Sore throats or tonsillitis include infectious diseases characterized by inflammatory processes in the palatine tonsils. There are many such pathologies. They are usually classified according to the type of pathogen and clinical course. The most dangerous types of tonsillitis include necrotizing tonsillitis of Simanovsky-Vincent.
Nowadays it can rarely be found in patients. The main difference between ulcerative membranous tonsillitis and other forms of tonsillitis is necrosis of the tonsils and surrounding tissues. The process develops rapidly, so complications are frequent.
What is ulcerative glossitis
Glossitis, as a rule, becomes a consequence of injury to the mucous membrane of the organ, as a result of which an open wound appears on its surface - a direct path for the penetration of bacteria and infections. This injury can be caused by accidental biting, trauma such as fish bones, exposure to overly spicy or acidic foods, or burns from eating excessively hot foods.
The photo shows ulcerative glossitis
The pathology itself is inflammatory in nature - painful ulcers appear on the surface of the tongue, the tissues of the organ swell, turn red, painful sensations and burning occur, and in the case of the ulcerative form, a dense coating of a grayish tint also forms. The result is unpleasant odor from the mouth, difficulties with eating and speaking.
Complications and consequences
The advanced form of the disease leads to inflammatory damage to other organs, including the heart, kidneys, and joints. The most dangerous complications include:
- mediastinitis
– inflammation of the mediastinal tissue; - chronic bronchitis
- inflammatory damage to the bronchi; - sepsis –
spread of infection through the bloodstream; - arthritis -
inflammation of the joints; - glomerulonephritis is
a dangerous kidney disease; - purulent meningitis -
damage to the meninges; - peripharyngeal abscesses
- suppuration of the lymph nodes and tissue of the peripharyngeal space.
Timely access to a medical facility allows you to avoid negative health consequences.
Is the disease contagious?
Regarding the contagiousness of glossitis, it is quite difficult to give a definite answer, since the disease has many different forms, which mainly depend on the root cause of the problem.
“You say that the disease is rarely transmitted, but my son brought this infection from kindergarten! The diagnosis is herpetic glossitis. The tongue was swollen, covered with tiny sores, the child cried in pain. After the examination, the therapist prescribed us tablets and rinses and advised us to buy pharmaceutical chamomile. In principle, I won’t say that the treatment took a very long time, maybe a couple of weeks, but the unpleasant impressions remained. In my family, neither I nor my sisters had this, so I was generally in a panic...”
Lydia D., Nizhny Novgorod, from correspondence on the woman.ru forum
Some forms of the disease can be transmitted by contact
. If the provoking factor is not an infection, then there will be no risk of transmission from the carrier to a healthy person. If the whole point is infection and spread of the fungus, then the disease can be transmitted, but not by airborne droplets, but as a result of direct contact of another person with the affected organ.
Causes
Inflammation of the palatine tonsils is provoked by infections transmitted by airborne droplets. Less commonly, infection occurs through contact and household contact (through shared dishes, towels, bed linen). The most common causative agent of purulent sore throat is hemolytic streptococcus. However, if a person’s immune system works normally, bacteria of this group die immediately after entering the body. The development of pathology is facilitated by weakened immunity and provoking factors.
Indirect causes of purulent sore throat include:
- severe hypothermia;
- chronic diseases of the upper respiratory tract;
- oral infections;
- alcoholism and smoking history;
- stress, overwork, strong emotional tension;
- living in areas with difficult environmental conditions;
- deficiency of vitamins and nutrients;
- mechanical damage to the tonsils (trauma, surgery).
The disease is diagnosed with equal frequency in adults and children.
Types of ulcers and their clinical manifestations
The appearance of suspicious neoplasms on the surface of an organ is always an alarm bell that cannot be ignored. In this case, the rashes may differ from each other, depending on the disease and the cause of its appearance. Let's consider various clinical manifestations of pathologies of the oral mucosa and find out what they may indicate.
White sores on the surface
If white or yellow ulcers appear on the back of the tongue, gums and inner surface of the cheeks, first of all you need to find out why they appeared. Most often, such a symptom indicates candidiasis (thrush) - it develops as a result of too intense proliferation of yeast fungi in the body.
The problem can be triggered by a sharp decline in immune defense or, for example, taking powerful medications, including antibiotics. With yeast glossitis, rather deep grooves form on the tongue, in which an abundant dense coating begins to accumulate. These symptoms are accompanied by itching and an unpleasant odor. The problem does not pose a serious threat if treatment with antifungal agents is started in time.
This is what leukoplakia of the tongue looks like
Another possible cause of white rashes is leukoplakia. The pathological process is accompanied by excessive growth of soft tissue cells and the appearance of whitish thickenings on the surface of the organ. This diagnosis is often made to heavy smokers, as well as to patients who experience constant trauma to the mucous membrane due to an incorrectly installed filling/crown or due to the crooked position of some teeth.
Reddish translucent bubbles
Almost colorless growths, often filled with blood, usually indicate problems in the digestive system or endocrine glands. Reddish blisters appear on the tip and root area of the tongue, as well as on the inner surface of the cheeks, including with atopic dermatitis.
It could also be due to infection or damage to the mucous membrane. So, for example, a single transparent blister may be the body’s reaction to a thermal burn. Bloody hematomas indicate sudden changes in blood pressure or vascular damage.
The photo shows a blister filled with blood.
Discolored blisters
As mentioned above, colorless neoplasms in the form of blisters most often appear after a burn to the mucous membrane. If small bubbles filled with serous fluid appear on the tongue or other part of the oral mucosa, this may indicate activation of the herpes virus in the body. Sometimes with scarlet fever, light gray rashes appear in the mouth, which gradually become brighter and spread to the throat.
This is what herpes looks like on the tongue
Ulcers on the lateral surfaces
The formation of ulcers is most often a consequence of organ injury. The wound becomes a favorable environment for the proliferation of bacteria, which often leads to the formation of a purulent boil. Sometimes a dark rash appears on the side surfaces, resembling a hematoma in its shape and appearance. This symptom indicates damage to the deeper layers of the epithelium and taste buds.
Ulcerative rashes due to stomatitis
In the first stages of the development of the disease, small rashes appear on the oral mucosa, more like a slight swelling. Gradually more pronounced aphthae appear, when damaged, a white or yellowish membrane with a red rim forms in their place. Such ulcers heal in just a couple of weeks and do not leave scars. Aphthous stomatitis can become chronic. In this case, periods of exacerbation usually bother the patient 1-2 times a year.
The photo shows stomatitis on the tongue
Afty Bednar
Erosive areas appear on the surface of the organ - a similar phenomenon is usually diagnosed in newborns and young children. The cause of canker sores is most often caused by minor injuries received during feeding, due to the habit of sucking the thumb while sleeping or putting foreign objects into the mouth. However, neoplasms, as a rule, are localized on the surface of the hard palate - erosion most often takes on an oval shape. The treatment prognosis is favorable if the problem is recognized in time, the traumatic factor is eliminated and antibacterial therapy is started.
Injuries and mechanical damage
Ulcers and erosions occur as a result of accidental biting, blow, bruise or permanent injury from an incorrectly installed filling or crown, or sharp elements of the braces system. If the integrity of the epithelium is not broken, a dark hematoma will appear on the surface of the mucosa - the result of interstitial hemorrhage. If the mucous membrane is damaged, a painful ulcer will appear at the causative site. The injury usually heals quickly on its own. If the scratch does not go away for a long time, it is better to consult a dentist, since there is a risk of infection of the wound and the development of complications.
Ulcers and erosions can occur as a result of accidental injury
Ulcerative-necrotizing gingivostomatitis
The causative agent of infection is anaerobic microflora, which forms on the palatine tonsils, in carious lesions and periodontal pockets. Therefore, this diagnosis often becomes a complication of sore throat, diseases of the upper respiratory tract, and pathologies of the hematopoietic organs. Ulcerative-necrotizing gingivostomatitis also develops against the background of heavy metal poisoning, infection with Koch's bacillus, the development of syphilis, AIDS and cancer.
The photo shows ulcerative necrotizing gingivostomatitis
After the incubation period, the patient is overcome by weakness, his temperature rises, his gums become covered with ulcers, and the mucosal tissues lose their elasticity and become loose. Often with this form of the disease, the lymph nodes become enlarged and painful.
Symptoms of purulent sore throat
In most patients, the first signs of purulent tonsillitis appear 2-3 days after the pathogen enters the body. When the patient's immunity is weakened, the clinical picture is most pronounced. In adult patients, the following symptoms are observed:
- the appearance of noticeable white or yellowish spots of pus on the tonsils;
- high body temperature (in the range of 39-40 ° C);
- intense pain in the throat that increases during swallowing;
- significant enlargement of the lymph nodes located under the lower jaw;
- easily removable whitish coating on the tongue;
- severe headaches;
- feeling weak and overwhelmed;
- loss of appetite;
- aching joints.
In adults, with timely treatment, the acute stage of the disease rarely lasts longer than a week. If the patient does not seek help from specialists, there is a risk of complications.
Causes and symptoms of pathology
It was already mentioned above that the disease most often develops against the background of damage to the tongue and penetration of infection into the wound. This leads to the appearance of very unpleasant symptoms that prevent a person from living a full life, eating normally and communicating with people. Thus, experts identify several key reasons that can cause the development of ulcerative glossitis:
- organ damage
- thermal injury,
- candidiasis of oral tissues,
- the presence of infectious diseases,
- anemia.
A common cause of pathology is damage to the tongue.
A distinctive feature of this form of pathology is the appearance of numerous painful red ulcers that can appear at the root, side or tip of the tongue, begin to bleed and cause serious discomfort.
On a note! The appearance of white ulcers in the mouth, concentrated mainly under the tongue, usually indicates the development of aphthous stomatitis. Taking into account the color and location of the rashes, a specialist can make a preliminary diagnosis, but to accurately determine the problem, you will most likely need to undergo additional examinations and tests. It is quite difficult to independently diagnose the disease, since many organ pathologies have similar symptoms.
With the ulcerative form of glossitis, a dark gray plaque also appears, and the mouth begins to smell unpleasant. The patient notes a general deterioration in his condition. If these symptoms appear, you should seek medical help as soon as possible, because prolonged ignoring of the signs of the disease can lead to dangerous complications.
Forms of the disease
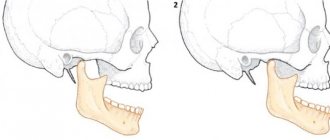
The form of purulent tonsillitis depends on many associated factors and conditions. The most common three forms of development are follicular, lacunar and ulcerative-membranous (necrotic). Each type is characterized by characteristics of the course, specific lesions of the tonsil tissue and varying duration.
Follicular
Follicular tonsillitis is manifested by pinpoint purulent lesions of the parenchyma of lymphoid tissue and follicles of the tonsils. The disease in 85% of cases is caused by group A streptococci. The remaining cases of infection are associated with staphylococcal infection, Haemophilus influenzae, pneumococcus, and adenovirus. This form of pathology is accompanied by a rapid increase in the symptom complex, severe hyperthermia, sweating, loss of sleep and appetite. Intense pain in the throat can radiate to the ear.
Lacunarnaya
This type of disease causes severe inflammatory damage to the tissues of the peripharyngeal ring. The opening of abscesses is accompanied by the formation of specific perforations on the surface of the tonsils - lacunae. The acute phase of the disease is manifested by an increase in the size of the tonsils, up to difficulty breathing. Along with other symptoms, a characteristic sign of the lacunar type of pathology is bad breath. Sometimes doctors note a noticeable change in voice and diction problems. Inadequate therapy can lead to the development of a paratonsillar or retropharyngeal abscess.
Necrotic
Necrotizing ulcerative tonsillitis is rare (about 5-6% of cases). The main cause of the development of this type of disease is fusospirochetous infection. The rapid development of the infectious-inflammatory process causes the formation of histological changes in the tissues of the palatine tonsils. Violations of vascular permeability, associated with the active production of histamine and cytokines, lead to hypertrophy and sometimes tissue necrosis. The first sign of the disease is the feeling of a “lump in the throat.” Later, a sharp, unpleasant putrid odor appears from the mouth and salivation increases.
Glossitis in children
The most common form of pathology among children is catarrhal disease, which usually occurs due to biting, injury from a brace system or sharp edges of a filling, or eating hot food. The result is obvious inflammation and severe pain.
The photo shows the desquamative form of glossitis in a child
But children with worms often encounter a desquamative form of the pathology1. At the same time, the child may not have any pain at all, and concerned mothers recognize the disease itself only by suspicious spots that appear on the body of the organ. Among other possible causes of the problem, experts identify pathologies of the endocrine system, atopic dermatitis, infectious diseases, pathologies of the blood and gastrointestinal tract. But candidal glossitis often becomes a consequence of childhood diabetes mellitus, a decrease in the body’s defenses and the use of potent medications, including antibiotics.
Diagnostic features
To determine the form of the pathology and the cause of its development, it is necessary to conduct a differential diagnosis. The specialist must conduct a visual examination of the surface of the tongue, teeth and gums, talk with the patient about recent diseases, injuries and mechanical damage, and allergies. In more severe cases, blood tests may be required - general, cytological, histological or bacteriological. Sometimes microscopy of scrapings and PCR diagnostics are required to identify pathogens.
Tests are required for diagnosis
Diagnostics
Since there are so many tonsillitis, doctors need to learn to distinguish between them:
- with ordinary sore throat, the sore throat is severe, with general weakness and fever. Both tonsils are affected, they are hyperemic, enlarged, there is plaque, but it is lighter;
- with diphtheria, the symptoms resemble ordinary tonsillitis with bilateral damage to the tonsils, but the diphtheria film on them cannot be confused with anything. It is tightly attached to the surrounding tissues, gray in color and almost impossible to remove. The decisive moment of diagnosis is taking a swab from the throat;
- tonsillitis during leukemia. Pain and intoxication, tonsils can be necrotic, as with Simanovsky-Vincent angina. A general blood test showing exclusively leukotic manifestations is of decisive importance. This is a high concentration of leukocytes (several tens of times higher than in a normal inflammatory process) with blast forms of immature cells.
It is clear that laboratory tests help in making an accurate diagnosis, since based on external symptoms it is not always possible to completely verify the clinical picture of the disease. It is possible to finally give the patient the correct diagnosis with the help of:
- clinical blood test. Leukocyte background and formulas, erythrocyte sedimentation rate are assessed;
- general urine analysis. Determine whether the kidneys are affected, whether there is protein and red blood cells in the urine;
- blood biochemistry with determination of total and C-reactive protein, creatinine, bilirubin, urea, etc.;
- a swab taken from the throat. We are talking about both the detection of a specific pathogen and the determination of the sensitivity of pathogenic flora to antibacterial drugs;
- PCR method. It well identifies the causative agent of a sore throat of a viral nature. Mainly, the PCR method is useful in searching for and detecting the Epstein-Barr virus.
In addition, the patient is prescribed an ECG and ultrasound to understand whether there are pathological changes in the heart. Sometimes it is necessary to consult with more specialized specialists - an ophthalmologist, a neurologist or a cardiologist.
How is the treatment carried out?
Treatment of ulcerative glossitis in both adults and children should begin with eliminating the root cause of the problem, and this requires a thorough diagnosis. Only after identifying the source of the pathology can the doctor offer effective therapy. As for symptomatic treatment, to relieve acute inflammatory processes, specialists usually prescribe the drugs Hydrocortisone and Prednisopon. At an advanced stage and the presence of keratinized areas, they are removed surgically. Remember: only your doctor can prescribe medications; any attempts at self-medication can result in very unpleasant consequences.
To restore organ tissue, doctors usually prescribe rinse solutions with an antiseptic effect. These include “Furacilin” and “Chlorhexidine”. But to cope with pain, doctors usually prescribe drugs that have both anesthetic and antiseptic properties - Ledocaine and Kamistad. When answering the question of how to treat other forms of glossitis of the tongue, it is important to note that therapy is selected taking into account the type of pathology and the individual characteristics of the clinical picture.
Desquamative form of pathology
This form is widely known as “geographic language”. On the back of the organ, irregularly shaped light spots appear framed by a whitish coating. From the outside, the drawing somewhat resembles a map of the world, which is why the disease received its name among the common people. Most often, this type of glossitis becomes a consequence of pathological processes in internal organs and systems.
This is what geographic language looks like
Treatment is primarily aimed at achieving stable remission without exacerbations, since the desquamative type of the disease itself most often has a chronic form. Regular treatment of the organ and tissues of the oral cavity is required using anti-inflammatory gels and solutions, such as Chlorophyllipt or Karotolin. If the patient complains of severe pain, novocaine blockades and phonophoresis (ultrasound exposure simultaneously with drug therapy) are prescribed. The patient will also have to follow a special diet and take B vitamins.
Folded tongue
Quite deep and noticeable longitudinal and transverse grooves are formed on the back of the organ. Most often this is a congenital phenomenon, but there are cases when the pathology becomes a consequence of injuries, burns and infections. Symptomatic treatment of the folded form of glossitis is prescribed in the presence of severe discomfort, burning sensation, pain and breathing problems. In this case, antiseptic rinse solutions are prescribed, for example, Chlorhexidine, as well as anti-allergenic drugs if acute symptoms were provoked by an allergic reaction. During therapy you will have to give up salty and spicy foods.
This pathology is treated when causing inconvenience
Catarrhal type of disease
The development of the pathological process is accompanied by the formation of swelling, redness of individual parts of the organ, and the appearance of a dense white coating over the entire surface of the back. The cause of the problem may be a thermal or chemical burn or mechanical injury. As part of therapy, rinses with antiseptic and anti-inflammatory solutions are prescribed, nutrition is adjusted and vitamin complexes are prescribed.
Some problems can be solved by rinsing
Candidal glossitis
The distinctive symptoms of this pathology are a thick cheesy plaque and bad breath. In this case, patients usually do not experience significant discomfort or pain. Candidiasis infection, caused by too intense proliferation of yeast-like fungi Candida, can be triggered by an imbalance of microflora in the oral cavity after long-term drug therapy, taking antibiotics or insufficient hygiene.
Therapy in this case is aimed at restoring the balance of microflora. To do this, a complete sanitation of the oral cavity is carried out, antifungal drugs are prescribed, such as Nystatin or Fluconazole, and vitamin complexes are recommended to strengthen the immune system.
Diamond shape
The epithelial layer noticeably thickens and becomes thicker, taking on the shape of a diamond or rectangle, and a characteristic plaque appears. This type of illness usually indicates a malfunction of the gastrointestinal tract. Since most often this is only a symptom and not an independent disease, treatment should be aimed at eradicating the source of the problem, and rinsing with antiseptics and anti-inflammatory solutions is usually prescribed to relieve symptoms. If the patient complains of pain, painkillers are prescribed.
Purulent-phlegmous type of pathology
The lesion spreads to the deeper layers of the epithelium and may affect adjacent areas of the oral cavity. This is one of the most severe forms, during the development of which the patient’s temperature rises and all signs of intoxication of the body are noted. In such a situation, antibiotics are usually prescribed: Doxycycline, Ceftriaxone, Rocephin and others. In particularly severe clinical cases, surgical removal of the purulent neoplasm is performed, followed by monitoring the patient’s condition during the rehabilitation period.
Gunter's glossitis
This form develops against the background of serious pathological conditions associated with the functioning of the hematopoietic system. The disease is considered a frequent companion to anemia. In this case, the surface of the organ becomes unnaturally smooth and acquires an overly bright red or crimson color. It is necessary to treat first of all the anemia or pathology that has become the root cause of such symptoms. Vitamin B12 is often prescribed as part of therapy.
The photo shows Gunter's glossitis
"Hairy" tongue
Due to the thickening and keratinization of the filiform papillae covering the back of the tongue, the surface of the organ acquires a dark brown or even black color, its texture becomes rough, visually reminiscent of hard stubble. This type of pathology has been studied much less than others. Until now, experts cannot establish the exact prerequisites for its formation. Possible causes include genetic predisposition, infections, taking powerful medications and bad habits.
This pathology is eliminated surgically
To eliminate the defect, it is usually necessary to surgically remove the hypertrophied filiform papillae, after which antiseptic treatment of the oral cavity and anti-inflammatory therapy are prescribed.
Stages of disease development
The disease progresses rapidly. This is especially true in children and adults with a weakened immune response. Symptoms depend on the current state of the body, age, concomitant diseases and the stage of infectious tissue damage.
Signs of the development of the disease at different stages from the moment of infection:
- 2-3 days.
This stage is characterized by the maximum severity of the symptomatic picture. The patient's tonsils increase significantly in size and white or yellowish ulcers appear on their surface. The inflammatory process covers the entire surface of the tonsils. The patient notes deterioration in health, weakness, loss of appetite and signs of fever, including an increase in body temperature to 39-40 ° C. The patient also experiences excruciating pain in the throat, which gets worse when swallowing. - Day 4
The ulcers that form on the tonsils begin to spontaneously open, releasing the contents (pus). In their place, lacunae are formed - characteristic depressions. If at this stage the patient follows the doctor’s recommendations, the lacunae quickly close. - 5-6 day
. At this stage, patients feel a noticeable improvement in their condition - body temperature normalizes, headaches go away, strength and appetite are restored. - 7-10 day
. The last pathological sign – sore throat – recedes. The size of the lymph nodes located under the lower jaw also decreases. The patient ceases to feel pain and discomfort in this area.
Competent and timely therapy allows you to avoid serious complications.
Folk remedies - treatment at home
Traditional medicine is relevant only as an auxiliary therapy; with their help, you can quickly get rid of annoying symptoms and return to normal life. However, even in this case, you should not use certain home recipes on your own - first, consult your doctor and get his consent.
Chamomile decoction helps well in treatment
So, in order to speed up tissue restoration, it is recommended to make applications with rosehip oil and ointments with vitamin A - “Actovegin” or, for example, “Vinizol”. A chamomile decoction for rinsing or a light solution of hydrogen peroxide will help relieve severe inflammation. Tea tree oil has excellent wound healing properties.
Diagnosis and treatment
To make a diagnosis and determine treatment approaches, you need to consult an otolaryngologist. Diagnostics is carried out according to the following algorithm:
- collection of medical history and complaints;
- examination of the pharynx using special lighting (pharyngoscopy);
- general and biochemical blood test;
- bacteriological examination of a smear with the preparation of an antibiogram.
How to treat a purulent sore throat is determined by an ENT specialist. In severe cases, hospitalization is required. General medical recommendations include bed rest, drinking plenty of fluids, taking vitamins and restorative medications.
Specific treatment of the disease is a complex of procedures and medications:
- Drug treatment of the oral cavity.
Complex therapy necessarily includes gargling with antiseptic solutions. For this purpose, solutions of furatsilin, manganese, hydrogen peroxide, sea salt, and natural herbal decoctions (chamomile, calendula) are used. This procedure is aimed at removing pathogenic microorganisms from the throat and mouth. - Taking systemic antibacterial drugs.
A full course of antibiotic therapy allows you to get rid of pathogenic flora. Antibiotics and their dosages can only be determined and prescribed by a doctor. The most commonly used drugs are from the groups of penicillins, macrolides and cephalosporins. - Symptomatic therapy.
To alleviate the patient’s condition during the acute stage, the specialist prescribes symptomatic treatment in the form of antipyretics, antihistamines and anti-inflammatory drugs. Sometimes it is recommended to undergo physiotherapeutic procedures during the recovery period.
Correctly selected treatment helps to avoid serious consequences and ensures healing of the affected tissue areas without visible defects.
Preventing tongue ulcers
No one is immune from microtraumas to the mucous membrane and the appearance of minor wounds on its surface. However, provided you have good health, good immunity and good hygiene, such a minor nuisance is unlikely to lead to serious problems. To protect yourself from diseases of the teeth and soft tissues of the oral cavity, it is enough to maintain hygiene, regularly brush your teeth, visit the dentist for preventive maintenance and professional dentistry. hygiene at least once every six months.
Preventive examinations at the dentist will help to recognize pathology in time
It is also advisable to monitor the health of the body as a whole, give up cigarettes and alcohol, diversify your diet with healthy foods, take vitamins from time to time to strengthen the immune system, and try to lead an active lifestyle.
Prevention
By paying attention to preventive measures, you can reduce the risk of developing the disease. Effective prevention includes:
- avoiding hypothermia (wearing warm clothes, monitoring microclimatic indicators in the room);
- regular preventative visits to the dentist to identify the early stages of caries and stomatitis;
- giving up bad habits (smoking, drinking alcohol);
- moderate physical activity, regular walks in the fresh air;
- normalization of diet, sleep and wakefulness;
- compliance with hygiene standards and requirements, maintaining cleanliness in the home and workplace;
- limiting contacts with unfamiliar people during periods of unfavorable epidemiological conditions.
Strengthening the immune system based on leading a healthy lifestyle helps to avoid infection and make it easier to endure purulent sore throat.
If you have a sore throat, call us and we will definitely help you!
Which doctor treats glossitis and when should you contact him?
When suspicious ulcers are discovered on the tongue, many begin to ask a completely logical question regarding which doctor to turn to for help. In such a situation, you can, of course, immediately make an appointment with a dentist, but it is not a fact that the pathology was caused by a dental problem, and this specialist will be able to provide the necessary assistance. It is better to first consult with your attending physician - after a visual examination, he can send the patient for additional examination, the necessary tests, or immediately refer him to a highly specialized doctor: a gastroenterologist, endocrinologist, immunologist, or again to a dentist.
The formation of strange suspicious spots, plaque and ulcers on the surface of the main speaking organ, the occurrence of obvious pain, burning and tingling sensations - all these are signs of tongue pathology. If we are talking about glossitis, then it can be an independent disease, since it is a secondary sign of disturbances in the functioning of internal organs and systems. In any case, the problem requires an immediate solution, so in such a situation the only correct instruction for action is to urgently consult a doctor.
- Kharitonova, M. P. Burning tongue syndrome (Etiology, clinical picture, differential diagnosis, treatment), 2000.
Incubation period
The period from the moment the pathogen enters the body until the appearance of the first characteristic symptoms can range from 2 to 6 days. During the first few days, the sick person is still unaware of his condition, becoming a source of infection for others. During the incubation period, the infection is actively transmitted by airborne droplets (through coughing, sneezing, kissing, talking). The onset of the disease is manifested by a feeling of chills, increased body temperature, weakness and headache. The sooner the patient sees a doctor, the easier the treatment is.