Giuseppe Cantatore University of Verona (Italy). Department of Endodontics. Assistant professor.
In a classic study published in 1985, Bystrom et al. compared the sterilizing effectiveness of three different methods of endodontic treatment of infected canals and found that mechanical treatment in combination with irrigation with saline solution ensures canal sterility in 20% of cases, while replacing NaCl with a 5% sodium hypochlorite solution leads to canal sterility in 50% of cases. cases, and the addition of the latter scheme with a single temporary filling of the canal with calcium hydroxide increases the percentage of canal sterilization to 97%. Does this mean that when treating infected root canals, temporary filling with medicated paste is required in all cases? More than 15 years have passed since the Bystrom et Al study; Today we know much more about the properties of microorganisms associated with pulp-periodontal pathology: from virulence to mobility, from the ability to penetrate dentinal tubules to sensitivity to various antiseptics. 15 years of research experience have shown that many irrigation solutions have pronounced bactericidal activity against microorganisms such as enterococcus faecalis or candida, which are resistant to calcium hydroxide or chlorophenol. In this article, we will discuss in 7 points how to improve the root canal irrigation procedure, using the right products in the right sequence, in order to reduce the need for additional medicinal treatment of the canals between visits.
Key Factors for Effective Cleaning and Irrigation of the Root Canal System
1. Careful diagnosis of existing pulp-periodontal pathology
2. Taking into account the condition of the tooth tissues and the complexity of the anatomy of the root canal system 3. Removal of the endodontic smear layer 4. Compliance with indications when choosing means for irrigation 5. Optimization of the active components of the irrigation solution 6. Correct sequence of application of the irrigation solution during root canal treatment 7. Mandatory costs of at least 5 minutes for irrigation before filling
Modern aspects of the use of adhesive systems
Fig.1. Three mechanisms of binding the adhesive system to dental tissues (A.I. Nikolaev, L.M. Tsepov, 2001). The negative aspects of the listed binding mechanisms are also micro-leakage, depressurization and the development of recurrent caries under the filling. On the other hand, a characteristic feature of these techniques is the low percentage of postoperative sensitivity. A feature of the third bonding mechanism (total etching or bonding technique) is the deep penetration of the components of the adhesive system into the open dentinal tubules, which makes it possible to achieve fairly strong mechanical adhesion to dentin. In addition, the mechanical connection is further enhanced by various chemical bonds of the individual components of the adhesive system with the inorganic and organic components of dentin. Double chemical bonding along with micromechanical bonding in the dentinal tubules made it possible to achieve significant bonding forces of these adhesive systems to dentin (up to 31 MPa). This adhesion force to dentin is characteristic of the latest generations of adhesive systems. Despite such a high rate of adhesion of modern dentin-binding mediators, there is still no complete confidence that the use of these materials eliminates the possibility of marginal permeability. All this is due to the fact that adhesion in relation to the dental surface is always in conflict with the polymerization shrinkage of the material. While developing a high adhesion force to dentin, adhesive systems are simultaneously subjected to a certain force of polymerization shrinkage. Composites undergo significantly greater shrinkage. For example, shrinkage of light-polymerizing composites proceeds faster over time and the interradical bonds of the resulting polymer are subject to severe stress, remaining in a tense state. It is especially important to take into account the high “C-factor” (the large size of the connected surfaces of the filling in relation to the free ones), as a result of which the composite may tear off, carrying the hybrid layer with it. Clinically, this results in postoperative sensitivity. With a low C-factor, the adhesion force exceeds the stress caused by polymerization shrinkage and the integrity of the restoration is not compromised. In addition, the total bonding technique is characterized by a number of negative features:
1. Limited use in cases of pronounced mineralization of carious and non-carious lesions due to the difficulty of opening the dentinal tubules. 2. The possibility of acid penetration directly into the tooth pulp when etching deep carious cavities with the ensuing consequences. 3. Postoperative pain due to possible leakage of dentinal fluid if the rules for etching dentin are violated. 4. Possibility of infection of tooth tissues when the dentinal tubules open. 5. Multi-stage implementation. 6. Adhesive systems, as liquids with higher viscosity, are not stable in shape and flow under the influence of tangential stress during chewing, which leads to a violation of the marginal seal. 7. This technique cannot be used for the restoration of permanent teeth in children at high risk of developing caries.
I would also like to touch upon some aspects of the use of modern adhesive systems, which, in my opinion, have not received enough attention in the scientific literature. The first reaction of a tooth to caries is dentin sclerosis. In this case, the dentinal tubules are partially or completely filled with mineral deposits. The degree of mineralization of sclerotic dentin probably depends on the nature of the damage and the functional state of the odontoblast layer. Often one encounters mineralization that is difficult, and sometimes impossible, to remove along with the smear layer by etching dentin with acid. Oddly enough, not a single manual on therapeutic dentistry pays due attention to this issue. When opening the dentinal tubules with acid, the emphasis is usually on removing only the smear layer. It seems that the entrance to the dentinal tubules is closed only by the smear layer, and it does not matter that sclerotic dentin blocks the tubules in 95% of cases with carious lesions. At the same time, it is necessary to take into account the possibility of the formation of replacement dentin, which is formed in 63.6% of teeth with carious lesions. The latter, with pronounced mineralization, is more difficult to etch than sclerosed. In addition, with deep carious cavities, it is the replacement dentin (if it has formed) that can separate the bottom of the cavity from the dental pulp in the event of complete or partial destruction of the dentinal tubules by the carious process. Therefore, it is hardly appropriate to talk about the technique of total bonding in this situation. From all of the above, we can conclude that protective-adaptive zones, with adequate mineralization, prevent the high-quality implementation of the total bonding technique, as a result of which the indications for the use of this technique are narrowed. It is important to note that the question of the advisability of opening the dentinal tubules during adhesive measures has not yet been clearly resolved. Is it even worth opening the dentinal tubules to penetrate the elements of the adhesive system deep into the dentin, if there is no hypersensitivity, if optimal conditions for the functioning of the tooth have developed under the smeared and sclerotic layers? This approach is also confirmed by the fact that opening the dentinal tubules is a very important and unpredictable step. Analyzing my many years of practical activity, I can say that earlier, when there were no adhesive systems and acid etching of tooth tissue was not used, postoperative sensitivity was observed much less frequently. In addition, these complications were, as a rule, chronic in nature, because If the diagnosis was made correctly, there was practically no need to observe postoperative sensitivity on the second or third day after filling. This picture is explained by the absence at that time of adhesive systems and composites, which, despite having less shrinkage than cements, developed stronger polymerization stresses. That is why polymerization shrinkage when using composites, especially light-curing ones, is characterized by a more acute course and an earlier period of occurrence. Based on modern ideas about polymerization shrinkage of filling materials, it is possible to explain the supposedly miraculous effect of protective linings. The lining should be considered not as a means to prevent thermal factors and the negative impact of the chemical components of a permanent filling on tooth tissue (as was previously thought), but as a means to prevent the traumatic effects of polymerization shrinkage. This approach is due to the fact that the linings do not have sufficient binding force to dentin (0.7-7 MPa) and during polymerization shrinkage there is no strong stress in them. It is also important to note that the fixation of composites is based on demineralization of dentin in order to renew collagen fibers and penetrate the latter into monomer. The reliability of this connection in terms of durability has been questioned over time (Graham Mount, 2002). It was assumed that collagen, which was demineralized by acid etching, becomes devitalized and later undergoes destruction, which leads to a loss of strength of the joint itself. From all of the above, we can conclude that the total bonding technique is not without its drawbacks and can be used for:
1) production of small-sized restorations; 2) restoration of cavities with a low “C-factor”; 3) unsatisfactory conditions for retention of filling material; 4) restoration of hypersensitive teeth (hypersthesia); 5) restoration of pulpless teeth.
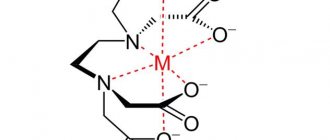
I want to pay special attention to the latter, because... in this case, the total bonding technique has some peculiarities. In the dental literature, little attention is paid to the interaction of the adhesive system with the dentin of a pulpless tooth, but the structure of the dentinal tubules in this case is completely different and requires a different approach. It is obvious that after extirpation of the pulp, blood and lymphatic vessels, the structure of the dentinal tubules also changes. In particular, the amount of water decreases. The “wet” bonding technique alone is not enough in this case. The clinician should take into account that during depulpation the oil layer is formed not only at the root, but also partially at the mouth of the tooth crown. Removal of the oil layer, as opposed to the smear layer, is only possible thanks to a combination of EDTA 15% and NaOCl 5.25%. Therefore, etching and applying an adhesive system without first removing the oil layer at the mouth of the tooth crown will lead to deterioration in the adhesion of the composite to the walls of the prepared cavity. In all other cases, it is inappropriate to use the total bonding technique, so I would like to offer an alternative technique, which, in my opinion, is more acceptable in similar situations. It is currently accepted that the adhesion of dentinal adhesive occurs primarily due to micromechanical bonding in the area of intertubular dentin, and not due to the penetration of elements of the bonding system into the dentinal tubules and the formation of protrusions in them (E. Helwig, J. Klimek, 1999) . It was also shown that when using the third generation adhesive "GLUMA", the bond strength to dentin increased when the smear layer was removed with EDTA. Preliminary etching of the dentin surface with orthophosphoric acid with opening of the dentinal tubules, on the contrary, reduced the bonding force and increased postoperative sensitivity (A.V. Borisenko, V.P. Nespryadko, 2001). Noteworthy is the research of DHPashley, who showed that acid etching of dentin caused a significant release of fluid from its tubules, so the bond of the composite to dry dentin was stronger than after etching. In addition, the scientist convincingly proved that, despite a significant increase in the adhesion of the adhesive system to dentin, when etching the latter, the main indicator of the strength of the bonding system is the addition of a mechanical bond to a chemical bond. It has also been shown that the orientation of the dentinal tubules is of secondary importance for bond quality. It should be especially noted that fourth and fifth generation adhesive systems provide a fairly strong bond with dentin even in the absence of acid etching. This phenomenon is explained by the high penetrating ability of the primer and the presence in it of organic or other solvents (acetone, alcohol), surfactants that penetrate deeply into the thickness of the dentin. Based on this, depending on the clinical situation, I believe it would be advisable to use conditioning instead of etching tooth tissues. As is known, this method is successfully used for the adhesion of glass ionomer cement to dentin, for which the surface of the prepared cavity is cleaned of the smear layer without opening the dentinal tubules. In clinical conditions, this is achieved by conditioning the dentin with a 10% solution of polyacrylic acid for 10 seconds, which is necessary for the full formation of the ion exchange layer between the glass ionomer and the tooth tissues. Using composites, conditioning can be used in cases where etching dentin with 37% phosphoric acid is not practical. Conditioning, like etching, increases the bonding strength of adhesive systems to tooth tissue. According to the laws of physics, the optimal degree of adhesion occurs between two smooth surfaces. Along with this, during conditioning, the dentinal tubules are not opened and the protective-adaptive zone (sclerosed dentin) is not destroyed, as a result of which the possibility of postoperative sensitivity is significantly reduced. “open dentinal tubule” stage is an advantage of conditioning over etching. This stage lasts approximately 30 seconds. – this is exactly the time required for the adhesive system to penetrate the open dentinal tubules and form a hybrid layer. As a rule, this period is the main cause of many complications, because at this time, dentinal fluid may leak out and the tubules may become infected. It is on this basis that, working on sixth and seventh generation adhesive systems, many manufacturers combined the stages of etching and priming. The use of such systems involves infiltration of hard tissues with resins at the same time and to the same depth as demineralization. Preconditioning when using sixth and seventh generation adhesive systems will prevent not only possible infection of the dentinal tubules when using a self-conditioning primer, but will also increase the adhesion strength of the adhesive to the tooth tissues. Unfortunately, in many dental publications, the processes of conditioning and etching are often equated. Although they all have in common the complete removal of the smear layer, the significant difference is the presence or absence of open dentinal tubules. It is difficult to agree with the authors who do not pay attention to such an important circumstance, identifying these essentially different methods. Thus, we can conclude that when using composites and adhesive systems, conditioning should be used in cases where the total etching technique is not practical. When working with adhesive systems, I believe it is unacceptable to leave a smear layer on the dentin surface. Conditioning, like etching of tooth tissues, allows for good adaptation of the composite to tooth structures and increases the bonding strength of adhesive systems to dentin. This technique can be combined with any type of adhesive system. The most preferred adhesive systems for these purposes are those containing particularly small filler particles, so-called nanofillers ["One Step" ("Bisco"), "Optibond Solo (Kegg)]. The average size of nanofiller particles is 0.001-0.008, which allows them to easily penetrate dentinal tubules of any size (the average size of a dentinal tubule is 0.8 mm). Nanotechnology makes it possible to achieve sufficient bond strength with dentin even without using the “total bonding” technique.
Material taken from the author’s monograph “Modern kariosology”
Description[edit]
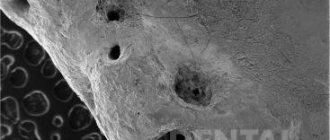
Early studies of dentinal walls after cavity preparation by Brännström and Johnson (1974) showed the presence of a thin layer of debris ranging from 2 to 5 micrometers in thickness. [1]
In 1975, McComb and Smith first described the smear layer. They observed an amorphous layer of debris with an uneven and granular surface on the walls of instrumented dentin using a scanning electron microscope (SEM). A thin granular microcrystalline layer of debris was 2-5 micrometers thick and was located on the channel wall. [1] [2] The authors stated that "most standard instrumentation techniques result in the canal wall being smudged and clogged with debris." [3]
In the same year, Mader et al. studied the morphological characteristics of the smear layer on teeth that were endodontically treated with k-type files and irrigated with 5.25% NaOCl. [4] The smear layer was examined from both sides; the first aspect looked "from above" at the smear layer, and the second - from the side. SEM micrographs showed that the smear layer was composed of two merging components. They have been described as a thin superficial layer, 1-2 micrometers thick, covering the densely packed layer, and a second one penetrating the dentinal tubules up to 40 micrometers. The packed material showed finger-like structures protruding into the tubules from the canal wall. [5]
Sandblasting dentin.
This type of treatment involves supplying Al2O3 particles under high pressure to the surface being treated. This is a fairly old method; in dentistry it was used mainly by dental technicians to clean and roughen the surface of the denture. In the clinic, portable sandblasting machines are used, and their main disadvantage is the disposal of aluminum oxide dust. The positive aspects of the method are the absence of vibration and noise during processing, which increases patient comfort.
When colliding with dentin, Al2O3 particles break intertubular dentin and, as it were, fold it over the dentinal tubules, forming an uneven rough surface.
Many manufacturers claim that sandblasting creates a surface that does not require etching and that adhesion will be quite high due to micro-retention. But as many studies have shown, this type of treatment only increases the surface of the dentin, and not the strength of the ligament. Therefore, with this type of treatment, adhesive preparation should be carried out in full.