From this article you will learn:
- causes of gum inflammation,
- how gums are strengthened at the dentist,
- treatment regimens.
The article was written by a dentist with more than 19 years of experience.
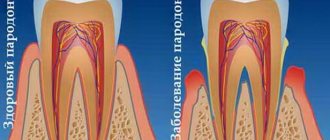
Complaints about weak, loose gums are typical for people with low-grade chronic inflammation of the gums (for example, chronic gingivitis or periodontitis). With a low severity of inflammation, such patients also experience bleeding gums and pain when brushing teeth, as well as swelling, redness or cyanosis of the gum margin.
In moderate to severe forms of inflammation, the above symptoms are gradually joined - periodic discharge of pus from under the gums, increasing mobility of the teeth, exposure of the necks and roots of the teeth. Patients notice that the gums seem to move away from the teeth (Fig. 4), which indicates the destruction of the dentogingival attachment and the formation of periodontal pockets.
What weak, inflamed gums look like: photo
Most often, loose, weak gums are characteristic of patients who have been trying to treat inflammation at home for a long time, using various rinses, gum gels or anti-inflammatory toothpastes. Their independent incorrect use always leads to only a temporary improvement, while the inflammation does not completely disappear, and the condition of the gums continues to slowly deteriorate. In this article we will tell you why this happens and what to do about it.
Weak and loose gums: causes
To understand how to strengthen your gums at home, it is important to understand the causes of gum inflammation. If you look carefully at the photos of patients with gingivitis and periodontitis (Fig. 1-6), you will see that in absolutely all photographs in the area of the necks of the teeth or in the interdental spaces you can see accumulations of soft microbial plaque and/or deposits of hard tartar . And this is no coincidence. Inflammation in the gums does not occur on its own - it occurs solely due to the impact of pathogenic bacteria on the gums by microbial plaque and tartar.
Bacteria release various toxins and pathogens, which trigger an inflammatory reaction in the gums. And when you start using various mouth rinses, gum ointments or pastes for bleeding without removing plaque, all this does not in any way affect the cause of inflammation (plaque and tartar), but only allows you to muffle its symptoms. Due to strong active components, swelling and redness of the gums and bleeding are temporarily reduced. At the same time, pathogenic bacteria remaining on the teeth will continue to produce toxins, slowly and less noticeably continuing to destroy the gums.
Important: any antiseptic or anti-inflammatory agents for gums, used without first removing dental plaque, lead only to a temporary reduction in the symptoms of inflammation, but most importantly, to the transition of inflammation into a chronic form and unnoticed progression of the disease.
It is logical that the appearance of dental plaque is associated with insufficient/irregular oral hygiene. But when you start talking about this with patients, almost no one wants not only to admit this fact, but also to change their behavior pattern (dental care). Good oral hygiene includes more than just brushing your teeth after every meal, i.e. 3 times a day, but also be sure to use dental floss to clean the interdental spaces. Therefore, it is very important, among other things, to avoid snacking between meals.
Over the many years of working as a periodontist, I have seen thousands of patients who were willing to spend a lot of time preparing various tinctures, gum massage, all kinds of rinses and applications. But when it came to brushing their teeth, they were not able to spend 5 minutes 3 times a day to properly brush their teeth, first with floss, and then with a toothbrush and toothpaste. Although, it is this, and not various medications, that is the key to healthy teeth and gums.
Yes, and one more important point - looking in the mirror at their inflamed gums, some patients may not see the accumulation of plaque and tartar. How so? - you ask. Not only did they tell me that stones on the teeth are formed not from hard water, but from poor hygiene... there are also no stones on the teeth, but there is inflammation in the gums. What's the matter, doctor? I believed you so much... and then comes a crying emoticon. But the whole point is that hard dental deposits can be not only supragingival, but also subgingival.
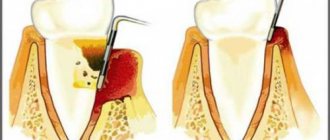
In patients with chronic periodontitis, hard dental deposits (tartar) most often form in periodontal pockets, and look like microbial plaques of different sizes, firmly attached to the surface of the tooth root. Such subgingival dental plaque causes even more damage to the gums than supragingival plaque. At the same time, finding and removing them, due to the lack of visual control, is much more difficult and requires a certain skill and perseverance.
In the photo below you can see how teeth with periodontitis that appear to have completely normal gums can actually have a deep periodontal pocket with a large amount of destroyed bone tissue (the second photo was taken after gum detachment). And this destruction was caused by the very subgingival tartar that we indicated with the arrow.
This bone destruction caused by subgingival dental plaque proceeds unnoticed until a certain point - until the amount of bone destruction becomes so large that tooth mobility occurs. In general, after this, all treatment comes down to the fight for survival and an attempt to delay tooth extraction. Therefore, you need to go to the dentist and remove deposits - not when it gets really bad, but much earlier.
How is gingivoplasty performed?
The operation does not require hospitalization or general anesthesia. The procedure can be performed as an outpatient visit to a doctor and under local anesthesia. With the help of effective modern anesthetics, gum grafting is performed completely painlessly.
If it is difficult for the patient to attend his own operation, then various options for premedication and sedation are provided for this.
In most cases, if it is necessary to fill the gum volume, the use of a donor flap is required. Often this is a fragment of the patient’s own mucosa from the tubercle of the upper jaw, palate or the area behind the lower teeth (retromolar). The area from which donor material is collected is dictated by the type of manipulation and the volume of tissue required.
In case of insufficient number of donor tissues, artificial materials are used. Plastic surgery of the lower gum is considered easier, but in reality, healing of the mucous membrane after surgery in any case occurs rapidly - in the oral cavity, tissue regeneration occurs very quickly.
Types of gingivoplasty
Depending on the diagnosis and health status of the patient, the surgical tactics may vary.
- When it is necessary to increase the gum or fill its defect - gingivoplasty
First, the site where the donor site will be placed is prepared, and then a free connective tissue graft is collected. After suturing the donor flap with the recipient area, the intervention is considered complete.
Sometimes the graft is placed in the implant area into a pocket or tunnel formed in the recipient area. To do this, the donor fragment is first de-epithelialized.
There are other methods, their choice is dictated by indications and capabilities.
- In case of incomplete tooth eruption - gingivotomy
An incision is made in the gum in the area of the tooth crown. The size of the excised area depends on the position and size of the tooth.
- If there is excess mucosal tissue – gingivectomy
If there is a periodontal pocket or various types of hypertrophy, the surgeon excises excess mucosa and tightly suturing the edges of the wound so that the mucosa is at the desired height and tightly covers the necks of the teeth.
Operation duration
The intervention can last 1-3 hours, depending on the volume and degree of complexity. The most complex situations are treated in several stages. For example, in order for the patient to undergo gum surgery more comfortably, it is recommended to operate on each side (left, right) in turn - then he will be able to chew food and sleep on at least one side.
Rehabilitation after gum surgery
Due to the high speed of regenerative processes in the oral cavity, gum healing after plastic surgery occurs in just 1-2 days. It is during this period that it is important to follow the rules of rehabilitation and the doctor’s recommendations to accelerate the epithelization of the wound, so that pain after gum surgery does not bother you too much:
- Avoid solid and irritating foods - sour, salty, spicy, cold;
- Stop smoking, alcohol, active sports, and shaking in transport;
- Carry out hygienic care very carefully (don’t even rinse too vigorously);
- Do not make suction movements, do not touch the wound with your tongue or any objects;
- Try to eat alkaline foods, as acidification of the pH of saliva promotes inflammatory processes.
How long it takes for the gums to heal completely after plastic surgery, that is, with complete restoration of blood supply, innervation and molecular connections, depends on the individual characteristics of the patient’s body. Sometimes final rehabilitation can take up to 3 months.
Swelling after gum surgery goes away within a few days (up to a week). At this time, slight tooth mobility and hypersensitivity are allowed. Some clinics provide the patient with a special mouthguard with a disinfecting effect, which accelerates wound healing.
What effect can be expected after gingivoplasty?
In addition to correcting aesthetics, the goal of surgical intervention is to prevent the development of many complications - tooth loss, deepening of periodontal pockets, the formation of wedge-shaped defects, hypersensitivity of the necks and roots of teeth.
Thanks to gingivoplasty, hygiene is facilitated, bleeding gums, bad breath, inflammation are eliminated, and tartar forms more slowly. Also, after plastic surgery, the possibilities for prosthetics and implantation expand - the patient has fewer contraindications for any dental procedures and manipulations.
Perioplasty - plastic surgery of the gums around implants - improves blood circulation in the implantation area, hygiene, and extends the life of artificial roots.
Complications after gum surgery
The operation can have complications during the rehabilitation period only if:
- Incorrect history taking - the doctor did not find out (or the patient was able to hide) the patient’s health problems, the presence of factors that complicate wound healing (for example, with immune problems);
- Non-compliance with the doctor’s recommendation - if the patient has neglected the rules of gentle care, does not follow the instructions for anti-inflammatory therapy, disinfection, lifestyle and others;
- Medical error - in case of infection in the wound, leaving a foreign body (bandage thread, bone fragment).
On the last point, gum plastic surgery is the least likely to have complications, because modern operating algorithms and antiseptics, sterile packaged instruments and suture material, disposable consumables - all this leaves practically no chance for infection.
It is much more important to take seriously the rules of the postoperative period, not to smoke, to make a proper menu and to care for the wound surface as necessary.
Strengthening gums: the right approach
Strengthening gums and teeth during gingivitis and periodontitis is possible in 2 options. Firstly, it is undergoing a professional course of treatment at the dentist, which primarily includes ultrasonic cleaning of teeth from stone and plaque. Plus a course of anti-inflammatory therapy, consisting of antiseptic rinses and special gels for the gums, which (with the exception of severe cases of periodontitis) can be easily carried out at home.
The second option concerns strengthening the gums in between courses of professional gum treatment at the dentist. If during the period of professional treatment (after removing dental plaque) products containing antiseptics and antibiotics are used, then for long-term maintenance therapy anti-inflammatory drugs are used, which will not cause harm with constant long-term use. We hope that it has become clear to you: the correct approach to gum treatment includes both professional treatment at the dentist and supportive treatment at home.
1) Removal of tartar and plaque –
How important it is to professionally clean your teeth to remove plaque and tartar, and how the condition of your gums changes just a few days after high-quality removal of dental plaque – you can see in Figure 9-10. But we once again draw your attention to the fact that in case of periodontitis, it is best to remove dental plaque not from a dentist or hygienist, but from a periodontist.
→ Video of ultrasonic teeth cleaning procedure
2) Anti-inflammatory therapy –
After removing dental plaque, the doctor will prescribe you anti-inflammatory therapy, which you can do at home. Only in cases of severe periodontitis and deep periodontal pockets (in parallel with home therapy), the doctor usually schedules an appointment once a day (for 10 days) to rinse the periodontal pockets with antiseptics. The course of treatment usually lasts 6-7 days for gingivitis, and 10 days for periodontitis.
Home therapy consists of antiseptic rinses and applications of anti-inflammatory gel to the gums. Gum treatment is carried out 2 times a day. The following drugs are usually used in the complex: Chlorhexidine solution for rinsing (its concentration can be from 0.05 to 0.25%, which will depend on the severity of inflammation), and CholisalGel for applications. How to properly treat gums with these drugs is described in detail by us in the article at the link below:
→ Treatment of gum diseases
Important : if you decide to start drug treatment, ignoring the need to remove dental plaque, then remember that behind the visible temporary decrease in the symptoms of inflammation from such treatment, you will receive a subtle, increasing destruction of the attachment of the tooth to the gum and bone tissue. Over time, it will lead to tooth mobility, their removal, and the need for expensive treatment methods (for example, splinting teeth with fiberglass or curettage of gum pockets).
Nutrition and vitamins
In order for your gums to always remain healthy, you need to eat a healthy, high-quality and varied diet. The daily diet should contain a sufficient amount of fresh vegetables and fruits, natural meat, as well as fiber and minerals.
Products that are most beneficial for gums:
- Citrus fruits . Rich in vitamin C, which actively strengthens the mucous membranes of the mouth and eliminates vascular fragility.
- Greens and dairy products . They are a source of vitamin K, which reduces tissue bleeding and increases the tone of the vascular wall in the gums.
- Fish and other seafood . They contain large amounts of phosphorus, which has a strengthening effect against periodontal disease.
- Garlic and onion . They contain zinc, a powerful antioxidant and anti-inflammatory mineral.
- Nuts . The ubiquinone contained in them prevents the deposition of tartar and the development of inflammation.
- Cheese . The main source of calcium is a mineral that strengthens teeth and gums.
- Red wine . Contains a large amount of antioxidants and tannins, which have a healing effect and prevent the occurrence of the inflammatory process.
During pregnancy, many women experience problems with teeth and gums. This is explained by the fact that a growing child takes a large amount of vitamins, calcium and other minerals from the mother. This is why taking vitamins is important during pregnancy. Popular multivitamin complexes are:
- Elevit
- Vitrum-prenatal
- AlfaVit Mom
- Sana-Sol Pregna
They contain the optimal amount of essential vitamins and minerals. These medications should be taken once a day after meals.
Strengthening gums at home: drugs, methods
As we said above, the best way to strengthen gums is proper and regular oral hygiene. However, there are a number of remedies that can further help you - improve the condition of your gums. Such products should not contain antiseptics and antibiotics, because the latter should be used only in short and infrequent courses (24stoma.ru).
High-quality oral hygiene –
In short... Teeth should be brushed after every meal, including lunch. To brush your teeth, you must first use dental floss, without which nothing will ever allow you to clean the interdental spaces from rotting food debris (toothpicks and mouth rinse are ineffective for this). At lunchtime, good hygiene involves a combination of dental floss + chewing gum. But if you no longer have gingivitis, but periodontitis, we advise you to have a second set of toothbrush and toothpaste at work.
You need to brush your teeth not 15 minutes after eating, but within the first 5 minutes. If you are visiting, at a restaurant, or outdoors, you should always have dental floss and a pack of chewing gum in your purse/pocket. It is very important to avoid snacks between main meals - no cookies, chocolate buns, etc. (apples that are not too soft are fine). If you eat candy, you need to brush your teeth. These are the simplest basic rules, the implementation of which is much simpler than the expensive and lifelong treatment of chronic periodontitis.
How to use dental floss and brush correctly -
Important: If you have crowns and bridges on your teeth, or if you have diagnosed periodontitis with deep periodontal pockets, be sure to use a home irrigator to rinse periodontal pockets and clean artificial crowns (in addition to basic hygiene methods). The cost of the irrigator will be 3-5 times cheaper than the cost of splinting mobile teeth, and also 10-20 times cheaper than the cost of open curettage of periodontal pockets.
Toothpastes for weak gums –
Such toothpastes can be divided into 2 groups. The first group of pastes contains potent antiseptics (usually chlorhexidine), and it is undesirable to use them for more than 2-3 weeks. It is optimal to use such pastes only as part of complex therapy during professional treatment of gingivitis/periodontitis at the dentist. Such pastes are good for relieving bleeding and swelling of the gums, and you can read more about them here .
But such pastes are not suitable for constant use, and their uncontrolled use can even cause harm (such pastes only suppress the symptoms of inflammation, making a person think that everything is fine). Therefore, to strengthen the gums, not antiseptics are used, but mild anti-inflammatory agents - extracts of medicinal plants, thymol, eugenol, clove oil, eucalyptol, bisabolol, allantoin, phenyl salicylate, as well as sodium fluoride.
a) Toothpaste “Parodontax-F” –
instructions for use- manufacturer - UK,
- active ingredients – extracts of echinacea, peppermint, sage, myrrh, chamomile, ratania, mineral salts, zinc citrate,
- fluoride content – 1400 ppm,
- price from 150 rubles (75 ml tube).
Comments: Parodontax toothpaste has a formulation that has remained unchanged since approximately 1890. This is a natural toothpaste that contains high concentrations of medicinal plant extracts and mineral salts, which have a pronounced anti-inflammatory and astringent effect, due to which gum bleeding is reduced. Unlike many others, these pastes can be used on an ongoing basis to treat and prevent gum inflammation (due to the fact that they do not contain antiseptics).
b) Toothpaste “Parodontocide” –
instructions for use- manufacturer – Russia,
- active ingredients – mint and sage extracts, thymol, eugenol, allantoin, phenyl salicylate, sodium fluoride,
- fluoride content – 1000 ppm,
- price from 120 rubles (50 ml tube).
There are other good anti-inflammatory toothpastes besides the ones listed above. You can independently evaluate the compositions of pastes, taking into account our recommendations for active ingredients made above. However, an important point is not only the names of the active ingredients, but their concentration in the paste. And in the above pastes there is a fairly high concentration of medicinal plant extracts, as well as other medicinal components.
Folk remedies and recipes
Traditional medicine has a large number of recipes that can strengthen the gums, even when the process has started and the teeth are already loose. In terms of their effectiveness, such methods are not inferior to traditional means, but are more accessible.
Herbs and medicinal plants
Decoctions and infusions for rinsing from medicinal plants have a quick and long-lasting effect, relieve bleeding and inflammation, and improve metabolic processes.
- Infuse 2 tablespoons of dried chamomile flowers in a thermos in 200 ml of hot water. Rinse your mouth with infusion after every meal. The course of treatment is 3 weeks with a break of 2-3 months. Chamomile has a strong anti-inflammatory and healing effect, increases the resistance of gums to adverse factors.
- Boil 3 tablespoons of crushed oak bark in 400 ml of water. Use the decoction to rinse the mouth three times a day. Oak bark has pronounced astringent properties, eliminates bleeding and restores damaged tissue.
- Infuse one tablespoon of sage and mint in a glass of boiling water for 20 minutes. Use the resulting infusion to rinse your mouth in the morning and evening. Herbs have a refreshing effect, increase blood flow in the gums, and strengthen them.
Sea salt
Strengthening gums with folk remedies is impossible without the use of sea salt. A rinse solution made from 200 ml warm water and a teaspoon of salt has a strong anti-inflammatory effect. Its constant use after meals prevents plaque deposition, bacterial growth and bleeding.
In the absence of natural sea salt, it can be replaced with the most common table salt.
Propolis
Propolis stimulates gum restoration, strengthens them, and has an anti-inflammatory and protective effect. Dilute a teaspoon of propolis tincture in a glass of boiled and cooled water. This solution should be used to irrigate the gums in the morning and evening. 3-4 courses of procedures should be carried out per year for 15-20 days.
Only regular visits to the dentist, as well as the use of products to strengthen the gums, can maintain oral health and avoid such serious diseases as periodontal disease or gingivitis.
Recession classification
Receding gums are classified according to their causes into the following types:
- Traumatic - appears as a result of mechanical damage to the mucous membranes. As a rule, the injury is associated with a hard toothbrush and improper brushing technique, which leads to systematic damage. Other common causes of injury include incorrectly installed orthopedic structures - veneers, crowns, etc. Sometimes injury is associated with protruding edges of fillings and elements of braces. It is important to understand that bite defects are also a common cause of recessions: improper distribution of chewing load leads to changes in tissues. Injuries can also be associated with direct pressure on the gums of the teeth. And finally, another group of injuries includes burns, for example, those associated with unsuccessful home bleaching.
- Symptomatic - in this case, the prolapse is associated with some pathological process and serves as its symptom. Usually we are talking about diseases of the gums and periodontal tissues: gingivitis, periodontitis or periodontal disease. They affect mucous membranes and soft tissues, disrupting their trophism. The situation is aggravated by dental deposits in the places where the gums adhere to the tooth; as a result, the tissue simply peels off from the surface of the tooth and the tissue level drops. More rare pathologies manifested by gum recession include other diseases, for example, diabetes mellitus, leukemia.
- Physiological - it develops as a result of a general metabolic disorder, including metabolic disorders in periodontal tissues. In this case, we are talking about the natural processes of aging. However, sometimes receding gums develop at a young age due to the individual structural characteristics of the dental system. The most striking example is a shortened labial frenulum, which leads to tissue tension.
Based on the severity of a recession, it is also classified into three categories:
- light: tissue loss up to 3 mm;
- average: 3−5 mm;
- heavy: more than 6 mm.
Based on the localization of the pathological process, recessions are divided into localized and generalized. In the first case, receding gums are associated with trauma and spread to one or more closely spaced teeth. As a rule, the outer side of the teeth is affected, and the defect is noticeable when smiling.
In the generalized form, the pathology covers the entire dentition on one or both sides. It is more often observed in elderly patients, as well as in people with periodontitis and periodontal disease.
Ask a Question
Symptoms of receding gums
The condition in which the gums recede may be accompanied by other symptoms. Depending on the extent of the pathological process, recession is observed in a limited area, one side or the entire jaw. As a result, the neck of the tooth may be exposed, and with severe loss, part of the root.
This cannot but be accompanied by increased sensitivity of the teeth - increased susceptibility to hot and cold, sour, sweet foods and even mechanical stress. This symptom leads to difficulties while eating.
It is important to understand that some symptoms may indicate concomitant pathologies. So, if recession is observed against the background of whitish, pale gums, we can talk about periodontal disease. Bleeding and red gums often develop with periodontitis and gingivitis.
What will happen if left untreated?
Lack of timely treatment for gum recession can be fraught with more than just aesthetic problems. If there is a gap between the gum and the tooth, food debris and plaque get into it, and this can cause an inflammatory process. As the tissues become thinner and sagging, the following consequences of recession may appear:
- Hyperesthesia, or increased tooth sensitivity, difficulty chewing.
- High risks of caries development, and in the least protected and more vulnerable areas - in the area of the exposed necks of the teeth. At the same time, carious lesions in this area proceed faster and are more quickly complicated by pulpitis and periodontitis due to a thinner layer of enamel.
- Increased risk of developing a non-carious lesion - a wedge-shaped defect.
- High risks of inflammation, swelling of the gums, and the formation of periodontal pockets.
- An increase in the amount of plaque at the roots, which further aggravates the condition.
Complications can result in serious consequences such as loosening and loss of teeth.
Diagnostic methods
If the gum is moving away from the tooth, it is important to see a doctor as soon as possible: in the early stages, recession is faster and easier to treat. Diagnosis involves collecting anamnesis, analysis of symptoms and complaints, examination and instrumental examination if necessary. During the examination, the doctor will assess the width and nature of the gum damage. A periodontal probe can be used for diagnosis - it is inserted into the periodontal pocket to assess the depth of the lesion.
An assessment of the degree of gum damage is calculated by calculating the recession index using the following formula: the number of affected teeth is divided by the total number of teeth and multiplied by 100%. This is how the severity of the disease is determined: less than 25% is a mild recession, 26-50% is moderate, and from 50% is severe.
For diagnostics, a microscope is used, and binocular magnifying glasses are used. The thoroughness of diagnostic measures allows you to accurately select an effective treatment method. In addition, before starting treatment, it is very important to find out the causes of the disease: to determine whether recession is an independent disease or a symptom of another pathology.
Therefore, differential diagnosis with other periodontal diseases in which the gums rise is necessary. To do this, the doctor may prescribe a targeted or panoramic X-ray to assess the condition of bone tissue and detect hidden concomitant diseases.