytotic vesicles in them). Further, through the lymphatic capillaries, the lymph flows into thin-walled collecting lymphatic vessels.
Material and methods
The work is based on the study of 130 isolated NP preparations removed from corpses in Tver morgues, and 20 embalmed corpses of people aged 20 to 70 years, studied at the Department of Topographic Anatomy and Operative Surgery of the TSMA.
The following methods were used: morphometric measurements, contrast radiography, decalcification, preparation, recording and photography. Using 16 NP preparations, experimental ligations of the inferior alveolar artery in the initial part of the mandibular canal were performed to identify additional intraosseous arteries involved in the blood supply to the NP.
For contrast angiography, injections were made through the external carotid or inferior alveolar artery of lead, diluted in petroleum jelly and turpentine in the following ratio: lead - 60 g, petroleum jelly - 15 g, turpentine - 15 g.
Innervation of the pulp -
The common sensory or afferent nerve for the maxillary and mandibular teeth are the II and III branches of the trigeminal nerve (i.e., the maxillary nerve and the mandibular nerve). In turn, nerves depart from them, which form plexuses - the superior dental plexus in the upper jaw and the inferior dental plexus in the lower jaw. In turn, bundles of myelinated nerve fibers branch off from these plexuses, which penetrate into the tooth cavity along with blood vessels - through the apical openings at the apexes of the roots. And, accordingly, forming a neurovascular bundle (tooth pulp) there.
The nerve fibers form a subodontoblastic nerve plexus, which is located under the layer of odontoblasts (also called Rashkov's plexus). Unmyelinated nerve fibers depart from this plexus, which are directed to the peripheral areas of the pulp, where they seem to entwine the odontoblasts, forming the so-called “nadodontoblastic plexus” between the odontoblasts and predentin. Some of the nerve fibers end in this plexus, but the rest of them penetrate into the dentinal tubules.
Arteries, veins and nerves of the upper and lower jaw
This article describes the following anatomical landmarks and their relationship to oral implant surgery: external carotid artery, maxillary artery, pterygopalatine fossa, capitis veins, and trigeminal nerve.
External carotid artery
The arteries supplying the face, upper and lower jaw mainly originate from the external carotid artery. However, branches of the ophthalmic artery (a branch of the internal carotid artery) supply blood to the forehead, scalp, upper eyelid and nose. The external and internal carotid arteries (Figures 1-1 and 1-2) arise from the common carotid artery at the level of the superior border of the thyroid cartilage. The external carotid artery has eight branches:
- Three anterior branches: superior thyroid artery, lingual artery and facial artery.
- Two terminal branches: the maxillary artery and the superficial temporal artery.
- Two posterior branches: the occipital auricular artery and the posterior auricular artery.
- One medial branch: ascending pharyngeal artery.
Figure 1-1 Main branches of the aortic arch
Fig 1-2 Main branches of the external carotid artery
Maxillary artery
The maxillary artery (Figure 1-3) arises from the external carotid artery in the parotid gland as a terminal branch. The branches of the maxillary artery can be divided into three parts:
- Part I or mandibular part (located within the parotid salivary gland and in front of the external auditory meatus): In this part, the maxillary artery gives off branches to the ear, dura mater, temporomandibular joint, mandibular teeth, and mylohyoid muscle.
- Part II or pterygoid part (located in the infratemporal fossa): The branches here mainly go to the muscles involved in the process of mastication, the skin and mucous membrane of the cheek, and also to the buccal muscle through the buccal artery.
- Part III or pterygopalatine part (branches in the pterygopalatine fossa after entering through the pterygomaxillary fissure): the branches here mainly go to the hard and soft palate through the descending palatine artery, to the molars and premolars of the maxilla through the posterior superior alveolar artery, to the upper part of the pharynx and the tympanic cavity through the artery of the pterygoid canal, to the nasopharynx and sphenoid sinus through the pharyngeal artery and to the anterior teeth of the upper jaw through the infraorbital artery.
Figure 1-3 Course of the maxillary artery
The maxillary artery ends with the sphenopalatine artery on the nasal septum after dividing into nasal branches. Figure 1-4 shows in detail the branches of all three parts of the maxillary artery.
Functions of dental pulp –
The functions of the dental pulp stem from its morphology (structure). Below we list its main functions:
- Trophic function - we have already said that the pulp has a well-developed network of blood and lymphatic capillaries.
The main intercellular substance of the pulp serves as an intermediate medium through which metabolism occurs. Thus, oxygen and nutrients from the blood enter the cellular elements of the pulp precisely through the intercellular substance, and metabolic products are excreted through it into the venous or lymphatic systems. But the trophic function of the pulp is not only to nourish its own structures. The dentin and enamel of the crown part of the tooth receive nutrients and calcium salts - almost exclusively from the dental pulp (the processes of odontoblasts play a major role here). But as for the nutrition of the hard tissues of the tooth root, it occurs not only through the pulp, but also due to the process of diffusion of nutrients from the pericementum.
- Plastic function is realized thanks to odontoblasts, which throughout a person’s life participate in the formation of secondary and tertiary dentin. For example, in teeth there is a constant deposition of secondary dentin on the side of the pulp chamber, which leads to a gradual decrease in its volume. The deposition of denser tertiary dentin, as well as the obliteration of dentinal tubules, also occurs due to odontoblasts, and protects the pulp from external irritants and the penetration of bacteria into it.
- The protective function - the function of phagocytosis and disposal of dead cells is provided by neutrophil granulocytes and macrophages. Lymphocytes (plasma cells) - participate in the synthesis of antibodies. Fibroblasts participate in the formation of a fibrous capsule around the inflammatory focus. In addition, the pulp is also a biological barrier that prevents the penetration of pathogenic bacteria from the carious cavity into the periodontium. The protective function also includes the processes of formation of tertiary dentin and obliteration of dentinal tubules that we have voiced.
- Sensory function - carried out due to the presence of a large number of nerve endings.
Age-related changes in the pulp –
Even after the complete formation of a tooth, with age there is a gradual reduction in the size of the pulp chamber. This occurs as a result of continuous deposition of secondary dentin as well as intermittent deposition of tertiary dentin. Consequently, at a more mature age, the pulp will occupy a significantly smaller volume than at a young age. In addition, the shape of the pulp chamber itself changes (as a result, the pulp horns are smoothed out).
All this also has clinical significance, for example, deep preparation of dentin in the area of the pulp horns in old age will be less dangerous. In addition, with age there is a decrease in the number of cellular elements in all layers of the pulp (up to 50% of the initial level), but at the same time the content of collagen fibers increases 3 times. The blood supply to the pulp deteriorates due to the reduction of a large number of capillaries (especially those located in the capillary plexus in the Weil layer). Loss of nerve fibers also occurs, and in particular, this is associated with an age-related decrease in the sensitivity of the pulp to irritants.
With age, the frequency of formation of calcifications in the pulp also increases. Although, if calcification occurs not locally, but diffusely, then this process is called petrification. Petrifications most often form in the root part of the pulp (along the periphery of vessels, nerves, and also inside the vascular wall), sometimes causing disturbances in the blood supply to the pulp and pain. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Periodontology” (Danilevsky N.F.), 5. “Pulpitis of temporary and permanent immature teeth” (Mamedova).