July 30, 2020
To talk about local inflammation, you must first understand what lymphadenitis is in general. This is an inflammatory process in the lymph nodes, sometimes accompanied by suppuration
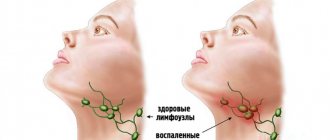
To talk about local inflammation, you must first understand what lymphadenitis is in general. This is an inflammatory process in the lymph nodes, sometimes accompanied by suppuration. It manifests itself through enlargement of one or more lymph nodes and can occur in several regions of the body at once. Clinical signs of the disease depend on the form and type of lymphadenitis: acute or chronic, regional (damage to lymph nodes of one anatomical group) and generalized (involvement of several groups of lymph nodes), serous, purulent, gangrenous, hemorrhagic, phlegmonous.
In the body, lymph nodes create a protective barrier against viruses, infections, cancer cells, participate in the formation of lymphocytes (special cells that destroy foreign microorganisms) and the production of phagocytes, antibodies (immune cells), participate in digestion and metabolic processes, distribute intercellular fluid between body tissues and lymph.
Normally, the lymph nodes are not palpable or are palpated in the form of elastic, small-sized formations that are not fused with adjacent tissues or with each other. Depending on the prevalence, the following types of lymphadenitis should be distinguished:
- local - enlargement of one lymph node in one of the areas (single cervical, supraclavicular lymph nodes);
- regional - enlargement of several lymph nodes in one or two adjacent areas (supraclavicular and axillary, supraclavicular and cervical, occipital and submandibular lymph nodes, etc.);
- generalized - enlargement of lymph nodes in three or more areas (cervical, supraclavicular, axillary, inguinal, etc.).
With axillary lymphadenitis, enlarged lymph nodes in the armpit are palpated. Symptoms of axillary lymphadenitis:
- Enlarged lymph nodes
- Painful sensations when palpating the affected area, turning the body, or moving
- Inflamed nodes are fused together with each other and adjacent tissues into one dense conglomerate
- The skin over the inflamed lymph nodes is hyperemic
- Symptoms of body intoxication appear - fever, weakness, headache, lack of appetite, feeling weak, muscle pain
Often the disease is accompanied by symptoms of the underlying disease; in addition, the patient may be bothered by:
- night sweats;
- weight loss;
- prolonged increase in body temperature;
- frequent recurrent upper respiratory tract infections;
- pathological changes on a chest x-ray;
- hepatomegaly;
- splenomegaly.
Causes of enlarged submandibular lymph nodes
Two groups of 6-10 lymph nodes, located symmetrically on the right and left in the tissue behind the arch of the lower jaw, collect lymph from the salivary glands, tonsils, palate, tongue, cheeks, nose, jaws and lips. Therefore, their increase is observed when these organs and tissues are damaged. Lymphoid hyperplasia is provoked by infections of the nasopharynx and oropharynx, dental pathology, local tumor processes, and may indicate the development of lymphoma and lymphogranulomatosis. Less commonly, damage to the lymph nodes is complicated by eye diseases - dacryoadenitis, stye on the eyelid.
ARVI
Infection with pneumotropic viruses is a common and obvious cause of benign lymphadenopathy, in which the submandibular and cervical lymph nodes simultaneously enlarge. Changes in the lymphoid tissue through which lymph from the oropharynx and nasopharynx are filtered are more noticeable with the development of ARVI during pregnancy and in children. In the first case, this is due to a physiological decrease in immunity to reduce the threat of miscarriage, in the second - with the age-related development of protective mechanisms.
Submandibular lymphadenopathy is more often observed with adenovirus infection, parainfluenza, infection with rhinoviruses or an association of viral pathogens. Typically, the lymphatic reaction is preceded by so-called catarrhal phenomena - runny nose, sore throat, pain when swallowing, dry cough, lacrimation. The temperature often rises, and to high (febrile) numbers - from 38 ° C and above. Characterized by moderate asthenia - weakness, weakness, fatigue. Muscle and joint pain is possible.
With ARVI, the skin over the submandibular lymph nodes has a natural color. The increase in lymphoid formations is slight (slightly more than 1 cm). The lymph nodes are compacted, but not rocky, have a smooth surface, and are mobile. During palpation, pain may be detected. As a rule, there is a symmetrical increase in nodes in both submandibular groups, which is associated with the spread of viral particles through the lymphatic system. As the infectious process subsides, the normal size and density of the submandibular lymph nodes are restored.
Sore throat and chronic tonsillitis
The second most common cause of enlarged submandibular lymph nodes is an infectious-inflammatory lesion of the palatine tonsils. Lymphadenopathy develops in both acute and chronic processes. With angina, the lymph nodes enlarge within 1-2 days from the onset of inflammation, in some cases reaching a diameter of up to 2 cm. The symptom occurs against the background of severe intoxication, an increase in temperature to 38-40 ° C, intense pain in the throat with painful swallowing and irradiation to the ears, severe headaches, muscle and joint pain.
With unilateral acute tonsillitis, the jaw lymph nodes on the corresponding side react more often; with bilateral acute tonsillitis, a lymphoid reaction is detected on the left and right. Often the cervical lymphatic groups are involved in the process. To the touch, the nodes are dense, painful, and mobile. The increase in size can persist for 1-2 weeks after the underlying disease subsides, then the diameter of the submandibular lymph nodes gradually decreases to normal, if the process has not become chronic.
Chronic tonsillitis is characterized by a symmetrical moderate enlargement of the nodes of both mandibular groups without involvement of the lymphatic formations of the neck. The pain is less pronounced. In a simple form of chronic inflammation of the tonsils, prolonged grade I lymphadenopathy often becomes the most noticeable manifestation of the disease. In patients with the toxic-allergic variant of tonsillitis, symptoms of damage to the tonsils are expressed with pain and sore throat, discomfort when swallowing, and bad breath. A persistent low-grade fever often persists.
Other infectious diseases
Damage to the submandibular lymph nodes is determined by a number of systemic infections, bacterial, viral and fungal processes affecting the respiratory system and salivary glands. The reaction of the submandibular nodes is due to the performance of a barrier function when pathogens enter the lymphatic system from the mucous membranes of the nose, oral cavity, and head organs. Mandibular lymphadenopathy manifests itself in such general and local infectious diseases as:
- Infectious mononucleosis
. The submandibular nodes are the first to respond to the introduction of the Epstein-Barr virus. Their increase is caused by lymphoid hyperplasia, primarily by the reaction of B-lymphocytes specifically affected by viral particles. At the initial stages of the pathological process, in addition to a local lymphoid reaction, low-grade fever is noted, a sore throat, and nasal congestion are felt. Later, the disease manifests itself as sore throat, generalized enlargement of the lymph nodes, liver and spleen. - Herpetic infection
. Hyperplasia of the lymph nodes of the submandibular groups is detected in herpetic stomatitis. Characterized by increased temperature, increased secretion of saliva, erosive and aphthous lesions of the oral mucosa. In addition to hyperplasia, inflammation of the lymphoid tissue with the development of mandibular lymphadenitis is possible. Kaposi's eczema herpetiformis is even more severe, in which the occipital and cervical lymph nodes are also affected, and vesicular, pustular, and erosive skin lesions are present. - Cytomegaly (CMVI)
. The involvement of the submandibular lymph nodes is due to the sensitivity of cytomegaloviruses to the ductal epithelium of the salivary glands with the occurrence of parotid sialadenitis as one of the pathognomonic signs of the disease. Submandibular lymphadenopathy is combined with the neck, high temperature, weakness, headache, and other signs of intoxication are determined. A clear clinical picture is observed in 4-5% of patients, while the manifestation of cytomegalovirus infection is more often observed in pregnant women. - Respiratory mycoplasmosis
. Moderate enlargement of the submandibular lymph nodes is characteristic of mycoplasma infections of the upper respiratory tract. Possible simultaneous damage to the cervical lymph nodes. Lymphadenopathy is preceded by a short period of catarrhal symptoms - a painful dry cough, runny nose with copious mucus, sore throat, injection of scleral vessels. In the future, respiratory mycoplasmosis can spread downward to the trachea, bronchi, and lungs. - Cat scratch disease
. The submandibular nodes are affected when a cat bite or scratch is localized in the facial area. Lymphadenopathy is quickly complicated by submandibular lymphadenitis. The combination of a lymphoid reaction with a reddish nodule (papule), and then an abscess (pustule) at the site of skin damage is pathognomonic. The inflamed lymph nodes are enlarged to 1.5-2 cm and are sharply painful. Lymphadenitis persists for up to 2 months and is accompanied by febrile temperature, weakness, fatigue, myalgia, and headache. - Scrofuloderma
. In lymphogenous colliquative tuberculosis of the skin, the leading symptom is the formation of dense reddish-purple nodes (tuberculous granulomas) in the area of the submandibular and cervical lymph nodes, from which dissemination of Koch bacilli occurs. An increase in lymphatic formations corresponds to lymphadenopathy I, less often II degree and complements suppurating subcutaneous tubercles, which break through fistulas and are slowly replaced by coarse scar tissue.
Dental pathology
The submandibular nodes serve as the main collectors of lymph from organs located in the oral cavity. Therefore, they are among the first to respond to any inflammation of the oral mucosa, dental tissue, upper and lower jaws. The reason for the enlargement of the lymph nodes is protective hyperplasia of the lymphoid tissue in response to the presence and proliferation of the pathogen, and in more severe cases, with lymphogenous spread of the process, infiltration of the stroma with inflammatory elements.
A moderately pronounced increase in the nodes of the submandibular group on the side of the pathology is observed in periodontitis, alveolitis, and periostitis of the jaw. Typically, lymph nodes become hyperplastic due to pain in the projection of the lesion, putrid odor from the mouth, low-grade or febrile fever, weakness, weakness, and other manifestations of intoxication. Submandibular lymphadenitis, which developed against the background of bright redness, multiple ulcerations, dirty gray plaque and foci of necrosis of the oral mucosa, is a sign of ulcerative necrotic stomatitis.
Malignant neoplasms
Lymphogenic metastases in the submandibular nodes are found in patients with late stages of oncological diseases of the head organs. A combination of mandibular lymphadenopathy with an increase in nodes of other groups is typical: for lip cancer - with mental and jugular nodes, for tongue cancer - with mental and occipital nodes, for cancer of the lower jaw - with cervical nodes, and for eye melanoma - with cervical and parotid nodes. Compaction and enlargement of the submandibular nodes is an important sign of malignant tumors of the salivary glands.
The detection of altered lymphatic formations usually indicates that the oncological process is old (early metastasis is typical only for tumors of the lower jaw and melanomas). The diameter of the nodes can reach 2 cm. To the touch they are defined as hard, rocky, sometimes have a bumpy surface, and are fused together with each other and the surrounding skin into a single conglomerate. Lymphadenopathy is preceded by pathognomonic signs of the tumor process - growths and ulcerations of the skin, mucous membranes, dense infiltrates, local pain, limitation of movements, etc.
Development mechanism
Enlargement of lymph nodes occurs in several ways, each of which involves the accumulation of a certain type of cell in the lymphoid tissue. The reaction of peripheral lymphatic organs is often associated with increased blood flow, proliferation of lymphocytes and macrophages in response to the appearance of foreign genes. With antigenic stimulation, the node can increase 5-15 times in 5-10 days. Systemic neoprocesses are characterized by active proliferation of degenerated lymphoid cells with an increase in the size of the affected lymph node.
The stroma of lymphatic formations can be infiltrated by inflammatory elements (in infectious diseases), tumor cells located in the lymphatic drainage zone of a given node. Metastatic lesions are often accompanied by proliferation of connective tissue. In some disorders of lipid metabolism (Niemann-Pick disease, Gaucher syndrome), macrophages filled with undigested glycosphingolipids are retained in the lymph node.
Axillary lymphadenitis in a child
Survey
Most often, patients who have identified enlarged lymph nodes in the submandibular area without other noticeable clinical manifestations turn to hematologists. In case of obvious pathology on the part of the head organs or probable signs of an infectious process (fever, skin rash, enlarged spleen, liver), doctors of the relevant profile are involved in organizing their examination. The diagnostic search is aimed both at determining the root causes of lymphadenopathy and at assessing the condition of the affected nodes. The most informative ones are:
- Ultrasonography
. Ultrasound of lymph nodes is used to quickly determine the size, shape, location, and structure of lymphoid formations. The method makes it possible to clarify the involvement of surrounding tissues in the process, as well as to differentiate lymphadenopathy from lesions of the salivary glands. - Radiodiagnostics
. In order to determine the characteristics of lymph flow in the affected area, lymphography using X-ray contrast is prescribed. In more complex diagnostic cases, CT scan of the lymph nodes is indicated. A valuable non-invasive diagnostic method is MRI of lymph nodes. - Biopsy
. Sampling of lymphoid tissue for histological examination is an accurate way to detect inflammatory processes, fibrous degeneration of the lymph node, and the degree of its damage by the oncological process. Biopsy of the lymph nodes of the submandibular zone is performed by puncture and open method. - Lab tests
. The examination begins with a general blood test, which reveals inflammatory changes and possible neoplastic changes in the composition of cellular elements. To confirm the infectious nature of lymphadenopathy, culture of a throat smear, RIF, ELISA, and PCR diagnostics are performed. - Special instrumental diagnostics
. To establish the cause of enlarged submandibular lymph nodes, pharyngoscopy, rhinoscopy, and otoscopy are performed. To exclude ophthalmological diseases, an examination of the eye structures is indicated. In case of possible dental pathology, radiography of teeth and jaws and other instrumental studies are used.
Ultrasound examination of the submandibular lymph nodes
Fact #2
Lymphatic vessels are not something abstract.
It is worth crossing or ligating them, for example, during surgery on the axillary lymph nodes for breast cancer, and lymphostasis is likely to develop - swelling of the limb, which, again, most likely will not go away.
The most visible to us from the point of view of examination - the so-called peripheral lymph nodes (in the neck, supraclavicular, axillary and inguinal) can increase, and this is in most cases a manifestation of reactive lymphadenopathy - an inflammatory reaction indicating the fight against infection.
Symptomatic therapy
Before prescribing special treatment, rinsing with antiseptic solutions is effective in order to more quickly restore the size and density of the submandibular lymph nodes in case of ARVI, sore throat, and other inflammatory processes in the oral cavity. In the presence of combat syndrome, it is possible to take analgesics. In other cases, therapy is selected only after the causes of the condition have been established. The combination of lymphadenopathy with fever, rapid deterioration in health, headache, or detection of tumor formations in the head area is an indication for emergency medical attention.
Treatment of axillary lymphadenitis
Treatment tactics for axillary lymphadenitis depend on the form and cause of the disease. In most cases, lymphadenitis does not require special therapy and goes away on its own after the underlying disease is eliminated. If the process is complicated by suppuration, then the treatment tactics completely change.
General recommendations: maintain rest, immobilize the affected area (do not rub or injure the affected lymph nodes), proper nutrition, take painkillers, anti-inflammatory medications. Therapy for acute axillary lymphadenitis depends entirely on the stage of the disease. Conservative treatment is used for the initial stages: UHF therapy, sanitation of the source of infection (opening of abscesses, leaks, cellulitis, drainage of the abscess), antibiotic therapy taking into account the sensitivity of the microbial flora in the main focus.
Surgical intervention is necessary for purulent axillary lymphadenitis: adenophlegmon, abscesses are opened, pus is removed, and the wound is drained. It happens that a biopsy confirms the presence of a tumor process - benign or malignant. Treatment may include radiation and chemotherapy. In the case of lymphadenitis, as in the presence of any other diseases, it is extremely dangerous to self-medicate.
Back to articles
Gingivitis and lymph nodes
Gingivitis is an inflammatory disease of the gums that occurs due to the formation of plaque on the teeth and the spread of microbes. It often develops in people who do not take good care of their oral hygiene. Typical symptoms of gingivitis are itching and bleeding of the gums, swelling, and pain, especially when soft tissue comes into contact with hard objects, such as a toothbrush.
This pathology can occur in various forms. If the lymph node is inflamed, it may be ulcerative-necrotizing gingivitis. Its other signs are:
- strong pain;
- copious amounts of saliva;
- formation of ulcers;
- increased body temperature;
- loss of appetite;
- headache.
One of the complications of gingivitis if left untreated is periodontitis.
Preventive measures
No one is immune from the problem described. But there are ways to minimize the risk of its occurrence. Among them:
- receiving qualified medical care for any ailments;
- annual laboratory tests;
- timely treatment of emerging dental diseases;
- sanitation of the oral cavity every six months;
- following medical prescriptions.
Take care of your health, and the risk of enlarged lymph nodes will be minimized.