Let's look at one of the most common dental anomalies. Distal dental occlusion is a problem that accounts for approximately 20% of cases of total jaw pathologies in adults and 30% in children. Therefore, you need to understand what this violation is, why it occurs, what threat it poses and, most importantly, how to eliminate it and minimize the consequences.
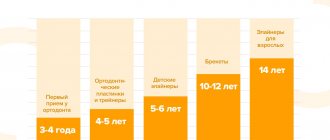
Let us immediately note that characteristic symptoms appear at the age of 4-16 years. If you ignore them and do not take any measures, various complications may begin, including facial asymmetry, difficulties with chewing and swallowing, and inflammatory diseases. It is worth preventing the development of this anomaly, and even better, getting rid of it completely.
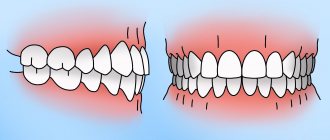
Manifestations of distal bite in the mouth
Closing of lateral teeth during distal occlusion.
Distal occlusion is manifested in the mouth by the closure of the upper and lower teeth according to the “second class” (violation of the relationship between the projections of the antagonist teeth of the upper and lower jaw).
In the frontal segment (at the level of the front teeth) there are two closure options (the so-called first or second subclasses).
In the first case, a “sagittal gap” is observed, which reflects the discrepancy between the dentition in the sagittal plane (anterior-posterior direction). And the upper incisors are in protrusion (inclined forward). In the second option, the upper front teeth are tilted back (into retrusion). With the formation of a deep bite (when the lower teeth are not visible from under the upper ones).
Sagittal chain with distal occlusion. 2 class 1 subclass.
Distal occlusion. 2nd class 2nd subclass.
Symptoms
The orthodontist sees all of the above anomalies during a visual examination of the patient’s oral cavity. The absence of normal closure in the frontal or lateral region is determined; a vertical gap may be observed.
Anatomical features cause various functional abnormalities. Patients with incisal disocclusion experience a number of symptoms:
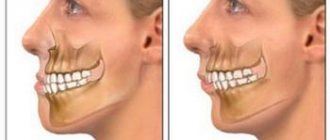
- Violation of the parameters of the lower third of the face. Disproportions can be noticeable both in profile and in frontal view, but in profile they are usually more pronounced. The lower third of the face can be significantly reduced, an effect that makes the supramental fold appear enlarged. The nasolabial folds are smoothed out, and the angle of the lower jaw becomes larger, sometimes approaching 90°.
- Various diction disorders. The most strongly distorted dental consonants are hissing and whistling sounds. If the occlusion is maintained, speech is less affected.
- The process of swallowing saliva and food is disrupted, so overstrain of the muscles involved in lowering and raising the corners of the mouth develops; the orbicularis oris muscle becomes enlarged due to the constantly increasing load.
The stronger the degree of pathology and the larger the size of the vertical gap, the more pronounced all of the listed signs are. Even if they are not developed at the initial stage, over time all symptoms gradually worsen.
Causes of distal bite (distal occlusion)
They are almost always (in the vast majority of cases) skeletal...
- Posterior position of the lower jaw. This is the most common cause of distal occlusion
- Small (short) lower jaw.
Many people write that the cause of a distal bite may be an overdeveloped (excessively large) upper jaw. They say that this is why there is a “gap” between the front upper and lower teeth (sagittal gap)... Many years of observations and our experience have shown that this is not so. With any anomaly of occlusion, there can be no talk of any OVERdevelopment. Everything, on the contrary, is UNDERdeveloped.
The lower jaw ends up in a posterior position (the first reason) only because the lower teeth bump into the upper teeth while the upper jaw is shortened and narrowed (generally underdeveloped). Or, when the upper incisors are “wrapped” back, into retrusion (second subclass). In addition, with distal occlusion, the upper jaw is always narrower than the lower jaw. Which, by the way, is another reason for blocking the lower jaw in the posterior position. And this same “blocking” does not allow the lower jaw, which is caught in the trap, to develop normally. Here is the second reason for distal occlusion - underdevelopment of the lower jaw.
There is also a “dental” reason for distal occlusion. Or more precisely, the dental cause of closure is “second class”. This is when mesial (front) displacement of the upper lateral teeth occurs. And then, even with a normal relationship of the jaws in the sagittal plane, the closure of the lateral teeth (molars) will also be in the second class. True, this is not a true distal occlusion...
A “dental” cause of the second class may complement or may camouflage true distal occlusion. Therefore, it will not be possible to figure out what is the reason for the closure in class 2 visually (by eye). Diagnostics required.
Diagnostics
The main goal of any diagnosis is to identify the cause of the problem. And make a diagnosis. Likewise, the diagnosis of distal occlusion is designed to identify the cause of closure in the second class. In order to separate the flies from the cutlets during treatment, so to speak. That is, dental causes of closure are in the second class from non-dental (maxillary, skeletal).
The main diagnostic methods are:
- Analysis of TRG (teleradiogram) of the skull in a lateral projection. It allows you to clearly determine all the skeletal (jaw) nuances of the problem. Both with the position of the jaws and with their sizes.
- Analysis of plaster models of jaws (for this, casts are taken). It allows you to clarify the “dental” nuances: the size of the teeth, the length and width of the dentition, the features of the relationship (including closure) of the upper and lower teeth
Analysis of TRG (teleradiogram) of the skull in a lateral projection.
Analysis of plaster models of jaws.
It is not recommended to fall below this diagnostic “bar”. Below - just by eye. But this, as we understand, is not the best option.
Diagnostics is the first and key step in the treatment of distal occlusion. Do you want to know why it’s impossible to do without diagnostics?
When will only a surgeon help?
If a person comes to an appointment not only with a greatly enlarged gap, but also with several missing molars or their strong inclination towards the throat, he is referred to a surgeon. In such situations, doctors have to disconnect part of the bone and move it to a physiological position. This is a complex operation that is performed under general anesthesia and recovery from it takes 6-8 months.
We told you what to do with non-physiological interdental distances. The main thing is to contact a competent orthodontist, be patient and set yourself up for a long journey to health. Before installing expensive structures and enrolling in surgical operations with a long rehabilitation period, it is important to undergo a full examination and start with gentle methods.
Errors in the treatment of distal occlusion
The first, main mistake is that many try to treat distal bite with one device. For example, only with braces (this is the most popular option). But braces, although a cool device, are not for skeletal problems. The level of hardware competence of the braces system does not extend further than “to place the teeth on the jaw.” And distal occlusion, as we have already said, is a purely skeletal problem. Jaws and posture are to blame. And braces are not capable of solving problems with posture or jaw problems. After all, braces cannot change the position or size of the jaw. No matter what the would-be doctors promise...
And therefore, such videos are just an advertising gimmick.
Or rather, a convenient “hook” that catches gullible patients. Convenient because it coincides with the desire to do everything quickly and efficiently... But it doesn’t coincide with reality.
And braces cannot be the main device in the treatment of distal occlusion.
Braces are the wrong choice when treating distal malocclusions. In any case, you definitely shouldn’t start with them. Braces, as mentioned and shown above, can be effectively used only at the final stage of treatment of distal occlusion. All major “feats” must be accomplished before working on the teeth. Before using braces. And they are accomplished at the level of the jaws and skeleton (posture). Otherwise, there will simply be nothing to “clog” (close) these teeth (read with braces). See “Fundamentals of the therapeutic concept of “Ortho-Arteli”.
The second common mistake in correcting distal occlusion is treatment with the removal of upper premolars (4 or 5 teeth).
And this mistake is much more serious. Because it can have the most dire consequences. See "Orthodontic treatment with tooth extraction."
After all, as we said above, the main causes of distal occlusion are skeletal. And most often the lower jaw is to blame. And if so, then a reasonable question arises: if the lower jaw is to blame, what does the upper teeth have to do with it (their removal). Where is the logic?
In general, all errors in the treatment of distal occlusion in an adult are usually associated with insufficient diagnosis. Which entails a misunderstanding of the reasons for the occurrence of distal occlusion in each specific case.
For example, the “dental” cause of distal occlusion is very often confused with the “skeletal” (jaw) cause. We remind you that in the first case you need to move the lateral teeth back. And in the second - to push the lower jaw forward and develop the upper one. And if you get confused, if you don’t figure it out... Start distalizing the upper teeth, or worse, remove them when it is necessary to advance the lower jaw... Or vice versa. It is clear that nothing good will come of it.
The third mistake is when, without understanding what’s what, what exactly is the cause of distal occlusion, but realizing, however, that the problem cannot be corrected with braces, they try to solve the problem surgically. Using orthognathic surgery. Through osteotomy of the lower and upper jaws.
This is where I would like to dwell in more detail. And explain something. Why do orthodontists send to a surgeon to “treat” a distal bite? They have already said: they understand that braces will not cope. But they don’t understand how to treat it without braces. They don’t understand because in dentistry in general, and orthodontics in particular, there are a lot of prejudices regarding the possibilities of moving the lower jaw forward and developing the upper jaw. And these, as we saw above, are the main (“key”) points in the treatment of distal occlusion.
Most orthodontists simply do not believe in this (that it is possible in principle). Because someone (even a “great one”) said two hundred years ago that this cannot be done. Time has passed. Everyone has already forgotten why it is “impossible”. But no one even bothered to check why, in fact, it was impossible...
And therefore, those doctors who blindly believe in these moss-covered “dogmas” simply do not see an alternative. And for them there are only two extreme poles in the treatment of distal occlusion: braces and surgery. That's all.
During a direct examination by a specialist, you will be able to find out your exact diagnosis, as well as receive a referral for diagnosis or a treatment plan.
And in our clinic we treat distal occlusion between these two poles. Using methods of maxillofacial orthopedics and craniodontics. Here are the ones: changing the position of the lower jaw and changing the size of the upper. And we get good results, without regard to the fact that someone once said something... We must always double-check what was said. We checked. And everything turned out to be somewhat different. Or rather, not at all the way they “frightened” us. You can also push it out. It can be developed. You just need to know how, because there are some “secrets” here. And we, at the Orto-Artel clinic, knowing these “secrets”, take advantage of these opportunities, successfully eliminating distal occlusion of any complexity.
By the way, if we are talking about surgical treatment of distal occlusion, then we need to determine when and in what cases surgery is generally appropriate. But the indication is basically the same - a small lower jaw, the so-called lower micrognathia, and the micrognathia is very pronounced.
We indicated this reason above as one of the skeletal reasons. I will add: the lower jaw should be VERY short. Literally ugly. Only then can this be resolved surgically. In all other cases, you can do without surgery. Proven and tested many times.
By the way... In our clinic, a good half of the patients have formal indications for surgical treatment of distal occlusion. But only a few got to the surgeon. Because formalities are formalities, but compromise solutions were found that satisfied everyone: both the patients and us. This is because we approach treatment not formally, but in essence. And we are guided by logic and common sense.
Well, as a special case of a short lower jaw, which cannot be corrected except by surgery, this is a small chin. If it is small and spoils the face, then even by pushing the lower jaw forward we will not get the aesthetics we want. Simply because orthodontists do not have the means and instruments (devices) to selectively influence the chin. It is impossible to stimulate the chin to grow. Only surgery.
Inferior micrognathia.
This is where the indications (and there is essentially one) for surgical intervention for distal occlusion end.
Going with a knife into the upper jaw - God forbid! Even if the upper jaw is indirectly to blame for the distal occlusion. More precisely, the upper jaw also, as a rule, suffers (dimensionally) with distal occlusion. The upper jaw is directly connected to the base of the skull. And such interventions can then backfire. Literally. And the most important thing is that there is no need to go there surgically. The upper jaw can be developed!!!