A pimple on the gum indicates the need to see a dentist. Unlike acne on the skin, rashes on the mucous membrane cannot be treated on your own. Treatment should be selected by a specialist, taking into account the type and causes of the formation. The mucous membrane is the most favorable environment for the proliferation of harmful microorganisms. By piercing or squeezing such a formation, there is a risk of getting a more serious infection.
A white pimple on the gum indicates an inflammatory process with suppuration inside, but even when there is no suppuration yet, it is better to see a dentist. The problem can be solved with simple home rinses, but there are cases when surgical intervention is necessary.
Pimple on the gum - what to do?
The treatment scenario depends on the reasons that caused the rash on the gums. In addition to clinical treatment, a number of home measures can be taken. For example, if the rash is associated with the spread of Candida fungus in the mouth or with stomatitis, regular rinsing, taking special medications and treating the mucous membrane help. A purulent pimple on the gum may be a consequence of a viral infection of the body, in which case antiviral drugs are prescribed. The treatment must be selected by the dentist. The doctor will explain how to rinse a pimple on the gum and what habits will need to be reviewed. If a rash appears, it is recommended to exclude certain foods from the diet:
- fried foods and dishes high in oil;
- solid foods - nuts, raw vegetables such as carrots, etc.;
- very hot or cold dishes - food should be at room temperature;
- spicy, sweet and sour.
It is important that the diet does not contain foods that can further irritate the mucous membrane. Dentists also recommend abstaining from soda during treatment. Mostly you will need to switch to a liquid diet; you can leave purees and well-cooked porridges.
A white pimple on the gum may be fatty. In this case, the dentist should observe the changes for some time without intervention - the fat will resolve on its own. They rarely increase, but such development is possible. Then surgical removal is necessary.
A rash on the gums may indicate stomatitis, candidiasis or herpetic infection. An individual treatment regimen is selected for each situation. Taking medications is combined with preventive measures such as adjusting the diet. Severe inflammation is treated with a course of antibiotics. If the rash is accompanied by pain in the mouth, the doctor prescribes antiseptic solutions or gels to reduce pain.
Drug treatment
How to treat acne on the gums depends on the diagnosis and the cause of the pathology.
| Diagnosis (cause) | Indications for treatment | Possible drugs |
| Candidal (fungal) stomatitis | They use rinses, topical preparations with antifungal action, and oral medications in tablet form and capsules. Diet is required - exclusion of sweets and yeast-based products. | "Candide" "Clotrimazole" "Fluconazole" "Pimafucin" |
| Herpetic stomatitis | In addition to rinsing, antiviral agents and drugs that enhance immunity are indicated. | "Immunal" "Interferon" "Acyclovir" |
| Purulent acne | Antibacterial drugs are prescribed, depending on the complexity of the case - tablets or injections. Rinsing the abscess with antimicrobial solutions. | "Tarivid" "Metronidozole" "Lincomycin" (for rinsing) |
If your gums hurt due to acne, medications in gel form containing lidocaine, for example, Kamistad, are prescribed. In addition to the analgesic effect, it has an anti-inflammatory and antimicrobial effect. “Kalgel”, “Cholisal”, “Mundizal” have similar properties.
Based on the clinical picture, the specialist may prescribe antipyretic and anti-inflammatory drugs. Particular attention is paid to rinsing the mouth with antiseptic solutions: “Furacilin”, “Chlorhexidine”, “Miramistin”, “Rotokan”.
What kind of pimple is on the gum?
Only a dentist can accurately diagnose inflammation. Conventionally, rashes are divided into 7 types:
- Transparent. A white bubble on the gum of a child or adult most likely indicates herpetic stomatitis, which occurs due to damage to the body by the herpes virus. Swelling of the mucous membrane can occur in parallel with enlarged lymph nodes and be accompanied by severe itching.
- White. A hard lump that is white or yellowish in color. It may turn out to be a wen that will resolve on its own. If this is him, there will be no other symptoms of inflammation.
- Purulent or bloody inflammations. Most often this is the result of stomatitis, which occurs due to infection in the mucous membrane. The disease appears when there are wounds on the oral mucosa, for example, due to wearing braces. The reasons can also be more trivial - for example, a deep scratch from a fish bone.
- Multiple white pimples on the gums of an adult or child. The pimples themselves or the plaque next to them are white. At the same time, itching is felt in the mouth, sometimes inflammation is accompanied by internal swelling. Such symptoms indicate damage to the oral cavity by Candida fungus.
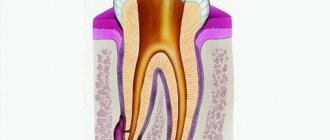
- Cystic formations. A cyst is a dense lump containing pus inside. It is rarely accompanied by symptoms, but sometimes there is aching pain. The causes are different - from caries and advanced gum inflammation to periodontitis and pulpitis. The cystic tumor is red, but if you press on it a little it turns white due to the pus inside. The size of the cone sometimes reaches a couple of centimeters. The pus inside can destroy bone tissue, so if a cyst-like formation appears, you should immediately make an appointment with a dentist.
- Flux. Inflammation that occurs on the periosteum due to periostitis. In addition to a large white or red pimple, severe inflammation appears. The gum swells and the cheek along with it.
- Abscess. The last stage to which a cyst, flux or purulent formation develops. The pus inside the inflamed tissue destroys it and a cavity appears. Due to the abscess, fistulas appear - these are channels for the removal of pus. They look like holes or pimples that are about to burst. Most often, people faced with such a problem are interested in whether it is possible to pierce a fistula on the gum on their own? A dentist should work with a fistula using sterile equipment. If you puncture yourself, you risk aggravating the situation.
Clinical trials
According to the results of clinical trials of the ASEPTA rinse after 3 weeks of use of the rinse, gum bleeding is reduced by 28.3%, inflammation is reduced by 32.3% and the hygienic condition of the oral cavity is improved by 33.5%.
Sources:
- Clinical experience in using the Asepta series of products Elena Ivanovna Fuchs, assistant at the department of therapeutic and pediatric dentistry. State budgetary educational institution of higher professional education Ryazan State Medical University named after Academician I.P. Pavlova of the Ministry of Health and Social Development of the Russian Federation (GBOU VPO RyazSMU Ministry of Health and Social Development of Russia)
- The use of adhesive balm "Asepta®" in the treatment of inflammatory periodontal diseases L.Yu. OREKHOVA, Dr. med. Sciences, Professor, Head of Department V.V. Thermal Power Plant, Dr. med. Sciences, Professor, Head of Department S.B. ULITOVSKY, Dr. med. Sciences, Professor A.A. LEONTIEV, dentist A.A. DOMORAD, O.M. YAKOVLEV SPbSMU named after. acad. I.P. Pavlova, St. Petersburg - *Department of Therapeutic Dentistry, Department of Microbiology
- The use of new anti-inflammatory drugs in the complex of therapeutic and preventive measures for periodontal diseases (E.D. Kuchumova, A.A. Leontyev, O.V. Kalinina, L.Yu. Orekhova, S.B. Ulitovsky) E.D. Kuchumova, Ph.D., Associate Professor, A.A. Leontyev, dentist, O.V. Kalinina, dentist, L.Yu. Orekhova, Doctor of Medical Sciences, Professor, Head of Department, S.B. Ulitovsky, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I.P. Pavlova
- Evaluation of the effectiveness of treatment of chronic generalized periodontitis of mild and moderate severity using Asepta antibacterial agents (S.I. Gazhva, A.I. Voronina) S.I. Gazhva, Doctor of Medical Sciences, Prof., Head of Department A.I. Voronina, PhD, dentist. Department of Dentistry FKPV GOU VPO "Nizhny Novgorod State Medical Academy"
How to treat a pimple on the gum?
If a white pimple appears on your gum, make an appointment with a specialist. Abscess, gumboil and purulent cyst are eliminated only with the intervention of a dental surgeon. The operation is carried out in 4 stages:
- Pain relief using local anesthesia.
- Removal of a tooth. It is carried out when the tooth is the source of infection. This stage is not always necessary.
- Opening inflammation and clearing pus.
- Treatment of the cavity with an antiseptic composition.
Sometimes, to completely remove purulent masses, opening the periosteum is required. After surgery, the patient must undergo a course of medication. The doctor prescribes antihistamines and antibiotics. Severe inflammatory processes are accompanied by a general weakening of the immune system. Additionally, you may need to take immunostimulants for recovery.
Folk remedies
The use of traditional methods in the treatment of acne in the mouth is not only acceptable, but also desirable. Most often - rinsing the mouth with decoctions and infusions of medicinal herbs: chamomile, sage, pine needles, bay leaf. Procedures should be carried out regularly after each meal or brushing your teeth. Use only warm liquid for rinsing. To enhance the effect, herbs can be alternated.
Chamomile infusion is great for rinsing
Important! Under no circumstances should you apply a hot compress to the sore spot or rinse your mouth with a hot solution unless prescribed by a doctor! Often patients, not having the time (or desire) to visit the dentist, try to warm up the pimple, stimulating its “ripening and opening.” Such self-medication is fraught with serious complications, including blood poisoning and death.
Another simple and effective remedy is a solution of soda and/or sea salt (you can also use table salt). This rinse quickly eliminates tissue swelling, helps reduce inflammation, and has a drying effect. The method is used as an additional method to the main purposes.
Remember that even folk remedies should not be used as independent treatment protocols. It is necessary to visit a doctor to make a correct diagnosis and prescribe treatment. Herbal medicinal therapy should also be determined by the dentist.
What does a fistula on the gum look like?
Fistulas are small holes. Initially, white bubbles appear on the gums. Inside the seals, pus collects and harmful microorganisms multiply. Holes or canals appear when the soft jaw tissue remains in an inflamed state for a long time.
Before the perforating channels appear, the fistula looks like a red lump. A white dot is clearly visible on the side or above it - this is a purulent accumulation.
The fistula can reach 1 centimeter in diameter. Most often it occurs next to a diseased tooth, which ultimately requires removal. In fact, a fistula is a symptom that indicates other diseases in the oral cavity. Before it forms, the gums may become red and swollen, and sometimes the formation process is accompanied by painful sensations. Chewing becomes especially uncomfortable. Fistulas appear with advanced caries, pulpitis and periodontitis.
Types of dental abscess
- Osteomyelitis
- Phlegmon
- Tooth loss
Osteomyelitis
When pus remains in the soft tissues, complications arise. Dense formations with pus form in the bone tissues, and swelling of the lymph nodes also occurs.
Phlegmon
A life-threatening complication occurs when the infection spreads into the soft tissues of the gums. The growth of pus leads to chronic pathologies.
Tooth loss
If the infected fluid spreads to the base of the tooth, painful swelling appears, which may lead to tooth extraction.
What is that white ball on the gum?
Pimples on the gums, bumps and holes occur for various reasons. The symptoms accompanying the formation are also different. Among the common causes:
- Poor oral hygiene. Even people who brush their teeth twice a day can face the problem. The reason often lies in improper cleaning.
- Unbalanced diet leading to a lack of vitamins in the body.
- Bad habits. Smoking and alcohol are common provocateurs of diseases that occur in the oral cavity.
- Diseases and long-term use of medications (especially antibiotics), which lead to a general weakening of the immune system.
- An allergic reaction to products used for oral hygiene or to food.
- Diseases of the gums or teeth - advanced caries, periodontitis, periodontitis, osteomyelitis or other pathologies.
- Viral infection of the body. Among the most common viral diseases is herpes. Because of it, many small pimples with a white coating appear in the mouth. Most often, a scattering of pimples collects in one place.
Long-term inflammation can lead to deterioration in the fixation of the tooth - it becomes loose and there is a risk of falling out. The inflammatory process is a threat to bone tissue. Chronic acute course can even cause jaw deformation. To avoid such consequences, you can make an appointment with us. Doctor Fedorov’s clinic will help you cope with the most difficult cases.
Types of dental abscess
- Desnevoy
- Periodontal
- Periapical
- Pericoronal
- Combined (periodontal-endodontic)
Desnevoy
A superficial formation on the soft tissues in the area of the gingival papillae between the teeth. Inflammation is associated with the ingress of food, foreign objects, or trauma to the gums with a toothbrush or floss. A gum abscess is relatively easy to correct, but if not treated early, complications can arise.
Periodontal
This is an internal inflammation of the soft tissues of the gums, often caused by periodontitis. In this case, the infection is localized between the outer wall of the alveolar ridge and the gum when the dental pulp is healthy. A purulent exudate forms in the affected gum, which forms a lump in the periodontal pocket. There is no place in the gum for fluid with infection to escape, so the soft and bone tissues near the site of suppuration are gradually affected.
Periapical
The most common type of abscess, the cause of which is complicated caries or untreated periodontitis. The infection affects the root system of the tooth, resulting in pus accumulating at the apex of the root. When the immune defense is weakened, the inflammatory process affects the periosteum of the tooth, spreads to the soft tissue of the mucosa and leads to the formation of a fistulous tract and a purulent lump on the gum.
Pericoronal
Inflammation occurs in the soft tissues above the erupting tooth when food debris and bacteria get there. Pericoronitis can cause swelling of the neck, jaw, and also lead to angina pectoris (impaired respiratory function).
Combined (periodontal-endodontic)
Damage to the gums in the pulp and soft tissues, which causes periodontitis on adjacent teeth.
Consultation, image and treatment plan free of charge
Enter your phone number, we will call you back and select a convenient appointment time for you. Or call us yourself - +7
Already received your application
We will definitely contact you as soon as possible and advise you on all your questions.
No time to wait? Call:
+7
Preventive measures
To prevent a pimple from appearing on your gums, you need to adhere to the following preventive recommendations:
- regularly and properly care for your teeth using individually selected products,
- visit the dentist for a medical examination, to prevent the presence of caries and other pathologies,
- Consult a doctor in a timely manner if any problems with teeth, gums,
- increase immunity,
- provide a balanced diet.
And finally, I would like to note that the recovery process also depends on the person’s daily routine and mood. Adequate sleep, good nutrition, walks in the air, optimism are a guarantee of a quick cure and prevention of complications.
Herpetic stomatitis
The herpes virus can provoke the development of stomatitis. During the first infection, the disease manifests itself in an acute form. Without adequate treatment, it quickly becomes chronic.
Most often, children become infected before the age of three, due to decreased immunity. The virus can enter the body in different ways. For example, through the skin and mucous membranes or by airborne droplets.
The onset of the disease is accompanied by intoxication, vomiting and nausea. After two days, pimples appear on the oral mucosa. After they burst, ulcers form on the gums, inside the cheeks and lips.
In adults, the disease is usually more severe than in children. This is facilitated by various oral diseases and smoking. Regardless of the age of the patient, antiviral therapy and local anesthesia are prescribed.
Lidochlor gel or Lidocaine Asept spray are often prescribed as an anesthetic. To combat the virus, Acyclovir, Zovikarx and oxolinic ointment are used.
Rinse
They are used as an additional treatment in order to completely remove pus and ichor from an opened abscess and prevent the infection from spreading to healthy areas. Soda-salt baths and rinsing with antiseptic solutions help make treatment more effective and speed up gum healing. When rinsing, you must adhere to the following rules:
- During the day, do 4-5 gentle rinses or baths. To do this, just take the solution into your mouth and hold it for about 30 seconds.
- During the day, do 4-5 gentle rinses or baths. To do this, just take the solution into your mouth and hold it for about 30 seconds.
Physiotherapy
Physiotherapeutic methods are used as additional ones. They allow you to quickly cope with the infection and stop the inflammatory process. The following methods can achieve good results:
- Fluctuarization. The inflamed tissues are exposed to low voltage current.
- Electrophoresis with lidase. Electrical current is applied to the tissue, allowing the drug to be effectively distributed.
- Ultrahigh frequency therapy. The method is based on the influence of an electromagnetic field.
- Ultrasound therapy. The effect of ultrasound on infected tissues accelerates their regeneration.
- Laser therapy. Damaged tooth tissue is treated with a laser beam.
Traumatic or bacterial stomatitis
Damage to the mucous membrane can cause stomatitis in adults. In healthy people, injuries disappear without a trace and quickly. But if immunity is reduced and the wound gets infected, bacterial stomatitis may develop. Pustules, erosions, wounds and ulcers may appear on the gums or mucous membranes of the cheeks.
Bacterial or traumatic stomatitis occurs when soft tissues are often injured in the same place. This situation is not uncommon among those children and adults who wear braces. Prolonged friction of the lock against the mucous membrane will sooner or later provoke the development of traumatic stomatitis. The only effective preventive measure in this case is the use of special wax.
Other common causes of stomatitis include:
- frequent injury to the tongue by seeds;
- biting the inside of the cheeks or lips;
- the habit of holding various objects in the mouth, such as pencils or paper clips;
- permanent injury to the cheek from a splintered tooth, filling or incorrectly installed prosthesis.
To treat this type of stomatitis, it is first necessary to get rid of the cause that injures the mucous membrane. Wounds and ulcers can be treated with bluing or peroxide. In order for damaged mucous membranes to heal faster, it is recommended to lubricate them with rosehip or sea buckthorn oil.