From this article you will learn:
- what is a dental cyst - symptoms, photos,
- why does it form?
- cyst on the root of a tooth - treatment.
The article was written by a dentist with more than 19 years of experience.
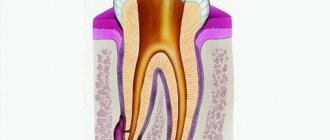
A dental cyst is a round-shaped inflammatory formation, which is a cavity in the bone tissue, which is lined from the inside with a fibrous capsule and filled with purulent contents (Fig. 1). In dentistry, the terms “root cyst of the tooth” or “radicular cyst” (from the word radix - root) are most often used to refer to this pathology. This is due to the fact that the most common place for its formation is the area of the apex of the tooth root.
The formation of a cyst on the root of a tooth is associated with an infection in the root canals. Most often it appears - 1) either in the absence of timely treatment of pulpitis or periodontitis of the tooth, 2) or is a consequence of poor-quality root canal filling. The formation of a cyst occurs gradually and over a long period of time. First, at the apex of the root, under the influence of infection in the root canals, a small apical granuloma is formed, which subsequently increases in size and transforms into a cyst filled with pus.
What does a dental cyst look like: photo
Pay attention to how a cyst on the root of a tooth looks on an x-ray - it looks like intense darkening at the apex of the tooth (for your convenience, we have limited this area with arrows). Such intense darkening at the apex of the tooth root indicates the presence in the bone tissue of a site of bone destruction in the form of a cavity. In Fig. 3 you can see what a cyst looks like at the apex of the root of an extracted tooth (like a sac filled with pus).
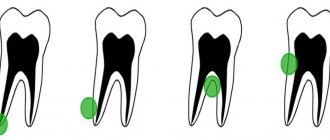
This article is written for patients and therefore will contain unnecessary medical details. But to complete the picture, it is worth adding that a dental cyst can be localized not only at the apex of the tooth root, but also on the lateral surface of the root, as well as between the roots of multi-rooted teeth - in the root bifurcation zone. But such localizations of root cysts are quite rare, and therefore we will examine in more detail the symptoms and treatment of a dental cyst localized at the apex of the root.
Type of cyst on the root of an extracted tooth (video 1) –
Tooth cyst: symptoms
If a dental cyst occurs, there may be no symptoms at all for a long time. In this case, jaw cysts are diagnosed accidentally, for example, during a routine X-ray examination before the start of prosthetics (usually a panoramic photograph of the teeth is taken for this - an orthopantomogram). But minor symptoms may still occur. For example, there may be periodic minor pain when biting on the causative tooth or slight pain when pressing on the gum in the projection of the tooth root.
Moreover, the patient will feel such symptoms inconsistently, but only periodically. For example, they can occur after hypothermia, against the background of decreased immunity and colds. In very rare cases, sharp pain may occur when biting on the causative tooth, against the background of which swelling of the gums and even soft tissues of the face may also be observed. Against the background of an exacerbation, slight mobility of the tooth with a cyst may also appear. Also, as a rule, such an exacerbation may be accompanied by a slight fever and weakness.
In some cases, a dental cyst can be suspected not only by these secondary signs. Sometimes you can even see it, of course, if it reaches a large size. If left untreated, the size of the cysts slowly increases, which is associated with the constant production of pus into the cyst cavity. An increase in the amount of pus in the cyst cavity leads to an increase in the pressure of the cyst on the walls of the bone cavity surrounding it. Under such pressure, the bone tissue is slowly resorbed and the cyst expands. I have operated on a number of patients whose cysts reached 3-4 cm in diameter.
On the upper jaw, root cysts increase in size much faster than on the upper jaw. This is due to the fact that the bone tissue of the upper jaw is softer and more porous in structure, and therefore its resorption always occurs faster. If a root cyst occurs in the premolars and molars of the upper jaw (teeth 4-5-6-7-8), the cyst may even occupy the entire volume of the maxillary sinus, and removal of the dental cyst in this case will require a maxillary sinus. In some cases, large root cysts may be visible during examination of the oral cavity, and not just on a targeted or panoramic x-ray.
Root cyst on the upper jaw (view in the oral cavity) –
Please note that, as in this case, the cyst deformed the hard palate. Such deformations can be observed not only in the palate, but also on the anterior side of the alveolar process of the upper and lower jaw. Very often, large cysts lead to complete destruction of bone tissue on the anterior surface of the alveolar process of the jaw (in the projection of the root of the causative tooth). And it turns out that under the mucous membrane in this area there will be a fibrous membrane of the cyst. In this case, during palpation you will not feel the hard bone; the finger will fall inward a little.
In what cases might you suspect you have a root cyst? –
Firstly, if you periodically experience discomfort or slight pain in one of your teeth when biting (in this case, gentle tapping on the tooth will also cause discomfort). But such symptoms are usually characteristic of apical periodontitis, which, by the way, also needs to be treated urgently. But what is not typical for ordinary apical periodontitis, but is typical for a root cyst, is pain on palpation of the gums in the projection of the root of the causative tooth.
Therefore, if there is discomfort in one of the teeth when biting, you can palpate (press) with your finger on the gum in the projection of the root of this tooth. Pain when pressed is highly likely to indicate the presence of a cyst at the root of the tooth (24stoma.ru). This diagnosis may also be supported by the presence of a dense or soft “bulging” of the gums in the projection of the root of the causative tooth, which can occur when the root cyst reaches a large size.
Cystadenoma and cystadenofibroma of the ovary
These formations are also common cystic ovarian tumors (cystomas), which can be either serous or mucinous (mucous). On ultrasound, mucinous cystadenoma often appears as an anechoic, unilocular mass that may resemble a simple cyst. Mucinous cystadenomas often consist of several chambers, which may contain complex fluid with inclusions of protein debris or blood. “Papillary” protrusions on the walls suggest a possible malignancy (cystadenocarcinoma).
Ovarian cystoma on ultrasound. Transvaginal examination (top left) reveals a left ovarian cyst measuring 5.1x5.2 cm (anechoic and without septa). However, a nodule is found on the posterior wall of the cyst with no evidence of internal blood flow on Doppler examination (top right); The differential diagnostic range includes a follicular cyst, an accumulation of debris, and a cystic neoplasm. On MRI (below), thin septa accumulating contrast are detected in the formation. No tumor nodes, lymphadenopathy, or peritoneal metastases were detected. The minimum amount of ascitic fluid is determined. The formation was verified as a cystadenoma by biopsy.
Ovarian cystoma: MRI. On MRI scans performed on the same patient five years later, the mass had grown. On T2 WI a complex cyst is visualized in the left ovary with a solid node on the posterior wall. After contrast administration, a slight increase in signal intensity from thin septa and a node in the wall is detected on T1 FS. MRI data did not allow differentiating between benign (eg, cystadenoma) and malignant ovarian neoplasms. Histological examination of the resectate confirmed cystadenofibroma.
X-ray diagnostics –
As we said above, the final diagnosis can only be made using an x-ray, on which a cavity formation in bone tissue will always look like a rounded darkening.
In the x-ray images below we have presented you with 3 options for localizing root cysts. The most common location is root cysts at the apex of the tooth root, but cysts on the lateral surface of the root or located between the roots of multi-rooted teeth are much less common. Radiographs of root cysts of different locations –
Types of ovarian cysts in women
There are main types of ovarian cystic formations:
Physiological cysts are normal
- Follicle
- Corpus luteum
Functional cysts
- Follicular cyst
- Corpus luteum cyst
- Thecal lutein cysts
- Complicated functional cysts: hemorrhagic cyst, rupture, torsion
Benign cystic tumors (cystoma)
- Dermoid cyst (mature teratoma)
- Serous cystadenoma
- Cystadenoma mucinous
- Cystedenofibroma
- Sclerosing stromal tumor
Malignant cystic tumors (cystomas)
- Serous cystadenocarcinoma
- Cystadenocarcinoma mucinous
- Endometrioid cancer
- Brenner's cystic tumor
- Immature teratoma
- Cystic metastasis
Other cysts
- Endometrioma (chocolate cyst)
- Polycystic ovaries (Stein-Leventhal syndrome)
- Postmenopausal cyst
- Ovarian hyperstimulation syndrome
Cyst on the root of the tooth: causes
As we said above, the formation of a cyst on the root of a tooth is associated with an infection in the root canals. Root canals open at the tops of the roots with small holes, which means that during inflammation, bacteria and their toxins will travel outside the tooth, forming foci of inflammation at the tops of the roots. At the first stage, a so-called apical granuloma (up to 0.5 cm in size) is first formed at the root apex, which is a section of granulation tissue surrounded by a loose fibrous capsule.
Such a granuloma does not yet have a cavity with pus inside, but with a further increase in its size (over 0.5 cm), a cavity is formed inside it, lined from the inside with epithelial cells. Such a cavity formation already corresponds to the concept of “root cyst,” although in dentistry small root cysts ranging in size from 0.5 to 1.0 cm are often also called the transitional term “cystogranulomas.” And the root cyst itself is most often called a formation with a diameter of more than 1.0 cm. Inside the cavity of the cyst there is pus, which is produced by its inner membrane.
Learn more about the reasons for the development of a cyst at the apex of the tooth root -
Infection in the root canals does not occur on its own, and this is not some kind of psychosomatics and related problems, for example, bronchial asthma. Infection in the tooth cavity and root canals occurs in the following two situations:
- Untreated caries, pulpitis and periodontitis - tissues affected by caries contain a large number of cariogenic microorganisms. If caries is not treated, then bacteria gradually enter the dental pulp (neurovascular bundle), causing inflammation in it - pulpitis. If pulpitis is not treated in time, which should consist of removing the infected pulp and filling the root canals, the infection penetrates through the root canals outside the tooth. This leads to the development of a focus of inflammation at the apex of the tooth root, followed by the formation of a root cyst (Fig. 5).
- Poorly sealed root canals - imagine that you have cured your pulpitis in time or the inflammation that has just begun at the apex of the tooth, but after some time you still have a cyst formed at the apex of the root. This happens very often and is due to the fact that the root canals were filled poorly (according to official statistics, dentists fill root canals poorly in 60-70% of cases). The fact is that the infection develops in the unfilled part of the root canal or where the canal was not tightly filled with a filling substance.
Normally, each root canal of a tooth should be filled to the apex of the root. If the canal is not filled to the top of the root, then an infection develops in the unsealed part of the canal, which penetrates beyond the tooth and also causes the formation of a cyst. In Fig. 6-7 you can see radiographs of teeth whose root canals were poorly filled, which in both cases caused the formation of a dental cyst. In Fig. 6, white arrows mark unfilled areas of the root canals. In Fig. 7, only traces of filling material are visible in the root canal, i.e. The root canal is not sealed tightly and not all the way.
Reasons for the development of root cysts in other locations –
The appearance of a root cyst on the side surface of a tooth is usually due to the fact that numerous small branches (opening with holes on the side surface of the root) always extend from the main root canal in the root of the tooth. Therefore, even with high-quality filling of the main root canal, there is a very small risk of a granuloma or cyst appearing on the lateral surface of the root.
A little more often you can find a cyst in another location - between the roots of multi-rooted teeth (in the bifurcation of the roots). Such a cyst usually occurs if the integrity of the hard tissues of the bottom of the tooth cavity is damaged, for example, as a result of a crack or perforation of the bottom of the tooth cavity, or perforation of the upper half of one of the root canals. Such complications are most often the result of dentist mistakes in the treatment of pulpitis and periodontitis.
Inflammation of the appendages (salpingoophoritis) and tubo-ovarian abscess
Tubo-ovarian abscess usually occurs as a complication of an ascending (from the vagina to the cervix and fallopian tubes) chlamydial or gonorrheal infection. CT and MRI reveal a complex cystic formation of the ovary with a thick wall and lack of vascularization. Thickening of the endometrium or hydrosalpinx makes the diagnosis of tubo-ovarian abscess more likely.
An axial contrast-enhanced CT scan reveals a complex cystic formation on the left, resembling an abscess, with a thick wall accumulating contrast and gas inclusions inside.
On a CT scan in the sagittal plane (left), it can be seen that the ovarian vein approaches the mass, confirming its nature (arrow). On the coronal tomogram (right), the anatomical relationships of the mass and the uterus can be assessed. A gas bubble is visualized in the uterine cavity, which suggests an infectious onset here, with subsequent spread of infection through the fallopian tube to the ovary.
Tooth cyst: treatment
If you have a cyst on the root of a tooth, treatment can be conservative (therapeutic) and surgical. Conservative treatment will consist of treating the cyst with a special medicinal paste based on calcium hydroxide, which will temporarily fill the root canals. Accordingly, if the root canals have not been filled, the tooth is opened and the root canals are mechanically treated. If the root canals have already been sealed, but poorly, they are first unsealed.
Below we will show how therapeutic treatment of a dental cyst is carried out using a specific example. It should be noted that good results with conservative therapy can be achieved even when treating fairly large cysts. However, there are situations where conservative therapy is less optimal than surgical removal of the cyst.
Surgical treatment is reasonable if...
- If the root canal is filled, but there is a pin in it, and there is a risk of fracture of the tooth root when removing the pin from the canal.
- If the root canal is filled, and the tooth has an artificial crown or is the support of a bridge (after therapeutic treatment of the cyst, the crowns will have to be redone, and this costs money).
- For large cysts.
- If the cyst arose as a result of perforation of the tooth root.
- If the cyst often suppurates, for example, every time you try to temporarily fill the root canals with medicinal paste.
A prerequisite (including in the presence of a pin and a crown) is that the root canal must be well sealed for at least 2/3 of its length. This will allow you to cut off the root apex with the unfilled part of the canal, removing it along with the cyst shell, and at the same time maintaining sufficient length of the root so that it can withstand the chewing load. A very important point is the convenience of surgical access, so surgical removal of a cyst is rarely performed, for example, in 6-7 teeth.
Therapeutic treatment of cysts using a specific example -
Let’s say right away that this method of treatment is very long (at least 2-3 months), it will require numerous visits to the dentist, and it is also the most financially expensive. The sequence of actions will be as follows (we will describe the main stages below):
- Working with tooth root canals – if the root canals of the tooth have not been previously filled, then at the first stage the dead pulp is removed from the tooth and instrumental treatment of the root canals is carried out. If the root canals have already been filled, then they are first unsealed. In this case, the cyst arose due to insufficient filling of the root canal to the root apex (Fig. 8).
Because the canal was previously sealed, then it must first be unsealed, which was done (Fig. 9). In fact, in this situation, it was much easier and cheaper for the patient to perform a resection operation. It would last about 30 minutes, and you could forget about the cyst. But the patient refused surgical treatment due to fear.Example of treatment of a root cyst (Fig. 8-12) –
- Medicinal treatment of canals - the cyst contains pus, therefore, after unsealing the canals or removing the pulp, numerous rinsing of the root canal with antiseptics is required.
- Temporary filling of the canals with medicinal paste - first, using special instruments, a medicinal substance is removed from the apex of the root (directly into the cavity of the cyst), which has a powerful antiseptic effect. For this purpose, a paste based on calcium hydroxide is used. The same substance is then used to temporarily fill the root canal (Fig. 10).
- Repeating points 3 and 4 - if the cyst is large, then over the next few months you will need to make a couple of visits to the dentist. This is necessary to change the medicine, as well as to take a control x-ray to assess the dynamics of the reduction of the cyst.
- X-ray control – the effectiveness of treatment is assessed. A significant reduction in the size of the cyst on x-ray indicates the effectiveness of the therapy (the structure of the newly formed bone is even visible in the image), and in this case, you can proceed to the next stage - permanent filling of the root canals.
- Permanent filling of the root canals - if a decrease in the size of the cyst is noticed over the course of several months during treatment, then the root canals are finally filled, usually with gutta-percha (Fig. 11). Immediately after this, you can begin to restore the crown part of the tooth.
After the root canals have been completely filled and a filling has been placed, the patient must visit the doctor every few months and take a control x-ray. The image clearly shows the dynamics of cyst reduction and bone tissue restoration. Compare the X-ray image in Fig. 12 (taken 2.5 months after the start of treatment) with the image before the start of treatment in Fig. 8. The naked eye can see a reduction in the size of the cyst and restoration of the bone beams.
Emergency care for exacerbation of inflammation -
We have already said above that dental cysts are usually characterized by a chronic, sluggish course of the inflammatory process. However, in some cases, a sharp exacerbation of the process may occur - with the appearance of acute pain when biting on a tooth and/or swelling of the gums in the projection of the cyst. When a patient goes to the dentist due to an exacerbation, the tooth is immediately opened to allow the drainage of pus from the cyst cavity (through the root canals). You can see how this happens in video 1.
If there is swelling on the gum, the patient is sent to a dental surgeon to make an incision in the gum. You can see how the gum incision is made in video 2. After this, the tooth is left open, and the patient is prescribed antibiotics, antiseptic rinses, and non-steroidal anti-inflammatory drugs.
Well, in conclusion, I would like to say about how dangerous a dental cyst is if it is not treated. Root cysts slowly increase in size, and imagine that there is a 2-3 cm cavity filled with pus in your head. A growing cyst, for example, can engulf the roots of neighboring teeth, which will require filling the canals in them as well. In addition, the cyst can grow into the maxillary sinus and do many other bad things. We hope that our article on the topic: Dental cyst treatment was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a dentist, 3. National Library of Medicine (USA), 4. “Outpatient surgical dentistry” (Bezrukov V.), 5. “Therapeutic dentistry: Textbook” ( Borovsky E.).
Ovaries after menopause
Entering the postmenopausal period is defined as the absence of menstruation for one year or more. In Western countries, the average age of menopause is 51–53 years. In postmenopause, the ovaries gradually decrease in size and Graafian follicles stop forming in them; however, follicular cysts may persist for several years after menopause.
On a T2-weighted MR image (left) of a postmenopausal woman, the ovaries appear as dark “clumps” located near the proximal end of the round ligament. On the right, the tomogram also visualizes a hypointense left ovary, devoid of follicles. Although it is slightly larger than expected, overall the ovary appears completely normal. And, only if it is possible to detect an increase in the size of the ovaries compared to the initial study, the differential diagnostic series should first of all include a benign neoplasm, for example, fibroma or fibrothecoma.
Malignant cystic ovarian tumors
Radiation diagnostic methods, such as ultrasound or MRI, are not intended to determine the histological type of tumor. However, with their help it is possible to differentiate benign and malignant neoplasms with varying degrees of certainty and determine further tactics for patient management. Detection of radiation signs of malignant tumor growth should direct the attending physician (gynecologist, oncologist) to further actively determine the nature of the cyst (surgery with biopsy, laparoscopy). In unclear and contradictory cases, it is useful to re-interpret the MRI of the pelvis, as a result of which you can get a second independent opinion from an experienced radiologist.
Get an MRI of the ovaries in St. Petersburg
Refusal of surgery: possible complications
If the ovarian cyst is not removed in a timely manner, the following complications may occur:
- Cyst rupture;
- Torsion of the cyst pedicle;
- Degeneration of a benign formation into a malignant tumor;
- Inflammation of the uterine appendages;
- Infertility.
When a cyst ruptures, fluid that was inside the formation enters the abdominal cavity. Women experience severe pain, nausea, vomiting, and body temperature rises.
A cyst can sometimes develop into a malignant tumor. Malignancy is detected during ultrasound examination. If the neoplasm is malignant, during an ultrasound examination, doctors identify extensive wall seals and the presence of pathological blood flow.
For differential diagnosis, oncologists determine the blood level of the tumor marker CA-125. An increase in its concentration is not an accurate confirmation of the cancer process.
In the absence of adequate treatment for ovarian cysts, purulent inflammation may occur in the uterine appendages. Subsequently, peritonitis develops - inflammation of the peritoneum.
In advanced cases, the disease can lead to the removal of the reproductive organs - the ovaries and uterus. Consequently, the woman is deprived of the opportunity to have a child.
Endometrioid ovarian cancer
Bilateral cystic solid ovarian masses are suspicious for tumor and require further evaluation. The importance of radiological research methods is to confirm the presence of formation; however, it cannot be concluded with absolute certainty that it is benign or malignant. For patients who have epithelial tumors (a much more common group of ovarian neoplasms), even after surgical treatment, determining the exact histological type of the tumor does not affect the prognosis as much as FIGO stage, degree of differentiation, and completeness tumor resection.
The sonogram (left) shows enlargement of both ovaries, inside of which there is both a cystic and soft tissue (solid) component. A CT scan of the same patient reveals a large cystic-solid formation extending from the pelvis to the abdomen. The role of CT in this case is to stage the formation, however, based on CT (MRI) it is impossible to determine the histological structure of the tumor.
Aneurysmal
An aneurysmal bone cyst is a benign tumor-like formation, which, unlike a solitary cyst, has numerous vascular spaces filled with blood. It progresses rapidly and predominantly affects the pelvic bones, vertebrae and knee joint (metaphyses of the femur and tibia), but is less common than solitary.
ACC can be present in children of any age and gender, but most often this bone cyst is diagnosed in adolescents, namely girls 10-20 years old. Among all bone neoplasms, it accounts for 1–9.1%.
For what reasons degenerative bone cysts of this type are formed have not yet been fully studied, but it is also assumed that its formation provokes a local disturbance of venous outflow. Trauma can also cause the formation of an aneurysmal cyst. Less commonly, this bone cyst in children acts as an element in the structure of another tumor.
Where did she come from?
The main function of the ovaries is the production of special hormones that regulate the maturation of the follicle and the release of the corpus luteum from it.
In the middle of the menstrual cycle, the follicle bursts, the egg is released and ovulation occurs. If ovulation does not occur, the unbursted follicle continues to develop and fluid accumulates in it. This cavity is called a cyst. With normally functioning ovaries, the cycle is reversed: that is, the corpus luteum should disappear. If this does not happen, after ovulation, excess fluid accumulates in the corpus luteum, which also leads to the formation of a cyst.
A cyst can also form from the appendages, then this bubble with liquid is entwined with tiny blood vessels.
Rehabilitation
The oncology clinic of the Yusupov Hospital has all the conditions for successful rehabilitation, which lasts from 10 days to a month. All actions during this period are aimed at restoring the reproductive functions of the body, preventing relapse of the disease, as well as normalizing the psycho-emotional state of the patient.
The rehabilitation program of the Yusupov Hospital includes several stages:
- Taking hormonal drugs;
- Phonophoresis;
- Diet correction;
- Laser or magnetic laser therapy;
- Physiotherapy.
During this time, it is necessary to abstain from sexual intercourse, heavy physical activity, and sports. After the end of the rehabilitation period, the woman can return to her usual lifestyle.
Serous cystadenocarcinoma
Ultrasound reveals a complex cystic-solid formation in the left ovary, and another large complex formation containing both a solid and a cystic component in the right half of the pelvis
A CT scan of the same patient reveals a complex cystic-solid formation with thickened septa accumulating contrast in the right ovary, extremely suspicious for a malignant tumor. There is also bilateral pelvic lymphadenopathy (arrows). Histopathological examination confirmed serous ovarian cystadenocarcinoma (the most common variant)
CT scan and macroscopic photograph of serous ovarian cystadenocarcinoma.
Ultrasound (left) shows a large multilocular cystic formation in the right parametrium; Some of the chambers are anechoic; in others, uniform low-level echogenic inclusions are visualized, caused by protein content (in this case, mucin, but hemorrhages can also look similar). The partitions in the formation are mostly thin. No blood flow was detected in the septa, the solid component was also absent, and no signs of ascites were detected. Despite the absence of blood flow during Doppler ultrasound and a solid component, the size and multilocular structure of this formation allows us to suspect a cystic tumor and recommend other, more accurate diagnostic methods. Contrast-enhanced CT scan (right) shows similar changes. The formation chambers have different densities, corresponding to different protein contents. Histopathological examination confirmed mucinous cystadenocarcinoma with low malignant potential.
Cystic metastases to the ovaries
Most often, metastases to the ovaries, for example, Krukenberg metastases - screenings of stomach or colon cancer, are soft tissue formations, but often they can also be cystic in nature.
A CT scan reveals cystic formations in both ovaries. You can also notice a narrowing of the rectal lumen caused by a cancerous tumor (blue arrow). Cystic metastases of rectal cancer are clearly visible in the recess of the peritoneum (red arrow), which in general are not a typical finding.
Functional neoplasms
When diagnosing functional formation, 90% use conservative methods. It uses hormonal drugs that affect the follicular and luteal capsules. Gynecologists most often choose progesterone-based tablets “Regulon”, “Janine”, which reduce the concentration of estrogen in the blood. After treatment, to stabilize hormonal levels, Duphaston courses are prescribed for up to 2 months.
Sometimes experts may recommend using traditional medicine methods. Most often this is brewing infusions of chamomile, calendula and other herbs that help activate the immune system and reduce pain. But traditional medicine methods are used exclusively in an auxiliary role and cannot replace drug treatment.
It is important to take into account that after 50 years, functional cysts do not form, which is due to physiological changes in the female body. At this age, the risk of malignancy of other types of formations is highest.
Possible consequences of the operation
After removal of an ovarian cyst, patients at the Yusupov Hospital spend about five days in the inpatient department of the oncology clinic, where the level of comfort corresponds to European standards. During this period, women undergo rehabilitation under the supervision of experienced specialists
After removal of the cystic formation, the biological material is sent for histological examination. Experienced morphologists at the hospital determine the nature of the neoplasm. During histological examination, specialists study the structure of the tissues of the cyst wall.
Histology makes it possible to distinguish an ovarian cyst from a borderline form of tumor and cancer. In order to prevent complications in the late postoperative period, hospital doctors monitor patients after removal of an ovarian cyst until final recovery. In the future, gynecologists regularly conduct preventive examinations.
Hormonal drugs
Conservative treatment is based on the use of various combinations of hormonal drugs. Gynecologists prescribe the following groups of drugs:
- If there is a deficiency or excess of hormones - “Duphaston”, “Urozhestan”.
- If it is necessary to reduce the level of the hormone that provokes the growth of formation - “Diane”, “Janine”, “Regulon”.
- To eliminate inflammatory processes - “Indomethacin”.
- To eliminate pathogenic microflora - “Vancomycin”, “Lincomycin”.
- To stimulate the immune system – “Timalin”.
To normalize hormonal levels and regression of education, specialists prescribe oral contraceptives. For treatment, a special drug regimen is developed. In some cases, COC therapy is combined with the use of gestagens, which block the pituitary gland and promote temporary replacement of hormones with artificial derivatives.
The drug Duphaston with the main active ingredient – Dydrogesterone – has proven itself especially well. The drug is actively used for the treatment of follicular formations and endometriosis. In the first case, it promotes the correct transition from the first to the second phase of the menstrual cycle, and in the second, it prevents the growth of the endometrium and the appearance of new capsules.
This drug is prescribed only by a doctor, who determines the dose and treatment regimen based on:
- Data obtained during the inspection.
- Nature of the pathology.
- Age.
- Analysis results.
In some cases, after taking large doses of the drug, side effects are observed, such as migraines, rashes, bleeding. But with proper treatment and dose selection, hormonal levels are normalized and the cycle improves.
If the inflammatory process or cyst formation is caused by pathogenic microflora, the doctor may prescribe broad-spectrum antibiotics that can eliminate diseases of the reproductive system.
If the urinary system is disrupted, diuretics are prescribed, and if the formation is inflamed, anti-inflammatory drugs are prescribed. Additionally, agents that enhance immunity are used, for example, folic acid, vitamin C, E. To minimize pain, use Diclofenac or No-shpa.
To enhance the effect of medications, various physiotherapeutic treatment methods are prescribed. Most often used:
- Electrophoresis.
- Ultraphonoresis.
These procedures make it possible to enhance the effect of medications, normalize the function of the damaged organ, and prevent the development of inflammation. Physiotherapy is also used during the recovery period to reduce the likelihood of relapse, improve blood circulation and other factors.