A number of dental procedures are impossible without laboratory diagnostic results.
Sometimes it is difficult to establish a diagnosis through examination of the patient by a dentist and using hardware diagnostic tools. In case of planned surgery, tests are also mandatory.
Laboratory diagnostics in dentistry can include both general clinical tests and complex morphological and biochemical screening.
This allows you to assess the work and condition of individual systems of the patient’s body, as well as predict the effectiveness of therapy, the approximate time of treatment and recovery.
At the first stage of making a diagnosis, the dentist examines and interviews the patient about problems with the dental system, listens to his complaints and the history of the development of the disease. In some cases, this is enough to make a diagnosis. But most often, the dentist refers the patient for an additional X-ray examination or orthopantomogram (second stage).
In 90% of cases, the data obtained is enough for a correct diagnosis and development of a treatment plan. In difficult cases, the doctor prescribes laboratory diagnostics, as well as hardware examination methods - MRI, CT, ultrasound. Popular diagnostic measures are general clinical blood and urine tests, as well as serological and microscopic examination.
Initial examination
Diagnosis of diseases in dentistry begins with a patient interview and visual examination. It is very important to tell your doctor the symptoms of the disease in detail. These may include: pain, discomfort when eating hot or cold food, sweet or sour taste. If you have allergies to any medications, hereditary or genetic diseases, be sure to tell your doctor. Smoking can also affect the condition of your teeth and gums.
The dentist will examine your mouth using a mirror and probe. For a detailed examination, all Dental Guru clinics have microscopes. If the problem and its solution are obvious, then if you agree, treatment can begin immediately. To clarify the diagnosis, the doctor will conduct the necessary functional diagnostics.
How do our dentists conduct a visual examination?
First, you will sit in the dental chair, and the doctor will examine your head and face: there are no changes in the color of the skin, the size of the lymph nodes, or swelling.
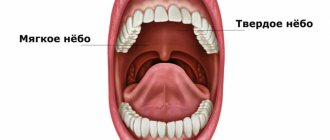
He will then ask you to tilt your head back and open your mouth as wide as possible. This is necessary to assess the condition of the upper and lower palate, tongue, inner cheeks and lips. No tools are required here, just a source of bright light. Even if you are concerned about a specific tooth, all teeth must be examined. After all, it often turns out that the problem lies in a completely different place. To do this, the doctor uses a dental mirror and a special probe.
- A small mirror allows you to carefully examine hard-to-reach areas and illuminate those places that the lamp rays do not reach. Carious cavities, tartar deposits, suppuration, chips, dental growth disorders - all pathologies appear in full view.
- Using a pointed probe (explorer), the dentist checks all suspicious crevices, depressions, cracks and darkened areas. If everything is in order, then the probe moves freely. If the enamel is damaged somewhere, then most likely there is a hidden carious cavity.
- The condition of the gums can be assessed with a periodontal probe. At its tip there is a millimeter scale and a small ball to reduce possible discomfort. With its help, the dentist receives information about the presence of inflammation, bleeding, the depth of periodontal pockets, etc.
A visual examination helps an experienced dentist immediately make a diagnosis in the following cases: caries, gingivitis, periodontitis, malocclusion. However, some diseases that occur latently, for example, periodontal disease and severe forms of caries, can only be detected using hardware diagnostics.
X-ray diagnostics in dentistry
A targeted photograph in dentistry is used if the problem is localized. In Dental Guru clinics, radiography is performed using modern digital innovative devices, where the dose of radioactive radiation is reduced to a minimum, and radiology in dentistry is absolutely safe. The radiologist will wear a special lead apron for your protection. The shooting sensor is located in the mouth or on the front side. The procedure is painless and takes a few seconds. The final image will show the doctor the condition of the diseased tooth and adjacent teeth.
Using an x-ray, you can see caries, bite defects, jaw fractures, areas of infection in the root canals, abscesses, tumors, cysts, incorrect placement of wisdom teeth and other pathologies. X-rays show hidden caries under a filling, crown or on the root.
Signs of caries on x-ray:
- The spot looks like an area with some darkening of reduced density.
- Medium and deep – reduced surface density due to enamel damage.
- Deep – deformation of the tooth structure with granulomas (areas of inflammation, proliferation of connective tissue) and hardening in the pulp
The importance of condylography in identifying dysfunction of the dentoalveolar system
Condylography is a method used to analyze the position of the temporomandibular joint. The main task of the manipulation is to establish the trajectory or, more simply put, the path of movement of the jaw. The technology significantly simplifies the diagnostic procedure and helps identify pathological processes.
Note! The information obtained as a result of condylography can be used not only when making a diagnosis, but also to implement the prosthetic procedure. Thus, the availability of data on the individual indicators of the patient’s TMJ movement trajectory allows the orthodontist to make the most suitable design.
Orthopantomogram, panoramic image
When you have some kind of local problem, of course, you can and should take a targeted photo. But since all the teeth and nerve endings in the mouth are connected, you may think that one tooth hurts, but the problem is actually somewhere nearby. That is why all professional doctors take a panoramic photograph of the teeth during the initial diagnosis in dentistry. And this “panorama” represents your entire dentition and allows you to see the existing problems in their entirety.
The panoramic image clearly shows both jaws, it is possible to draw conclusions about the condition of the teeth and roots, skeletal system and paranasal sinuses, and diagnose defects in bite, location and shape of teeth. Having received an orthopantomogram, the doctor will see caries at any stage, periodontal pockets, fibromas, granulomas and cysts, latent inflammation, possible changes in the condition of the temporomandibular joint, unerupted wisdom teeth, and sinusitis. A panoramic photograph is necessary before implantation, prosthetics, orthodontic treatment, surgery (complicated removal of wisdom teeth), complex treatment of periodontitis and periodontal disease.
Practical significance of the photo protocol
Creating a photo protocol is necessary for a more detailed assessment of the condition of the dental system. When diagnosing a disease, photography is an integral part of the procedure.
The manipulation is carried out in accordance with the protocol, so even the smallest details are subject to analysis and assessment by a specialist.
According to the object, the photo protocol can be extraoral and intraoral. An important nuance of the procedure is the position of the patient’s head; when creating a series of images, it must remain unchanged.
What information can be obtained as a result of creating an extraoral protocol:
- indicators of tension in the muscular system of the neck and head;
- data on the symmetry (asymmetry) of the dental system;
- information about the individual characteristics of the patient’s appearance.
The intraoral protocol allows:
- analyze the condition of the jaws;
- identify the presence of phenomena such as tooth abrasion or wedge-shaped defect;
- assess the position of the teeth.
The photologging technique is used to evaluate both intermediate and final results.
Computed tomography of teeth
But on an orthopantomogram, since it is a two-dimensional image, nuances are not always visible, and it is impossible to accurately determine the volume and height of bone tissue. Therefore, before implantation and in other cases, the doctor will do a CT scan. This examination is also absolutely safe. The final three-dimensional image of your jaws will show both the canals to the therapist and the volume of bone tissue to the implant surgeon. Based on computer diagnostics in dentistry, a doctor can prepare precise surgical templates for implantation and prosthetics.
Casts and models
To accurately reproduce the position of the jaws and display their movement as closely as possible, a technique for creating casts and models is used. The principle of operation of the technology is to make a plaster copy of the jaw using a special articulator device.
Simulation provides the doctor with the opportunity to obtain the most accurate information about the state of the dental system. Moreover, the procedure helps to determine the initial position of the lower jaw, which is important when analyzing the relationship of the two jaws and making a diagnosis in general.
Teleradiography of the skull
Diagnostic methods in dentistry include examination of the skull. Before orthodontic treatment, the doctor needs to see the angle of inclination of the teeth and the degree of their displacement. Using TRG, the doctor can examine in detail all parts of the skull from all sides by rotating the image. During teleradiography, the patient does not touch the device.
Teleradiography of the skull is performed in three projections: frontal, axial and lateral. Frontal projection is a basic photograph of the head, which shows the condition of the teeth, bones, jaws, symmetry or asymmetry, and inflammatory processes. The axial or chin projection helps the implantologist evaluate the structure of the nasal cavity, cheekbones, and sinuses of the upper jaw before implanting the upper teeth.
In Dental Guru clinics, the orthodontist performs teleradiography of the skull in a lateral projection to determine the bite, plan further strategies and tactics for correcting it. After the examination, diagnostic models will be made that will allow you to more accurately plan your treatment and even show the final result.
Diagnosis by palpation
The palpation method is often used in dental practice. During the procedure, the doctor feels the muscles of the head and neck, thus determining their general condition. Disturbances in the functioning of this muscle group indicate the development of pathological processes in the dental system.
What palpation reveals:
- development of disharmonic processes in the work of the muscular system;
- the reason for the violations.
As a result of bilateral palpation, the dentist receives valuable information, which, together with data from other diagnostic methods, allows us to clarify the picture and draw up an optimal treatment plan.
Diagnostic methods in modern dentistry
In our clinics, in addition to traditional ones, there are innovative diagnostic methods. For example, the MegaEye intraoral (intraoral) camera, which allows you to demonstrate problems in your oral cavity in real time. For example, plaque, superficial caries, poor fit of the crown, any postoperative complications. The examination result will be visible on the screen. To diagnose, you need to open your mouth, after which the doctor will move the camera along the dentition from below and above. If you're planning to travel, buy this compact camera. MegaEye connects to a smartphone or laptop via Wi-Fi, which allows the doctor to see the condition of your teeth and consult you remotely.
There are also chemical diagnostic methods, for example, caries detectors and hygiene level indicators. Our hygienist can measure the hygiene index for your child or spouse, who does not like to brush their teeth and constantly suffers from caries. The drug will color all problem areas and show how well and efficiently the teeth are cleaned.
In addition to all this, functional diagnostics in dentistry Dental Guru (Moscow) includes the MEGA ISQ device, which after implantation surgery allows you to most accurately measure the stability of the implant before prosthetics. We do not prepare the crown until we are sure that the installed implant has taken root and will withstand the load.
We also have a Medit i500 intraoral scanner in our clinics, which allows you to recreate the full 3D model of your jaws as accurately as possible. The device is intended for prosthetics, for the manufacture of crowns and inlays using the CAD/CAM system. The procedure for prosthetics using a three-dimensional scanner is as follows. For example, to prepare an inlay after caries treatment, the cavity is scanned and a 3D model is sent to the laboratory. In our own dental laboratory, the technician casts the inlay, the courier brings it to the clinic, and the prosthetist fixes it. The Dental Guru dental network offers treatment, prevention, and diagnostics.
Each Dental Guru clinic has a full range of x-ray diagnostics: a microscope, a computed tomograph with the function of taking pictures of the temporomandibular joint, a device for cephalometry, OPTG, a digital radiovisiograph for targeted imaging. Multifunctional devices Rayscan and Vatech are used, which can be used to perform all types of radiation diagnostics in dentistry.
What additional diagnostics can the dentist prescribe?
- Apex locator
With its help, the doctor can determine the length of the dental root canal as accurately as possible. Due to the complex anatomy, it is difficult to do this in other ways. Selecting the right tools is essential to effectively treating root infections.
- Biopsy
This procedure is carried out if a dental cyst or other neoplasm has been diagnosed. A biopsy is necessary to ensure that the suspicious object is benign. The dentist takes a sample of fluid or tissue using a biopsy needle and sends the finished sample to a laboratory for analysis.
The diagnostic methods used in our clinic are safe and do not cause any discomfort. Thanks to them, the doctor will be able to start treatment on time and keep your smile healthy and beautiful!
Infectious and inflammatory periodontal diseases can fully be called diseases of civilization, given that they are ranked sixth in the list of the most common human diseases. The constant effect of predisposing factors (social, systemic, iatrogenic, local conditions of the oral cavity, etc.) against the backdrop of environmental unfavorability extremely often leads to the development of periodontopathies in all age groups with an increase in the proportion of moderate and severe lesions in people over 35 years of age. According to the WHO report (WHO: Oral health. Fact sheet No. 318, April 2012), modern advances in understanding the etiology of pathogenesis, as well as in the treatment of these diseases, have not significantly changed the situation for the better.
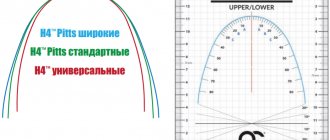
Infectious and inflammatory periodontal diseases are prone to a chronic progressive course, and the outcome of the pathological process depends on the timeliness of diagnosis and the early initiation of adequate therapeutic and rehabilitation measures. In one of the reviews by U. Carounanidy, R. Sathyanarayanan [14], devoted to the problem of diagnosing caries as a provoking factor of periodontal diseases, the authors commented on the “Caries Iceberg” diagram, proposed at one time by N. Pitts, C. Longbottom [38], which is quite clearly reflects the state of diagnosis of this pathological condition and the main problems associated with it at the present stage (Fig. 1).
Figure 1. “Caries iceberg” - diagnostic scheme, D1-D4 - diagnostic criteria [38].
It can be assumed that this diagram can be applied to the diagnosis of not only caries, but also any other dental pathology, while the authors describe the main stages in the development of the diagnostic process as follows:
1) development of strict diagnostic criteria based on easily detectable signs of the disease;
2) improving the technology of diagnostic methods aimed at reducing their diagnostic threshold when verifying the diagnosis at a qualitative level;
3) development of methods for quantitative assessment of pathological conditions to recognize “hidden” deviations that are not registered at the qualitative level;
4) transition from a logically constructed, nominal or ordinal scale for assessing the pathological process to a numerical scale that allows monitoring of the disease and prognosis of its course and outcomes [14].
The presented scheme clearly demonstrates that starting from the second stage, the dentist has an urgent need not to limit himself to clinical methods of examining the patient, but to resort to instrumental and laboratory diagnostics. Thus, if at the first stage the basis of diagnosis is the principle of clinical observation, then at the second stage a different level of data assessment is required, which requires the scientific development of a list of biological markers of the disease and the presence in the arsenal of laboratory diagnostics of methods for their registration. At the third stage, we are talking about the quantitative assessment of biomarkers by laboratory methods and the scientific development of associated signs of the disease - indicators, factors and determinants of the risk of developing the disease itself and its adverse outcomes. Finally, the fourth stage involves the creation of a diagnostic monitoring system with the identification of predictors of the disease, its biological markers, criteria for assessing its course, forecasting possible outcomes and the effectiveness of treatment measures.
From this point of view, the development of laboratory methods and the possibility of their use in the diagnosis of dental diseases requires not only their technical perfection, but also taking into account the characteristics of the pathogenesis of lesions of the oral cavity, including infectious-inflammatory genesis, and this, in turn, is the most important step towards development of methods for pathogenetic therapy of these diseases [44].
Etiology and pathogenesis of infectious and inflammatory periodontal diseases
Development of criteria for the laboratory diagnostic process
The current level of organization of the laboratory diagnostic process in dentistry can be clearly seen in the example of infectious and inflammatory periodontal diseases, the incidence of which in adults reaches 50-70% [3, 45].
As is known, the infectious-inflammatory process in the periodontium is most often initiated by virulent microorganisms of periodontopathogenic species, the influence of which alone, according to modern concepts, is not enough, since the characteristics of the response to pathogens of the macroorganism itself are of a certain importance for the development and progression of the pathological process [21, 41]. Once the infectious process is initiated, periodontal disease typically progresses with loss of collagen fibers and their association with dental cementum, migration of apical epithelium, deepening of periodontal pockets and alveolar bone resorption [36].
Modern ideas about the pathogenesis of the development of infectious and inflammatory periodontal diseases are described in some detail in the works of [24, 28, 45] and others, and the general scheme of their development may look as shown in Fig. 2.
Figure 2. Scheme of the pathogenesis of the development of infectious and inflammatory periodontal diseases.
In accordance with the presented scheme, the most important triggering factor in the initiation of the pathological process is the formation of dental plaque as a multilayer microbial biofilm with the participation of periodontopathogenic microorganisms [12, 29]. These include such causative agents of chronic inflammatory process in the periodontium as Tanerella forsythensis, Porphyromonas gingivalis, Treponema denticola,
as well as an inducer of acute aggressive inflammation,
Actinobacillus actinomycetemcomitans
[45, 50]. All of these periodontopathogens are a source of lipopolysaccharides (LPS), which can interact with damaged epithelial cells, neutrophil granulocytes, monocytes/macrophages, and fibroblasts through Toll-like receptors (TLRs) [28].
It should be emphasized that the process of interaction of periodontal pathogens with TLR cells is significantly different from that with the participation of normal microflora of biofilms. Thus, using a caries model, it was found that representatives of normal microflora, unlike pathogens, induce the formation of the cytokine TGFβ1 (transforming growth factor β1), which in turn inhibits the expression of TLR [27]. In contrast to this scenario, with the predominance of pathogenic microflora, a continuous flow of signals is provided through TLR, activating macrophages and other immunocompetent cells bearing these receptors [27], and inducing them to chemotaxis, secretion of proinflammatory cytokines (tumor necrosis factor α (TNFα), interleukins ( IL)-1, -6, -8), release of matrix metalloproteinases and other enzymes, production of immunoglobulins specific to microbial antigens, produced with the participation of T- and B-lymphocytes attracted by chemokines [24, 28, 45, 50]. Released enzymatic substances take part in the degradation of collagen and other extracellular matrix proteins, resulting in loss of contact between the periodontium and bone [3, 24, 45]. The role of pro-inflammatory cytokines is quite significant, which, in addition to inducing inflammatory changes in tissues, can activate osteoclasts and thus promote bone resorption of the alveolar processes [45].
As a result of all the described interactions, a complex complex of molecules appears in the gingival-cervical fluid, including electrolytes and other small molecules, proteins, cytokines, antibodies, bacterial antibodies, enzymes, and breakdown products of connective and bone tissues [18, 31, 39, 43]. All of these components can potentially be considered as biomarkers of infectious and inflammatory periodontal diseases.
In the table
presents the main and auxiliary biomarkers of infectious and inflammatory periodontal diseases, currently used for diagnostic and research purposes and identified in the analysis of biofilms, gingival-cervical fluid, and saliva.
These biomarkers are described in the most complete form by M. Taba et al. [45]. At the same time, M. Curtis and I. Gillett [15] once proposed to distinguish three categories of biomarkers:
1) indicators of current disease activity;
2) predictors of disease progression;
3) predictors of the disease in a currently healthy person.
Among these categories of biomarkers, a group of signs that allow predicting disease progression and reflecting quantitative characteristics of indicators deserves special attention.
Thus, using the example of infectious and inflammatory periodontal diseases, it is clearly seen that technical improvement of laboratory determination of biomarkers, its transfer to the level of quantitative testing is the most important task of dentistry, like any other clinical discipline, since it allows not only to accurately and timely diagnose the disease, but and predict its progression, complications and outcomes. From this point of view, modern methods of laboratory diagnostics and their capabilities deserve separate discussion.
Optical methods in laboratory diagnostics of infectious and inflammatory diseases of the oral cavity
Among the entire arsenal of methods for laboratory diagnosis of dental diseases, optical methods have always occupied a significant place due to their accessibility and information content. It is not without reason that histological examination of biopsy specimens of affected tissues has been and remains the “gold standard” of diagnosis. In recent decades, microscopic technology has undergone such significant changes that it allows us to speak of modern methods of microscopic examination not only as a scientific method, but also as a method of non-invasive intravital diagnosis of dental diseases.
There are several principles that form the basis of modern optical methods, among which confocal microscopy and scanning ion conductivity microscopy have acquired particular importance in medicine. For research purposes, electron microscopy has not lost its importance in dentistry [12].
The history of the creation of a confocal microscope dates back to the middle of the last century, when in the 50s biologists needed to increase the contrast of observing fluorochrome-labeled objects in thick tissue sections. To solve this problem, M. Minsky, a professor at the Massachusetts Institute of Technology in the USA, proposed using a confocal scheme for fluorescence microscopes. A confocal microscope is based on the principle of receiving a point signal from a fluorescent object in the thickness of tissue using a laser beam. In this regard, a confocal microscope, which has a high contrast, provides two invaluable opportunities: it allows you to study tissue at the cellular level in a state of physiological activity, and also evaluate the results of the study (i.e. cellular activity) in four dimensions - height, width, depth and time [37].
This technique turned out to be suitable not only for studying preparations from microorganisms or tissue sections, but since 1980 it began to be used for in vivo
[48]. Thus, with this method it became possible to determine the structure of epithelial tissues to a depth of 0.1-0.5 mm, while characterizing the cellular composition and microvascularization of periodontal tissues [52]. Particularly effective was the use of confocal microscopy to study the mechanism of biofilm formation in dental plaque and to identify, in particular, periodontal pathogenic microorganisms [29].
The principle of scanning ion conductivity microscopy (SCIM) was proposed in 1989 at the University of California by P. Hansma et al. [25] and is currently intended for the study of soft objects of biological nature, in particular, cells in the native state. The operating principle of the SMIP is based on the use of a glass micropipette as a probe, which records the ion current flowing through its internal hole with a radius of about 100-500 nm, which allows scanning the surface of the object. Using SMIP, it is possible to obtain detailed information about the functioning of biological cells with a nanometer level of spatial resolution [11].
The method can be used in vivo to study the functioning of cell membranes [33], to record the movement of cells and their contacts, and the interaction of cells with viruses and other microorganisms. Despite the wide possibilities of the method in the study of epithelial structures, the experience of using the method in dentistry remains only promising.
Methods of molecular biology in laboratory diagnosis of infectious and inflammatory diseases of the oral cavity
Molecular biology methods in dentistry include a wide range of methods for assessing the qualitative and quantitative composition of the oral microflora and biomarkers of various dental diseases. The most commonly used method is the polymerase chain reaction (PCR).
The PCR method was invented in 1983 by the American scientist Kary Mullis. He subsequently received the Nobel Prize for this invention. The essence of the method is that it imitates the natural replication of nucleic acids and allows one to obtain DNA sequence fragments characteristic of a particular microorganism in quantities sufficient for their recognition.
In accordance with this principle, PCR of a clinical sample includes three main stages: sample preparation (isolating DNA from clinical material), amplification cycles (multiplying DNA fragments) and recording the results. In each cycle, the number of copies of the amplified region doubles; in 30-40 cycles, short specific fragments accumulate in an amount sufficient for their further recognition. Detection of amplification products is carried out in different ways: using electrophoresis in an agarose gel, or by hybridization with a specific oligonucleotide probe, or using mass spectrometry, etc. [9].
PCR is very widely used for the detection and identification of microbial pathogens, including periodontopathogenic microorganisms [4, 7, 8, 35], and the method allows one to detect the pathogen in biological material even when other methods are ineffective. The diagnostic efficiency of PCR in this case increases significantly when it is combined with a culture-based diagnostic method [12].
In addition to microorganisms, PCR can be used to determine the expression of genes that regulate the formation of receptors or secretory products in the cell. In the latter case, an example is the discovery in osteoclasts of alveolar processes of genes that regulate impaired synthesis of type I collagen with the formation of telopeptides, while the detection of the corresponding genes after amplification is carried out by DNA hybridization [28].
The variety of PCR techniques tested in dentistry can be demonstrated by another example. It has previously been noted that periodontal microorganisms can initiate the production of proinflammatory cytokines and enzyme systems when interacting with cells that carry out innate immunity through Toll-like receptors (TLRs) [27]. The level of mRNA expression of TLR genes is usually determined by real-time PCR combined with reverse transcription using specific primers. In this case, mRNA serves as a template for the formation of complementary DNA (cDNA) using reverse transcriptase, and the latter is amplified using appropriate primers [51].
Another direction of using PCR promises certain prospects - the establishment of polymorphism of a number of genes associated with a high probability of severe chronic periodontitis. We are talking about allelic variants of the IL-1 gene - IL-1α +4845 and IL-1β +3954, according to which a person can be classified as either a “favorable” or an “unfavorable” genotype for the possibility of developing chronic periodontitis and the severity of its course [42].
In addition to PCR, molecular biology methods that are promising for dental clinical practice include mass spectrometry - a physical method for studying a substance by determining the ratio of the mass of charged particles of a substance to their charge (quality) and the number of charged particles formed during exposure to the substance. Using the method of mass spectrometry of various biological substrates, it is possible to solve one of the most important problems in medicine - determining disease markers by identifying proteins, the altered expression level of which can serve as a means of early, preclinical diagnosis of diseases [6]. In dentistry, there is an example of proteomic studies using mass spectrometry to study the composition of oral biofilms [30]. This method was used to determine the majority of biomarkers of infectious and inflammatory periodontal diseases related to the breakdown products of connective and bone tissue.
In recent years, the study of the salivary proteome as the basis for general clinical laboratory research has begun to occupy a significant place, along with studies of blood/plasma, cerebrospinal fluid, and urine [47].
Immunological methods in the diagnosis of infectious and inflammatory diseases of the oral cavity
To determine the molecular products of connective tissue degradation, bone resorption, and proinflammatory cytokines, immunoassay methods based on the use of labeled monoclonal antibodies are widely used. Monoclonal antibodies are highly specific antibodies that, as a rule, react to one antigenic determinant and are obtained using hybridoma technologies, i.e. by crossing immunocytes with plasmacytoma cells. The hybridoma cells obtained in this way have the ability to unlimited proliferation and synthesis of antibodies of only one narrow specificity, corresponding to the clonal specificity of the original immunocyte [1]. For use in immunoassay methods, monoclonal antibodies are labeled by crosslinking them with fluorochrome molecules, a radioactive label, magnetic particles or an enzyme. In the latter case, the use of labeled monoclonal antibodies serves as the basis for enzyme immunoassay.
Enzyme-linked immunosorbent assay (ELISA) is a method for detecting antigens or antibodies, based on determining the antigen-antibody complex by introducing an enzymatic label into one of the reaction components, followed by its detection using an appropriate substrate that changes its color. The basis for any version of ELISA is the determination of the products of enzymatic reactions when examining test samples in comparison with negative and positive controls. Most often, the hardware version of ELISA is reproduced as a “sandwich” method. A biological material containing the antigen being analyzed (microbial molecules, cytokines, biomarkers) is added to the carrier with immobilized antibodies. During the incubation process, at the first stage, an antigen-antibody complex is formed on the solid phase. Then the carrier is washed from unbound components and specific antibodies labeled with the enzyme are added. After secondary incubation and removal of excess antibody-enzyme conjugate, the enzymatic activity of the carrier is determined, which is proportional to the initial concentration of the antigen under study. At the stage of identifying a specific immunocomplex, the analyzed antigen appears to be sandwiched between molecules of immobilized and labeled antibodies, which gave rise to the widespread use of the name “sandwich” method. The enzymatic reaction (color reaction, in which the enzyme is usually a plant peroxidase) takes place in the presence of hydrogen peroxide and a substrate, represented by an uncolored compound, which is oxidized during the peroxidase reaction to a colored product. The intensity of staining depends on the amount of antigen detected. The result is assessed spectrophotometrically [5].
The enzyme-linked immunosorbent method has found wide application in almost all areas of medicine; it is also used in dentistry, including to determine biomarkers of oral diseases of an infectious-inflammatory nature. In particular, in case of periodontal diseases, the ELISA method is used to determine the content of such biomarkers as cytokines [17, 26, 27], proteoglycans [40], and peptide products of tissue destruction [49] in the gingival-cervical fluid. This principle is used in dentistry and as a rapid method for diagnosing HIV infection using samples from gingival contents [2].
In addition to the enzymatic principle of antibody labeling, the fluorescent principle is widely used in medicine. Fluorochrome-labeled monoclonal antibodies are widely used to detect microorganisms and biomarkers of various diseases in tissues - an immunohistochemical method described in the optical methods section. Fluorochrome-labeled monoclonal antibodies to immune system cell markers make it possible to determine the quantitative composition of the latter in various biological samples, including those from the oral cavity. The fluorescence inducer in this case is most often laser beams with different wavelengths, and the method of such detection is called flow cytofluorimetry [16]. Flow cytofluorimetry as a method for quantitatively characterizing the cellular composition of immunograms of biological fluids, as well as factors of bactericidal activity in the oral cavity, has found its use in various areas of dentistry, since it allows you to work with both the blood of patients and saliva [10, 46] and gingival-cervical fluid [27].
Conclusion
Thus, the development of technologies that form the basis of modern laboratory methods takes the diagnosis of dental diseases to a new methodological level. By creating the basis for the development of biomarkers of oral diseases, as shown in the example of periodontal diseases of infectious and inflammatory origin, modern laboratory technologies not only open up wide scope for identifying signs of a pathological process, but also make it possible to predict its course, complications, and outcomes based on quantitative monitoring.
How complex digital diagnostics are carried out
The most popular area for digital diagnostics is complex dental implantation with the installation of a complete fixed bridge prosthesis 1-3 days after surgery. Getting teeth back so quickly is quite a difficult task. After all, as a rule, the remains of patients’ own teeth are in poor condition or missing, and the bite is disturbed. The implant surgeon and orthopedist need to re-create the balance of the entire jaw system. But it is impossible to do this right away; muscles and joints need time to rebuild. That is why there is a so-called adaptation period or adaptation prosthesis, through which orthopedists set the vectors of change in combination with the necessary balance of load on the implants. As a result, in addition to aesthetics, prostheses must normalize the position of the joint and the functioning of the facial muscles - and such a large-scale task cannot be solved without careful functional diagnostics and planning.
Comprehensive functional diagnostics is important not only when installing an adaptive fixed prosthesis, but especially when replacing prosthetics. A permanent prosthesis on implants lasts for decades, but only if it functions without overload.
However, a detailed analysis of the initial situation is useful in any orthopedic treatment: when installing veneers, crowns, bridges, etc. Any intervention in the shape of the teeth shifts the balance - the chewing load is distributed slightly differently, the facial muscles are tensed differently, and the movement of the joints changes. Will these changes be for the better or will they lead to structural failure and complications? This can be done
Are there any disadvantages to digital diagnostics?
The disadvantages of high-precision digital solutions include their low prevalence due to the high cost of the equipment, as well as the time spent by the doctor. The technologies are relatively new and are just beginning to come into practice. There are still few doctors who have a full range of equipment and can carry out the analysis inside and out. Most are just learning new products and using only individual devices - for example, myographs or face arcs. That's why you won't see them in every clinic.
Smile-at-Once is so far the only clinic in Moscow with a full diagnostic range of devices and programs for planning orthopedic treatment and creating prosthetics.
Scanning facial parameters using the Proface scanner
The final stage with the participation of the patient is scanning of facial parameters. There are two options here - use a facial scanner and/or a special application for Mac OS on the iPad.
The Proface scanner or program creates a three-dimensional model of the patient's appearance. For this purpose, a specially developed craniometric analysis algorithm is used (craniometry is a technique for measuring the skull). That is, many points of the skull are calculated - due to this, a copy of the patient’s face and all the bones of the head is transferred to the computer.
In addition, photometry is carried out - photographing the face is necessary to evaluate the result “live” and maintain a digital photo record.
An example of photometry is photographing the face from all angles before and after dental implantation with the installation of a fixed prosthesis immediately
We approach diagnostics wisely! We use the latest developments and artificial intelligence! We make an accurate diagnosis and find the best solution to your dental problems.
Sign up for a consultation