From this article you will learn:
- what is curettage of gums and teeth (video),
- methods of its implementation, reviews,
- What is flap surgery for periodontitis?
The article was written by a practicing periodontist surgeon.
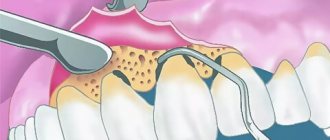
Curettage is a surgical technique for the treatment of chronic periodontitis, which involves scraping out the contents of periodontal pockets. Its goal is to remove granulations, subgingival dental deposits, the epithelial lining of the pockets, as well as a layer of necrotic “cement” on the surface of the tooth root from the pockets. This is a fairly complex intervention that requires surgical skills and should ideally be performed only by a periodontal surgeon (oral surgeon).
There are 2 methods of this operation in dentistry. Closed curettage is a technique that is preferred for shallow periodontal pockets up to 4.0 mm (which corresponds to mild periodontitis). Open curettage is a more complex surgical technique, which is indicated in the presence of periodontal pockets with a depth of more than 4.0 mm, i.e. carried out for moderate to severe periodontitis. The open technique requires good surgical skills, because... During the operation, the gums will peel away from the bone tissue around the teeth.
Closed curettage technique –
There is also an even more radical option for open curettage, which is called the term “flap operation” (we will also talk about this in more detail below). The following is a very important point. If the closed curettage technique has the right to be performed by ordinary dental therapists with advanced training in periodontics, then open curettage and flap operations can only be performed by dental surgeons or maxillofacial surgeons.
When to do gum curettage?
Indications for curettage of periodontal pockets are: 1) the presence of chronic generalized periodontitis, 2) local form of periodontitis. In both cases, periodontal pockets will appear along the surface of the tooth roots, the formation of which is associated with the resulting destruction of the dentogingival attachment (i.e., the attachment of the marginal gum to the neck of the tooth).
Destruction of the periodontal attachment in chronic generalized periodontitis occurs against the background of irregular oral hygiene, which contributes to the deposition around the necks of teeth - soft microbial plaque and hard tartar. Microorganisms in the composition of dental plaque trigger an inflammation process in the gums, which at the first stage is manifested by swelling and redness of the gums, bleeding when brushing teeth. Already during this period, gradual destruction of the periodontal attachment begins (with the formation of periodontal pockets).
Chronic generalized periodontitis –
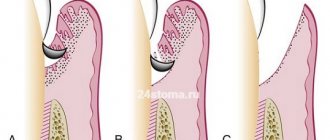
1) Formation of periodontal pockets –
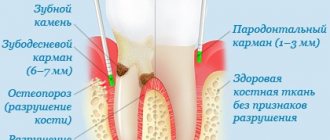
As soon as the periodontal attachment is destroyed, so-called “periodontal pockets” are formed between the gum and tooth. At first they are relatively small. Shallow periodontal pockets up to 4.0 mm deep correspond to mild periodontitis, and closed curettage may be indicated for precisely such patients (to prevent the progression of periodontitis).
Periodontal pockets are localized between the gum and the root of the tooth (Fig. 2). One wall of the pocket is the surface of the tooth root, on the surface of which microbial plaque and subgingival tartar are attached. The other wall is the inner surface of the unattached gum, which is covered with pathological epipelium and granulations. Thus, the typical contents of a periodontal pocket are dental deposits, granulations, and pathological epithelium.
Scheme of the structure of the periodontal pocket -
As we said above, in the absence of treatment, the depth of the pockets gradually increases. This occurs due to the destruction of the bone plate around the tooth, as well as periodontal fibers, due to which the tooth root is firmly attached to the bone. This gradual process inevitably leads to the appearance of tooth mobility, the increase in the degree of which in the future will be directly related, among other things, to the continuing increase in the depth of periodontal pockets.
2) Destruction of bone tissue around the tooth –
As was seen above in Fig. 2, the periodontal pocket “grows” deeper due to the destruction of periodontal fibers between the root surface and the bone plate, which also leads to the destruction of the bone graft itself (alveoli). Moreover, it should be noted that bone tissue does not simply disappear without a trace, but is replaced by the so-called inflammatory granulation tissue, which contains a large number of microbial cells, osteoclasts, etc. On an x-ray, the absence of bone around the teeth looks like this (Fig. 3b).
Clinical situation No. 1 –
Next, in Figures 4-6, you can see exactly what a deep periodontal pocket looks like under the gum in the interdental space between the canine and premolar in the lower jaw. As we can see from the outside, the gums look quite healthy, and only on an x-ray (Fig. 5) can we see a slight darkening between the roots of the teeth, indicating the presence of destruction of bone tissue. But we have a completely different look after the gums are detached and granulations are cleaned out of the pocket between the teeth (Fig. 6).
In Fig. 6 we see a deep bone defect of a large volume, as well as subgingival calculus on the surface of the tooth root (indicated by an arrow). Such deep periodontal pockets can no longer be sanitized using the closed curettage technique, which is carried out without gum detachment and therefore does not imply visual inspection of bone defects in the depths of the periodontal pocket (i.e., the doctor will simply blindly try to clean out what to clean out from under the gums).
Therefore, for pockets larger than 4.0 mm, only open curettage or flap surgery should be used. For medium and deep periodontal pockets, only these methods allow you to remove all granulations and dental deposits from under the gums, carefully scrape out the pathological epithelium from the inner surface of the gums, and also replant synthetic bone tissue in the area of deep bone defects (with the hope of partially restoring bone levels ).
Why is it impossible to do without curettage when treating periodontitis (in principle) -
With shallow periodontal pockets up to 4.0 mm, provided that you have good equipment (a good scaler, a Vector device) and the painstaking work of a periodontist, it is still possible to stop the progression of chronic periodontitis. The biggest challenge will be removing subgingival deposits from periodontal pockets, which is difficult to do even in shallow pockets, given that the work is carried out almost blindly.
When deep periodontal pockets have formed (more than 4 mm deep) and granulation tissue has formed at their depth, the process essentially becomes irreversible, despite any conservative local and general anti-inflammatory therapy. You can drink antibiotics, rinse your mouth with antiseptics, smear your gums with anti-inflammatory gels, irradiate your gums with a laser, but all this will be ineffective. Why?
- Firstly , it is impossible in principle to completely remove dental plaque from deep periodontal pockets. The fact is that the doctor inserts the ultrasonic attachment under the gum “blindly”, i.e. he makes movements without seeing what exactly is happening in the periodontal pockets. Therefore, some dental plaque necessarily remains in the pockets.
- Secondly , if deep periodontal pockets have formed, then in them, even after removal of dental plaque and anti-inflammatory therapy, conditions are created for the development of infection and further progression of periodontitis. The fact is that the pockets are filled with granulations, without surgical removal of which it is impossible to stop further destruction of the bone tissue around the tooth.
It turns out that you can still try to remove subgingival dental deposits and granulations in shallow pockets using ultrasonic cleaning and closed curettage techniques. It will be possible to do the same thing efficiently in deep pockets only by performing open curettage or patch surgery.
Symptoms
Symptoms appear over time and develop progressively. The following signs may indicate the disease:
- severe pain that occurs in the place where the tooth erupts. It can radiate to the temple or ear;
- difficult to chew and swallow food. If the disease concerns the lower third molar, then it will be difficult for the person to even open his mouth;
- The gum tissues swelled and hyperemia occurred. This happens in the place where the tooth erupts;
- the tooth next door hurts and is destroyed (if the wisdom tooth that is erupting is incorrectly positioned);
- regional lymph nodes on the side where the tooth is cut have enlarged;
- pus is released and bad breath appears.
How is closed curettage performed?
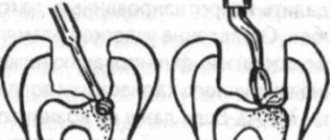
The purpose of the operation is to remove granulations from periodontal pockets, as well as those subgingival dental deposits that could not be removed using an ultrasonic scaler.
Disadvantages of the technique: curettage is carried out blindly, there is no visual overview of the surface of the roots, periodontal pockets - because of which granulations and dental deposits partially remain in their places. Scheme of closed curettage –
Closed curettage of periodontal pockets is performed under local anesthesia. Curettage of the gums with sharp curettes is accompanied by bleeding, which further complicates visual control. At the end of the operation, the wound surface is treated with antiseptics, and a protective gum bandage is applied for several days. In Fig. 7 you can see the instruments used to perform closed curettage. Laser surgery is also an option (see video below).
Closed curettage can be more or less effective only with shallow periodontal pockets (no more than 3-4 mm), i.e. with the mildest degree of periodontitis. For moderate and severe periodontitis, closed curettage (by reducing the volume of granulations) can only temporarily improve the condition of the gums, but this improvement will only be short-term, and periodontitis will definitely progress further. In some cases, closed curettage is performed as a preparatory step before open curettage or flap surgery.
The closed curettage technique is popular in dental clinics that do not have an experienced periodontist surgeon, and therefore the operation is performed by an ordinary general dentist (periodontist). These specialists have neither the skills nor experience in performing complex surgical interventions in the oral cavity, which include open curettage and flap operations. Therefore, the worst thing that can happen to you in this situation is that you will undergo a closed curettage (although with your pocket depth, more radical techniques have long been indicated for you).
In this case, the following consequences are possible - 1) you will get a short-term, but still improvement, 2) you will not get any results from the treatment in principle, 3) closed curettage can provoke an exacerbation of periodontitis, in which case you will get suppuration from the periodontal pockets and acceleration of inflammatory bone resorption.
Closed curettage using curettes and laser –
Video 1 shows scraping of granulations from a periodontal pocket in the area of only one tooth. As you can see, this use of curettes is quite traumatic and is accompanied by bleeding. In video 2, periodontal pockets are treated using a laser. In most cases, this will also be accompanied by slight bleeding (especially if the gums are loose and inflamed).
Treatment methods
When selecting therapy, an integrated approach is used. The source of infection is initially eliminated. The types and number of procedures are selected depending on the severity of the disease. In addition to treatment in the dental office, procedures are performed at home. Additionally, the doctor advises getting rid of bad habits (drinking alcohol, smoking) and treating systemic diseases.
Open curettage of periodontal pockets –
The purpose of this operation is to remove all subgingival dental deposits, remove inflammatory granulation tissue from under the gums, eliminate periodontal pockets, and also stimulate the restoration of bone tissue (by means of “replanting” materials based on synthetic bone into bone defects).
Before the operation begins, careful preparation must be carried out - dental plaque must be removed, anti-inflammatory therapy must be carried out, and if there are indications, splinting of mobile teeth is carried out. The latter is very important, because Carrying out curettage without splinting mobile groups of teeth will lead to an even greater increase in their mobility, and will also increase the resorption of bone tissue around them.
Scheme of open curettage –
Description of the main stages of open curettage -
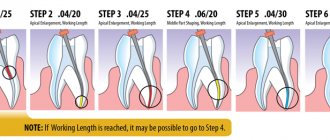
The operation is performed against the background of antibiotic therapy, under local infiltration and conduction anesthesia. During one operation, usually only one segment of 7-8 teeth is removed (usually this volume of intervention requires at least 2.5 hours of time). Next, we will focus on the main points of the operation.
1) Incision and detachment of flaps - open curettage means that after the onset of anesthesia, we make an incision in the gums around the necks of the teeth and peel off the mucoperiosteal flaps (on both sides of the dentition). Detachment of flaps from the necks of teeth and bone will allow us to expose the surface of the roots and bone tissue defects. Thus, we will obtain visual control over periodontal pockets and subgingival dental plaque (Fig. 9).
Clinical case No. 2 (Fig. 8-12) –
2) Removal of granulations and bone grafting – removal of granulation tissue is carried out using sharp curettes (in combination with an ultrasonic scaler or laser). The scaler softens granulations well and makes it easy to scrape them out of all the gaps and lacunae of bone tissue, as well as polish the root surface, removing a layer of necrotic cement from it. Next, antiseptic treatment of the wound is carried out. Next, chemical modification of the root surface is carried out, for example, with a suspension of tetracycline.
Next, the bone defects are filled with bone material, and ideally covered with special membranes. Bone grafting is effective precisely in the presence of deep periodontal pockets (when there is vertical resorption of bone tissue). If inflammatory bone resorption against the background of periodontitis occurs evenly and horizontally, bone grafting will not allow for an increase in bone volume. As a continuation of clinical case No. 2, you can see in this patient a partial restoration of bone volume in the interdental space (Fig. 11).
3) Suturing – sutures are placed in the area of the interdental papillae. At the end of the operation, a protective gum bandage is also applied, which will protect the operation area and promote speedy healing. Sutures are removed 10 days after surgery.
Open curettage: video
Medicines
Professional teeth cleaning removes plaque and stones. But this does not mean that the infectious process is over. To eliminate it, you need to use medications:
- Mouth rinses. Antiseptics are used to destroy pathogenic microflora. For example, Chlorhexidine or Miramistin. They are used for no more than 7-10 days, so as not to cause resistance of microorganisms.
- Gels, ointments with antimicrobial action. They eliminate the infectious process and suppress inflammation. It is recommended to use 2 times a day for 7 days.
- Anti-inflammatory drugs. They are used topically in the form of an ointment or systemically in the form of tablets. They suppress swelling, pain, redness.
- Regeneration products. Use oils and ointments based on vitamins. In addition to herbal products, ointments are used that stimulate cell regeneration.
- Antibiotics. Systemic drugs are prescribed only for severe infections that affect the body systemically. They are used in the form of tablets, suspensions, injections. They are prohibited from being used together with alcohol.
Medicines are designed to complement the main treatment. They accelerate the destruction of infection and suppress the inflammatory process. With their help, the effect of professional cleaning is enhanced.
Flap surgery on the gums for periodontitis –
Flap surgery on the gums allows not only to remove all subgingival dental plaque, but also to remove inflammatory granulation tissue from under the gums. It allows, in principle, to eliminate periodontal pockets, and also, in some cases, to stimulate partial restoration of bone volume (in vertical bone defects). The difference between flap surgery and open curettage is that the incision during flap surgery is made 1-1.5 mm from the edge of the gum (24stoma.ru).
Then this 1.5 mm strip of gum, which wraps around the necks of the teeth, is simply removed. Firstly, this allows us to reduce the size of the flaps (gum size), because with severe bone resorption and after removing a large number of granulations, excess gum will be observed. We will not have enough underlying tissue volume to stretch the gum back to the necks of the teeth. That is, as a result, we will receive partial exposure of the roots of the teeth, but at the same time, periodontal pockets between the gums and the roots of the teeth will be completely absent. And this is the most important thing if we want to stop the progression of periodontitis.
The decrease in gum level after surgery can be somewhat reduced if synthetic bone tissue preparations are used for grafting into bone defects. The effect will be even better if special bioresorbable membranes are also used. At one time, the operation is performed on a segment of no more than 6-8 teeth, and takes at least 2.5 hours. This is a complex procedure that requires good surgical skills.
Carrying out flap surgery (animation and video) –
What is pericoronitis
Pericoronitis is a process during which the gum tissue becomes inflamed. A similar complication occurs when the tooth is difficult to cut and takes a long time. Pericoronitis is usually noted in relation to the wisdom teeth, which are located below. And here it is important to start treating the disease in time to avoid the acute stage.
Because there is no room for such teeth, they erupt incorrectly. When the gums are injured over a long period, inflammation begins. There are cases when the tooth has not fully erupted and is almost invisible. Pericoronitis can also develop here.
Flap surgery and curettage: price 2021
So how much does curettage of periodontal pockets cost in mid-price clinics in Moscow? For closed curettage, the price will start at an average of 700 rubles per tooth. Carrying out closed curettage with a laser will be slightly cheaper and will cost from 500 rubles per tooth.
The cost of open curettage for a segment of 6-7 teeth will be about 14,000 rubles (including the cost of economy-class bone material). The cost for each tooth starts from 1,500 rubles, but this price does not include the use of bone material. As for flap surgery, a segment of 6-7 teeth will cost you about 18,000 - 20,000 rubles, taking into account the cost of economy-class bone material.
Diagnostics
When a patient comes to the clinic, the dentist conducts the following examination:
- survey of patients, complaints;
- examination of the oral cavity using instruments;
- inspection of the quality of dental care;
- test for gingivitis;
- X-ray of the jaw;
- prescribing MRI or other hardware diagnostics;
- rheography.
The diagnosis is established when the following pathologies are identified:
- detection of symptomatic gingivitis;
- pronounced periodontal pockets;
- violation of the integrity of the cortical plate of the bone;
- osteoporosis - loss of bone tissue.
Gingivitis is characterized by redness of the gum tissue, sometimes it takes on a bluish tint. Periodontal pockets are checked for each tooth using a special probe. The degree of density/rarefaction of bone tissue makes it possible to distinguish periodontitis from periodontal disease. Periodontitis is characterized by a thinning of bone tissue density, while periodontal disease is characterized by compaction.
Reasons for the formation of pathology
Changes in the structure of periodontal tissues can be caused by various factors:
- inflammatory diseases of the gums and periodontium, which form as a result of poor hygiene: swollen and loose gums lose their elasticity, are easily injured, which further complicates hygiene and leads to increased inflammation, the formation of subgingival stones,
- hard deposits: dense deposits that appear above the edge of the gums, which were not removed in a timely manner, become favorable soil for the development of microorganisms. Colonies of bacteria are formed, which are subsequently calcified under the influence of saliva components. The sharp edges of the stones damage the mucous membrane, causing inflammatory reactions and changes in the structure of periodontal tissues,
- Bite defects: such features lead to the appearance of retention points - areas that are very difficult to clean from plaque residues and food particles. This leads to the formation of bacterial plaques and stones. Also, incorrectly positioned teeth can easily rub and injure the mucous membrane, contributing to the formation of an inflammatory process on it,
- systemic diseases: inflammation of periodontal tissues, disruption of their blood supply and the formation of hard deposits are symptoms of underlying diseases. For example, metabolic disorders, diabetes mellitus, endocrine pathologies, bone disease (histiocytosis), leukemia.
Important! In addition to the main reasons that lead to inflammation of periodontal tissues, there are also factors that aggravate the disease or contribute to its formation: smoking, eating preferably soft foods, violation of the technology for installing structures and dentures or their inappropriate sizes, natural hormonal changes (pregnancy, adolescence, menopause).
Can complications occur?
Open intervention can provoke:
- swelling and local soreness;
- inflammatory changes;
- increased sensitivity.
It is better to use closed curettage only at the very initial stages (not complicated by serious pathology). If the process has already gone deep enough, then the only way out is to resort to open surgery. This method allows you to perform sanitation quickly, effectively and radically.
But the ideal option to remove pockets is to use modern options - vacuum, laser. These treatment methods are less traumatic and reduce the number of complications.
Prevention methods
It is not difficult to avoid problems associated with gum disease. The basic rule is to brush your teeth daily (at least morning and evening). Particular attention should be paid to the interdental spaces, where food debris often remains. In the future, they become a suitable environment for the appearance of bacteria. Acid produced by pathogenic organisms is the root cause of gingivitis.
Another useful rule is to rinse your mouth after every meal. In addition, it would be useful to regularly treat the oral cavity with ultrasound.
Who's at risk
Experts in the field of periodontology identify specific factors that largely contribute to the development of inflammatory and dystrophic processes in the gums and periodontal tissues, as well as to their gradual destruction. Those at increased risk are primarily men aged 30-40 years, smokers and those who abuse alcoholic beverages1.
However, it must be recognized that today no one is immune from the appearance of periodontal pockets. Such pathological phenomena are also often diagnosed in patients during adolescence, and here the most common causes are hormonal imbalances or poor oral hygiene.
Smokers are more susceptible to the problem
Dental care for gum pockets
If a patient has gum pockets, in addition to therapy in the dental office, treatment is carried out at home. All doctor’s recommendations must be strictly followed:
- daily brushing of teeth at least 2 times a day;
- periodic use of mouth rinse to provide antiseptic treatment;
- the use of preparations for cleaning teeth to eliminate inflammation and periodontitis;
- using an irrigator to clean the interdental spaces using a jet of water with strong pressure (they additionally massage the gums, increasing blood flow, activating metabolism and regenerative processes).
Periodically rinse your mouth with herbal decoctions. For example, chamomile and calendula. They simultaneously eliminate infection and suppress inflammation.