Let's consider common questions that arise in patients with acute gum disease:
- How to treat an abscess on the gum in Samara
- What to do if pus appears on the gum
Moreover, precisely in this formulation. The definition of “abscess” in this case can include many different diseases, with different causes, mechanisms of development, different methods of prevention and treatment. The most common options will be discussed in this material.
What diagnoses can fall into the category of “abscess on the gums”?
- Exacerbation of chronic periodontitis;
- Exacerbation of chronic gingivitis (periodontitis).
Suppuration also occurs after tooth extraction (alveolitis), with cancer, with fractures (osteomyelitis) - these conditions are also accompanied by the release of pus, but here the patient (in most cases) knows about the cause (a tooth was recently removed, there was a fracture, etc.). d.). Sometimes manifestations of diseases of the mucous membranes are confused with ulcers - aphthous stomatitis, herpetic stomatitis and others, which also appear as a white (white-yellow/gray) area of the mucous membrane with a red rim around, but as such there is no pus there, and the causes of these conditions are also different. Therefore, we will talk more about periodontitis and periodontitis.
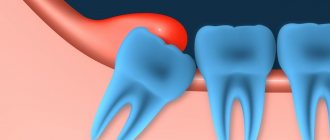
Exacerbation of periodontitis
Cause and mechanism of development
Periodontitis is an inflammatory disease associated with infection in the bone at the apex of the tooth root. Infection can enter the bone in different ways: through a tooth root canal or through a periodontal pocket.
- In the first case, the development of the disease begins with caries. If caries is not cured in time, the infection spreads deep into the tooth and causes pulpitis, and if further untreated, microorganisms spread deeper along the neurovascular bundle inside the tooth and reaches the bone.
- In the second case, the cause of infection in the bone is a problem in the interdental space (deep pocket). Inflammation of the gums can begin due to the accumulation of tartar, due to chronic injury from the sharp edge of a crown or filling, due to improper position of the tooth in the arch, and for many other reasons. Gradually, inflammation from the gums spreads to the circular ligament of the tooth, the ligament is destroyed, allowing microbes access to the space between the tooth root and the alveolar bone.
In both cases, the entry of microbes into the bone is accompanied by the release of a large amount of toxins, the bone begins to deteriorate, and in its place a cavity filled with pus forms. The process can go relatively unnoticed, causing inconvenience to the patient only during periods of exacerbation against the background of acute respiratory infections or other conditions accompanied by a general decrease in immunity.
Gradually accumulating, the pus continues to dissolve the bone, causing the inflammation to become larger. At the moment when the amount of pus reaches a critical level (or, due to a decrease in immunity, it becomes more), the pus begins to look for a way out. The bone gradually dissolves, passages are formed through which pus comes out under the periosteum and at some point a breakthrough occurs. Through this fistula, the pus comes out, and the original process returns to its chronic course.
Symptoms
Outside of periods of exacerbation, manifestations of periodontitis are minimal. This may be discomfort when biting on a tooth, or when pressing on the gum in the area of the causative tooth, but there are no other manifestations.
During the period of exacerbation, the following symptoms occur:
- acute pain when biting on a tooth (before an abscess appears on the gum), and after the fistula opens and the pus flows out, the pain goes away;
- the feeling of a grown tooth (also goes away after opening the fistula);
- pain and swelling of the gums in the area of the causative tooth;
- A whitish bubble appears on the gum, filled with liquid contents, when opened, pus flows out.
Symptoms of general intoxication may occur: fever, general weakness, lethargy, headache.
Diagnosis and treatment
To make an accurate diagnosis, they collect anamnesis, examine the oral cavity and the possible causative tooth, and be sure to take an x-ray.
The x-ray will show dark areas in the bone that are located in the area of the tooth root. The size of these lesions can vary from a few millimeters to a centimeter in diameter or more. Most often, an x-ray can tell you exactly where the source of infection is located, on which root (or between the roots of the teeth). The image determines the condition of the bone, the condition of the causative tooth and a possible prognosis for the future life of the tooth. Based on these data, a decision is made on the treatment method.
Possible treatment options for periodontitis in the acute stage
- Therapeutic treatment. This method involves removing nerve remnants from the canals (or unsealing them if the tooth has previously been treated), antiseptic treatment of the root canals, introducing medicinal drugs into the canal, and after some time (from a week to several months) the canals in the tooth are permanently sealed . It is assumed that with this treatment the source of infection will be removed (more than 90% of microorganisms responsible for the development of periodontitis live not in the bone itself, but in the root canal system, so high-quality canal treatment often leads to complete victory over the infection and restoration of the bone). After time (six months to a year), the bone is completely restored, and the gums heal with the formation of an invisible scar. To speed up the healing of the fistula tract, it is sometimes washed with a weak antiseptic solution or cleaned with ultrasound.
- Surgical treatment with tooth preservation. There are several options for this operation. If the inflammation is at the apex of the root, then the apex of the root is removed (the operation is called “resection of the apex of the tooth root”) and the cavity in the bone is cleaned. This method assumes that the canals are well sealed, at least 2/3 of their length. The second option is to remove half the tooth (hemisection operation). This type of operation is performed on multi-rooted teeth if inflammation is observed on one root, and the second root does not have such problems. The third option (when there is inflammation between the roots in a multi-rooted tooth) - the tooth is left unchanged, and only the bone between the roots of the tooth is cleaned. All these methods assume that the inflammation came from the tooth, and not through the periodontal pocket (since if the infection came through the pocket, then after the intervention the cavity will soon be populated with microbes again, and the inflammation will progress further). For each of these operations there are certain conditions, the observance of which is mandatory for a favorable prognosis. Thus, resection is carried out only if the canal is well sealed, at least 2/3 of the length, hemisection also implies that the root that remains in the bone will be well treated, and cleaning between the roots is carried out only if all canals are well sealed.
- A combination of therapeutic and surgical treatment. If the tooth has not been previously treated (or has been treated, but the canals are poorly sealed), then before undergoing any of the above operations, the tooth must be prepared. Therefore, the canals are treated first, and only then surgical intervention is performed.
- Removal of a tooth. If the focus of destruction in the bone is large (for each patient and for different teeth the concept of “large” will also be different), if the infection came through the periodontal pocket, if the tooth is not valuable for further prosthetics, the canals in it are impassable, there are cracks and there are other - conditions due to which the tooth cannot (or is impractical) to be saved, such a tooth is removed. You need to understand that sometimes doctors leave something that, by and large, would need to be removed, and sometimes, on the contrary, they remove a tooth that could still be fought for. As an example: they leave mobile teeth in elderly people, since they are the only ones that hold a removable denture, or they remove a tooth with inflammation between the roots in a young patient in order to preserve bone volume for future implantation. In any doubtful case (when you can try to treat it, or you can immediately remove it), they focus on a further prosthetic plan. If implantation is planned, it is better to remove all questionable teeth, and if bridges or removable dentures are used, they try to fight for every tooth.
You can read more about treatment and operations in the article about jaw cysts.
Gingivitis and periodontitis
Cause
Gingivitis is an inflammation of the gums, and periodontitis is a more severe form of the disease when not only the gums, but also the jaw bone are involved in the inflammatory process. Both diseases are often chronic and do not cause the patient much discomfort, but during periods of exacerbation more severe symptoms appear and the patient consults a doctor.
There are many causes of gum inflammation:
- hard and soft dental deposits;
- sharp edges of crowns and fillings, which constantly injure the mucous membrane;
- improperly restored contact points between teeth (due to which food accumulates in the gap, puts pressure on the gums and is an excellent place for microorganisms to settle);
- malocclusion (crowding of teeth, incorrect position in the arch);
- general diseases (diabetes, vascular problems, infectious diseases and others) can cause gum inflammation;
- changes in hormonal levels (during pregnancy, for example).
These are not all possible causes of gum disease, but most patient visits have one (or several) of these factors predisposing to inflammation in the gums.
Constant trauma (from food, the edge of a crown, tartar), microbial toxins, and impaired blood flow in the gums lead to the development of an inflammatory process. Usually, pus as such is not visible, but during periods of exacerbation, noticeable suppuration often occurs from periodontal pockets or its accumulation in the thickness of the mucosa (this formation is called a periodontal abscess).
Symptoms of gingivitis (periodontitis) in the acute stage
Patients with this diagnosis complain of:
- pain in the gums near a group of teeth;
- redness of the gums, swelling, pain when touched;
- it hurts to brush your teeth and eat;
- pus (sometimes with bloody veins) is released from the periodontal pocket or from the fistula tract (a fistula can form if the pockets are very deep);
- with gingivitis, the teeth usually do not suffer, but with periodontitis, tooth mobility, exposure of roots, pain from cold and sweet foods may be observed (since the root is more sensitive to irritants than the crown part of the tooth);
- Sometimes there is a deterioration in general health: fever, weakness, headache.
Exacerbations most often occur against the background of a general decrease in immunity (with acute respiratory infections or other diseases). In addition, periodontitis is characterized by seasonality (in spring and autumn, exacerbations occur more often).
Diagnostics
How to distinguish periodontitis from periodontitis? Outwardly, both cases may look the same: swollen gums, redness, a fistulous tract from which pus is released. In both cases, it hurts to bite on the teeth. In addition, one disease does not exclude another (there are cases when a tooth is surrounded by inflamed bone on all sides and it is almost impossible to say with certainty what is primary: periodontitis or periodontitis).
An x-ray is required to make a correct diagnosis and choose treatment tactics. In the image with gingivitis, we will not see any changes at all, but with periodontitis, areas where there is no bone tissue will be visible, while the teeth will be either healthy or well treated.
Treatment
It must be said right away that gingivitis is a reversible process, and periodontitis cannot be completely cured in most cases (it can be stopped, put into remission, but growing back the height of the bone is very problematic, and in many cases it is completely impossible).
If in the case of periodontitis we were dealing with microbes inside the root canal, then here we also have a microbial infection, only it is localized in the gums and bone. Treatment should be aimed at combating the cause, so the following measures can be taken:
- mandatory professional hygiene – removal of soft and hard dental plaque, polishing the surface of teeth, removal of granulations from periodontal pockets;
- correction of fillings and orthopedic structures, creation of normal contact points between teeth;
- if there is mobility of the teeth, they need to be splinted (limit movement);
- active anti-inflammatory therapy (rinses, dressings, ointments with antimicrobial action, in severe cases - antibiotics);
- general therapy (at the doctor’s discretion and depending on the severity of the process, antihistamines, painkillers, immunostimulants, vitamins, etc. can be added).
Usually this is enough to stop suppuration and relieve the acute process. To prevent exacerbations in the future, it is imperative to maintain hygiene (remove tartar at least once every six months), restore the dentition (if some teeth are missing), correct the bite (if there are problems with this) and maintain general health (if the cause of periodontitis is some common diseases).
Treatment options
The mucous membrane is very sensitive, so smearing wounds on the gums with iodine and brilliant green is strictly prohibited to avoid getting burned.
Medicines
To treat wounds in the oral cavity, special ointments are used that have an antiseptic effect: Solcoseryl, Metrogyl Denta, Apident. These drugs contain components that eliminate pathogenic microflora.
If a scratch causes pain, special ointments are used to relieve pain and strengthen the gums.
In addition to gels, it is recommended to rinse with the following solutions:
- Chlorhexidine - to clean the wound and protect against germs.
- Miramistin - to prevent infection with fungi leading to stomatitis.
- Hexoral, which contains levomenthol and hexetidine, which have an antiseptic effect.
- Hydrogen peroxide, which cleanses the scratch from dirt and stops the spread of inflammation.
If a white scratch is discovered, indicating suppuration, you cannot do without the help of a dentist, since you will have to open the wound. The doctor will remove any accumulated fluid and treat the cut with antibiotics. If a child has damaged the gums, one of the following antiseptics intended for children will help:
- Cholisal - for children after one year, promotes rapid restoration of damaged tissues, relieves pain.
- Kamistad is an ointment consisting of natural chamomile oil, intended for healing scratches.
- Dentinox-N is used not only for teething, but also for suppuration, redness and burning of the gums.
- Kalgel is an antibiotic that cleanses the wound and stops suppuration.
- Glycerol - used to moisturize and soften the damaged area, as well as to prevent the appearance of scars.
It is recommended that every mother have these medications in her medicine cabinet in order to promptly lubricate the scratch and protect the child from infection. Any of these drugs are lubricated on the gums 2-3 times a day. In this case, it is necessary to observe how the baby tolerates the effect of the medicine, whether there is an allergic reaction.
ethnoscience
Having scratched the gum, you need to immediately begin treatment to prevent inflammation. To do this, you can use folk remedies based on medicinal herbs.
You can quickly and easily get rid of redness and burning using the following formulations:
- 1 tsp tincture of calendula diluted in 200 ml of water - used to rinse wounds, and also used as a compress;
- propolis lozenges for application to the inflamed area of the gum;
- decoction of chamomile and sage, for the preparation of which 1 tsp. dry herbs pour a glass of warm water. This natural antiseptic helps get rid of purulent contents.
In order for the treatment to give the fastest possible effect, you should limit the intake of solid foods, exclude hot seasonings and sour pickled foods from the diet.
By choosing the right oral hygiene products, you can reduce the risk of scratches on your gums. Quitting smoking and strengthening the immune system will help the body fight off any infection. In summer, it is advisable to include more vegetables and fruits in your diet, and take more walks in the fresh air. In winter, it is recommended to drink a vitamin complex to increase immunity.
How to treat an abscess on the gum with folk remedies?
In both cases, the cause of the development of the process is an infection that sits deep in the gum or bone. This means that we still won’t be able to influence it directly. Traditional methods (rinsing with herbs, applying propolis, etc.) usually bring their results: the fistula really goes away for a while. BUT! All these methods remove the effect, not the cause! Until the microbial contamination is removed, inflammation will progress. It won’t cause such discomfort, but it certainly won’t go away on its own.
Therefore, treatment should begin with a visit to the dentist to determine the cause. And only then, when you identify the cause and begin to fight it together with the doctor, you can also use traditional therapy, since rinsing with herbs really gives a good result after removing the stone, and, for example, sea buckthorn oil slightly speeds up the healing of wounds on the mucous membrane.
Causes of sores on the gums
Sores on the gums can appear as a result of:
- thermal or chemical burns,
- the gum near the tooth can be injured by a hard toothbrush, or scratched by rough hard food,
- dental procedures, chipped teeth, braces,
- the dangerous habit of holding sharp objects in the mouth, a match, a toothpick, a pencil, can cause injury,
- stomatitis,
- ulcerative gingivitis.
To strengthen gum tissue, it is necessary to use special medicinal pastes that prevent inflammatory processes and increase gum tone.