Features of the parotid lymph nodes
Parotid lymph nodes are those located in front of the ear, running along the tragus from top to bottom from the side of the cheek
The parotid lymph nodes react acutely to the presence of an infectious pathogen in the human body. It is possible that the disease that caused the inflammation of these formations does not pose a serious threat to health or life. But also, enlargement of the lymph nodes in this part of the body can occur due to the development of a dangerous pathology, which, if progressed, leads to serious complications.
Anatomy and physiology
The parotid lymph node is located in the front of the ear, in a place that is close to the cheekbone and cheek. The second node can be felt closer to the lobe, behind the auricle.
Normal sizes
Inflammation of the lymph nodes located in front of and behind the ear can be determined by their size. In a healthy state, they are much smaller than the structures that are located in the neck or groin area.
The parotid lymph node, which is located on one side, has a size of 3-5 mm. This is the norm for men and women. If the lymph node undergoes an inflammatory process, it increases to 3 cm or more.
Chronic mumps
Acute mumps rarely becomes chronic, so chronic mumps often occurs as a primary disease.
Chronic mumps are classified into 2 groups: parenchymal and interstitial.
Chronic parenchymal parotitis
Chronic parenchymal parotitis is often asymptomatic. However, the clinic is varied. Patients may complain of swelling, pain in the gland area, and a taste of pus in the mouth. The disease lasts a long time, periodically exacerbating. Most often one gland is affected.
Objectively we can see a swelling of the gland with clear contours. Palpation is painless, the gland is dense, the surface is lumpy. When massaging the gland - saliva with pus.
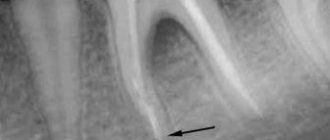
Diagnostics
For diagnosis, a contrast sialogram is performed. On the sialogram you can see deformation and/or necrosis of the ducts of 2-4 orders and the parenchyma of the gland - in the image there are cavities filled with a contrast agent. As the disease progresses, the cavities merge, areas of necrosis increase until the glandular tissue is replaced by fibrous tissue.
The radiosialographic method allows us to identify the stage of the disease. At the initial stage, there is a rapid accumulation of radioactivity. In the stage of pronounced signs - slow accumulation. In the late stage, radioactivity is low.
The cytological method for diagnosing punctate and gland secretions is also used.
Treatment of chronic parenchymal parotitis
Treatment of chronic parenchymal parotitis is difficult due to the inability of dead gland tissue to regenerate. Therefore, the dentist’s task is to relieve the disease.
The gland is stimulated with ocular probes and washed every day with antibiotic solutions and massaged, freeing it from solution and pus until clear saliva appears. The ducts can also be washed with chymotrypsin, a solution of potassium iodide. Novocaine blockades and radiotherapy are indicated.
With frequent relapses, extinguishing the function of the gland is carried out by three times instillation of ethyl alcohol with increasing concentrations of 60-80-96.
Surgical treatment: parotidectomy, extirpation of the parotid duct + denervation of the auriculotemporal nerve.
Reason to visit the doctor
A person needs medical attention if they have symptoms that indicate inflammation and tenderness of the parotid lymph nodes.
It is not recommended to wait until the inflammation goes away on its own. If the pathological process is not suppressed, the disease will progress. As a result, the patient will experience complications that will significantly worsen his overall health.
If you suspect inflammation of the formations of the lymphatic system, you need to go to the hospital. With such problems, it is customary to go to an appointment with a therapist or infectious disease specialist.
Enlarged lymph nodes: causes
The main reason for contacting a specialist is an enlarged parotid lymph node. By itself, this education cannot become larger. Before starting therapy, it is necessary to find out the reasons that could lead to inflammation. A competent specialist will help you cope with this task.
Enlarged lymph node syndrome as a pediatric problem
The cause of enlarged lymph nodes in most cases is processes not related to hematological malignancies: most often these are general pediatric, infectious, immune and other conditions
The fact that a pediatrician quite often discovers enlarged lymph nodes (LNs) in his patients and he has to quickly find an answer to the questions “why?” and “what to do?”, allows you to do without a long introduction. Thus, when conducting pediatric screening and subsequent analysis of 1607 diagnoses of acute and chronic diseases in children and adolescents aged 5–17 years, it was revealed that lymph node diseases were detected in 3.35% of cases [6]. Traditionally, when enlarged lymph nodes are detected, without taking into account other components of this syndrome (history, general clinical picture, local symptoms), the pediatrician thinks about an oncohematological disease. As a result, such patients make up 40% of all patients of oncohematologists [7], which seems unjustified. The frequency of newly diagnosed cases of oncohematological diseases in our country is low. The incidence of acute leukemia is 4.0 - 5.0 cases per 100,000 children per year, non-Hodgkin's lymphoma - 0.9 - 1.1 per 100,000 children per year. This makes it clear why the overwhelming majority of children with enlarged lymph nodes return from hematologist appointments to pediatricians with a diagnosis of lymphadenitis. That is, the reason for the increase in lymph nodes in most cases is processes not related to hematological malignancies: general pediatric, infectious, immune and other conditions. Based on the above, we decided to present our point of view on swollen lymph node syndrome.
| Figure 1. Submandibular lymph nodes in lymphogranulomatosis (ultrasound, 7.5 MHz) |
| Figure 2. Submandibular node in tuberculosis (ultrasound, 7.5 MHz) |
LN enlargement can result from lymphadenitis (LA) and lymphadenopathy (LAP).
LA is an inflammation of the lymph nodes that occurs as a complication after various purulent-inflammatory diseases and specific infections (tuberculosis, actinomycosis, plague, etc.). LA is usually a secondary process.
LAP is a systemic enlargement of lymph nodes, not associated with inflammation (effects of certain medications, proliferation, metastasis, etc.).
The epidemiology of PA and PAP has not been developed. One can only note that, according to I. S. Tarasova [6], in continuous mass studies of children in the Bryansk region, LA occurs, as one would expect, somewhat more often (1.86% among all examined) than PAP (1.49 % of the total contingent).
Methods for studying lymph nodes should be standardized as much as possible. In clinical practice, complaints are assessed (local pain, local or general increase in temperature, general somatic complaints), anamnesis (epidemiological history, duration of onset, localization of enlarged lymph nodes in one or several groups, their simultaneous increase or gradual increase, speed of disease manifestation, etc.) . Examination of the patient is of particular importance. Along with a thorough general pediatric examination by system, it is necessary to pay attention to the number of altered lymph nodes and their location by group. The size of the lymph nodes should be assessed only objectively: in millimeters or centimeters. Comparison of the size of LU with grain, peas, cherries, hazelnuts or walnuts, which is accepted in our country and widely recommended in the domestic literature, is irrational, gives incomparable results and should be eliminated. It is necessary to carefully record the ratio of enlarged lymph nodes to each other. For example, the location of lymph nodes according to the “solar system” type (one large lymph node in the center and on the periphery of it lymph nodes of smaller diameter) is typical for tuberculous lymphadenitis [2]. LNs can be elastic, dense, with fluctuation phenomena. The adhesion of the lymph nodes to neighboring nodes and surrounding tissues, the presence or absence of pain on palpation, must be described. It is necessary to examine and describe the condition of all accessible lymph nodes: occipital, submandibular, anterior and posterior cervical, supra- and subclavian, axillary, elbow, inguinal, popliteal. Inspection and palpation data are supplemented, confirmed and clarified by instrumental techniques. First of all, these are non-invasive imaging methods used to study deep-lying lymph nodes. They allow you to accurately determine the size of lymph nodes, changes in groups of lymph nodes that are inaccessible to inspection and palpation, characteristics of the capsule, adhesion, topographical features, internal structure; exclude conditions simulating lymph node enlargement (tumors not originating from lymph nodes, hematomas, kidney anomalies, etc.). It is extremely important to obtain information about the condition of the liver and spleen. In terms of accessibility and speed of obtaining information, echography (ultrasound) ranks first. LNs with a diameter of less than 1.5 cm are close in density to the surrounding adipose tissue, are rarely visualized, and it is almost impossible to limit their tumor damage from other causes of enlargement only according to ultrasound data. Such lymph nodes are observed primarily in infectious processes, reactive lesions, and in children with hemoblastoses - in a state of complete remission. LNs with a diameter of 1.5 - 2 cm are well visualized if they are projected onto echo-negative structures or change the usual topographic-anatomical relationships. The entire spectrum of ultrasound changes can be reduced to several main groups [3].
1. The enlargement of individual lymph nodes is assessed as small if they do not lose their usual ultrasound picture, retain the capsule, clarity and evenness of the contour, and do not change the topic of the organ. This type is typical for infectious lesions, especially tuberculosis, viral hepatitis, collagenosis, immunodeficiency, hemoblastosis in children at low risk.
2. Further growth of lymph nodes leads to the appearance of masses merging with each other, pushing aside the vessels. It is observed with purulent melting of a group of lymph nodes, with hemoblastosis, metastatic tumors.
3. Compression or pushing aside of internal organs. In this case, hydronephrosis may occur due to compression of the ureters, significant displacement of the uterus and bladder. Typically for extremely unfavorable variants of myeloid leukemia, Hodgkin's lymphoma and non-Hodgkin's lymphoma.
Ultrasound findings can be confirmed by computed tomography (CT). Additionally, CT allows one to clarify the structure of lymph nodes, their topographic relationships, and detect other groups of lymph nodes.
If it makes sense to evaluate superficial lymph nodes only echographically, and mesenteric and retroperitoneal lymph nodes are almost equally well detected by ultrasound and CT, then intrathoracic lymph nodes are detected almost exclusively radiographically.
| Comparison of the size of lymph nodes with grain, peas, cherries, hazelnuts and walnuts, which is accepted in our country and widely recommended in the domestic literature, is irrational, gives incomparable results and should be eliminated |
Diagnostic methods such as isotope scintigraphy and lymphography can be used according to very strict indications in specialized clinics or limitedly in dynamic studies and are not used in widespread practice.
Reliable identification of the causes of lymph node enlargement is possible only by histological methods. In this case, the material should be obtained only by open biopsy of lymph nodes, although modern techniques of fine-needle biopsy make it possible to obtain reliable results. The previously recommended puncture biopsy gives a very high percentage of false-positive and false-negative results.
LN enlargement can be schematically [5, 11] presented (with a description of some practically significant but little-known forms) as associated with infection (IA) and not associated with infection (PAP).
1. LA of viral nature.
- cytomegaly.
- Infectious mononucleosis.
- measles.
- rubella.
- psittacosis.
- Ardmore's syndrome.
An infectious disease, most likely of a viral nature, the peak incidence is observed in the fall, and is transmitted by airborne droplets.
The contagiousness index is high, the incubation period is 3-10 days. It begins with pharyngitis, rhinitis, low-grade fever. It occurs with a generalized enlargement of lymph nodes, a painful enlarged liver (less commonly, splenomegaly), myalgia, and chest pain. Recovery without consequences. 2. LA for bacterial infections.
- caries.
- abscess.
- cat scratch disease. Called Bortanella (Rochalimeae) hensella. More often, bilateral inflammation of lymph nodes (including mesenteric and intrathoracic) with general and skin nonspecific symptoms, which occurs benignly with spontaneous recovery, is caused by skin wounds from cats, dogs, and, less often, from foreign sharp objects. Granulomatous hepatitis, splenomegaly, encephalitic reactions, and convulsive syndrome have been described [8, 10]. It is observed mainly in children and adolescents, mainly in late autumn and winter.
- Borreliosis. Known as pseudolymphoma. Lymphoproliferative lesions of lymph nodes and skin during infection with Borrelia burgdorferi after a tick bite. Transitions to malignant lymphomas have been described.
- Tuberculosis. Along with the typical forms of tuberculosis, one should remember about the so-called. atypical mycobacteriosis. According to F. Miller [2], up to 50% of submandibular lymph nodes in children under 5 years of age are caused by atypical strains of mycobacteria (in particular, the avium type), and the probability of mycobacterial lesion of lymph nodes is higher, the younger the child (Fig. 1).
- Sepsis.
- Allergic subsepsis. It is also considered as a variant of juvenile rheumatoid arthritis, the so-called. Still's disease.
- Syphilis. The rate of increase in the incidence of syphilis in children is significantly higher than that in adults. Thus, the incidence of syphilis among adults increased 15.8 times over 4 years, and among children - 21 times. 65.6% of children became infected through sexual contact [1].
- Genito-anorectal symptom complex is a complication of chronic PA in chlamydia serotypes L1-L3 with periproctitis, chronically recurrent perianal and perineal fistulas, strictures and fibrosis of the genitourethral tract, and elephathiasis of the vulva. It occurs mainly in female patients.
3. LA for fungal diseases.
- histoplasmosis.
4. LA for parasitic diseases.
- echinococcosis.
5. LA for protozoal infections.
- toxoplasmosis. The subclinical variant is cervical subacute necrotizing PA. Clinically - painful, often cervical PA, with spontaneous remission after 3 - 6 months, fever, exanthema. Neutropenia. Histologically - coagulative necrosis with histiocytic and immunoblastic cells without granulomas, without neutrophils. Differential diagnosis is carried out with malignant lymphomas, tuberculosis, histiocytosis, and according to histology (vasculitis) - with systemic lupus erythematosus.
- kala-azar.
- malaria.
Forms not associated with infections (PAP)
1. Medicinal PAWS.
- Hydantoin derivatives (diphenin, etc.) are anticonvulsants. With this complication of therapy, PAP is considered autoimmunoblastic.
- allopurinol (used in the treatment of hyperuricemia, including myeloproliferative conditions).
- anti-leprosy drugs (used in gastroenterology for the treatment of chronic colitis, in rheumatology - for the treatment of arthritis and spondyloarthritis, especially those associated with the histocompatibility antigen HLA B-27).
- post-vaccination.
- against the background of foreign bodies.
2. With systemic processes in the body.
- collagenosis (in this case, the greatest increase in lymph nodes is still recorded in infected variants of diffuse connective tissue diseases, that is, there is a combination of LA and PAW).
- local tumor-like amyloidosis. Traditionally described as a pathology exclusively of adults [4]. However, we found this form of dysproteinosis in 2 of 44 children with systemic amyloidosis. Local tumor-like amyloidosis in our patients occurred with a pronounced general paraspecific reaction, which, in combination with a palpable mass in the abdominal cavity, initially led to an erroneous diagnosis of lymphoma.
- Lubarch amyloidosis, genetically determined. Generalized PAP, orthostatic hypotension, obstructive infiltrative cardiomyopathy, splenomegaly, neuropathy, carpal tunnel syndrome.
- Dorfman-Rosai syndrome (intermittent benign lymphadenopathy). Probably an autoimmune disease with benign proliferation of plasma cells, histiocytes, and fibroblasts. The peak incidence is in the first 10 years of life. It occurs with bilateral cervical, often generalized lymph node enlargement, fever, leukocytosis, erythema nodosum. According to our observations, if internal organs are damaged, the prognosis is poor. The prognosis worsens in the presence of simultaneous immunodysfunction (accelerated ESR, dysproteinemia).
- Leiner's desquamative erythroderma. Most likely, a defect in leukocyte chemotaxis and deficiency of the complement fragment C5. The disease manifests itself in the first 3 to 4 months of life. It manifests itself as a generalized enlargement of all lymph nodes, secondary erythroderma, nail dystrophy, anemia, vomiting, and diarrhea. More common during breastfeeding. Familial cases are known. The prognosis is favorable.
3. Granulomatosis
- sarcoidosis
- allergic granulomatosis Churg-Strauss. Combined with a history of atopy. Manifests itself in the form of bronchial asthma, severe eosinophilia, PAP, neuropathy, skin ulcers, damage to the heart, lungs, intestines and vasculitis of small arteries and veins.
- multicentric reticulohistiocytosis. Systemic granulomatous disease with the formation of skin nodules, destructive arthritis, and damage to internal organs. It proceeds according to the type of psoriatic arthropathy.
- Lipomelanotic reticulosis (Pautrier-Waringer syndrome) is a localized or generalized increase in lymph nodes as an accompaniment of dermatoses, primarily melanoerythroderma.
| Figure 3. Atypical histiocytes in the lymph node punctate with histiocytosis X. Romanovsky staining. X900 |
4. PAW for hemoblastoses.
- acute leukemia.
- non-Hodgkin's lymphomas.
- Hodgkin's lymphoma (according to the old terminology - lymphogranulomatosis).
- alpha heavy chain disease (Mediterranean lymphoma). Observed mainly in childhood and adolescence, the clinic is caused by severe malabsorption syndrome, which is the result of lymphoproliferative processes with infiltration of the small intestine and mesenteric paws.
- gamma heavy chain disease. It is caused by monoclonal gammopathy and occurs as a lymphoproliferative systemic disease.
- histiocytic syndromes
5. LAP in metastasis of solid tumors to lymph nodes.
6. Paraneoplastic reactions [12].
- POEMK complex. Paraneoplastic symptom complex (especially often with sclerosing plasmacytomas) = polyneuropathy + organomegaly + endocrinopathy + dysglobulinemia (M-gradient) + skin lesions.
7. PAP in primary immunodeficiency conditions (PID).
- common variable immune deficiency.
- autoimmune lymphoproliferative syndrome.
- granulomatosis septic. A heterogeneous group of immune defects, united by incomplete intracellular phagocytosis of catalase-positive microbes as a result of deficiency of hydrogen peroxide and atomic oxygen [11]. Currently, 4 different molecular defects are known: a) X-chromosome-linked recessive defect of cytochrome B558 heavy chains; b) autosomal recessively inherited defect of light chains of cytochrome B558; c) defect of 47 kd cytosol factor; d) defect of 65 kd cytosol factor. Clinical signs: acute abscess infections of the skin, lungs, gastrointestinal tract, lymph nodes, liver, spleen caused by catalase-positive bacteria (staphylococci, enterobacteria), as well as aspergillus; chronic granulomatous inflammation in the gastrointestinal tract and urinary tract with possible stenosis; decreased production of atomic oxygen and hydrogen peroxide in response to soluble and opsonized stimuli.
| Data from examination and palpation of lymph nodes must be confirmed and clarified by instrumental methods. First of all, non-invasive imaging methods used to study deep lymph nodes |
8. Genetically determined PAWS [9].
- Klippel-Trenaunay syndrome. Combination of local lymphangiomas and hemangiomas.
- syndromes with hereditary lymphedema. Wever-Smith and Milroy syndromes.
- pulmonary muscular hypertrophy - muscular cirrhosis of the lung. The proliferation of smooth muscle fibers is perialveolar, peribronchial, interstitial, interlobar. Enlarged lymph nodes at the hilum of the lungs. DD is carried out with sarcoidosis, tuberculosis, pulmonary emphysema, alveolar-capillary block syndromes. The diagnosis is verified only histologically.
9. Acquired immunodeficiency syndrome (AIDS).
In the process of diagnosing diseases that occur with an increase in lymph nodes, the efforts of pediatricians, infectious disease specialists, immunologists, and oncohematologists are combined. The main role in this case is given to the pediatrician, since most PAs and PAPs in children are associated with an infectious process. At the same time, one cannot insist on the infectious genesis of lymph node enlargement if a two-week course of antibiotic therapy did not lead to a significant improvement in the clinical, laboratory and instrumental picture. In favor of the oncohematological genesis of changes in lymph nodes is indicated by an increase in their diameter to 4 cm or more, stony density, tuberosity, formation of conglomerates of lymph nodes, their adhesion to surrounding tissues, intrathoracic conglomerates, especially in the upper mediastinum, intraperitoneal conglomerates.
A clear knowledge of the variety of causes of lymph node enlargement will help pediatricians in the diagnosis and differential diagnosis of this syndrome.
Literature
1. State report on the state of health of the population of the Russian Federation in 1994. M., 1995. p. 43. 2. Miller J. Tuberculosis in children and adolescents. M.: Medicine, 1984. p. 296. 3. Nazarenko O. R. Comparative value of echography in assessing the condition of the abdominal organs in children with acute lymphoblastic leukemia. Author's abstract. dis. ... Ph.D., M., 1997. p. 24. 4. Nikhamkin L. I. Local tumor-like amyloidosis of the mesentery. Archives of Pathology, 1966. 4. p. 76 - 78. 5. Samochatova E.V., Vladimirskaya E.B., Zhestkova N.M., Navolotsky A.V. et al. Hodgkin’s disease in children. M.: Altus. - 1997. 96. 6. Tarasova I. S. Clinical and hematological characteristics of children under various radiation dose loads. Author's abstract. dis. ... Ph.D. M., 1997. p. 25. 7. Chernov V.M., Finogenova N.A., Shakhtalin V.V., Sidorovich G.I. Structure of hematological morbidity of children in the city of Klintsy, Bryansk region. In the book: Medical aspects of the influence of low doses of radiation on the body of children and adolescents. Obninsk - Moscow, 1992. p. 92 - 95. 8. Dangman BC, Albanese BA, Kocia M. Cat scratch disease with fever of unknoun origin: imaging features and association with new causative agent Rochalimea henselae. Pediatrics, 1995. v. 5. p. 767 - 771. 9. Emery A., Rimoin D. Principles and practice of medical genetics. 1988. V. 1, 2. 10. Flexman J. Bortanella henselae is a causative agent of cat scratch disease in Australia. J. Infect., 1995. V. 31. No. 3. p. 241 - 245. 11. Leiber B. Die klinischen Syndrome. Muenchen, 1990, Bdd. 1.2. 12. Siegenthaler W. Differential diagnosis innerer Krankheiten. Stuttgard, 1993. s. 800.
Diagnostics
Laboratory tests will help determine the level of white blood cells in the blood
Lymph nodes in the parotid area and on the face become inflamed for various reasons. Therefore, first of all, it is necessary to find out the true factor that provoked the increase in the formation, which is located next to the ear area. An internist or an infectious disease specialist can examine an inflamed lymph node.
If you complain of pain and enlargement of the parotid lymph node, you should first contact a therapist. He must interview the patient and examine the affected area. Afterwards, if necessary, the therapist refers the person to a highly specialized specialist.
The results of the following diagnostic measures help to understand why the lymph nodes near the ears or near one ear are enlarged:
- Anamnesis collection. The doctor should study the symptoms of the disease in detail. Thanks to this, he will be able to make a diagnosis and exclude similar pathologies.
- External examination of the inflamed lymph node. Palpation is carried out, which allows you to determine the degree of inflammation and the presence of suppuration.
- Lab tests. Blood and urine samples are required. These tests help determine the level of leukocytes in the body and other important indicators.
- Instrumental diagnostics. The patient is given a referral for a fine-needle biopsy and ultrasound examination.
After the doctor receives the test results, he will be able to make a diagnosis for the patient. Based on this, a suitable treatment is selected for a person with an inflamed parotid lymph node.
What to do if the lymph node near the ear is inflamed?
Not everyone knows what to do if the lymph node near the ear suddenly becomes inflamed.
For lymphadenitis and other diseases that lead to an increase in the formation of the lymphatic system, it is strongly recommended to refrain from self-medication.
To relieve painful symptoms and reduce the size of the parotid lymph node to normal, full treatment is required. It must be prescribed by the attending physician.
Drug therapy
Therapy designed to treat inflammation of the lymph nodes in the ears (in the area of the hearing organs) involves the use of medications. Treatment is based on the following medications:
- Antibiotics (Azithromycin, Amoxicillin, Biseptol). The lymph nodes in the parotid area begin to ache when the body is susceptible to an infectious disease. Depending on the reasons for the development of the pathological process, the patient is prescribed drugs with antibacterial action,
- Painkillers (Ibuprofen, Paracetamol). They help cope with pain and other signs of illness that occur with inflammation of the lymph nodes.
- Antihistamines (Zyrtec, Telfast). They are prescribed to patients with inflamed lymph nodes. These drugs do not cause drowsiness or other unpleasant side effects.
Acute mumps
Mumps is an infectious disease caused by a filter virus. Most often occurs in childhood.
Symptoms of mumps
Often, in the prodromal period, the first symptom of mumps is stomatitis. Then there is swelling of the gland, pain, protruding earlobe, decreased salivation, temperature up to 39 C. Fever lasts 5-7 days.
The patient may complain of increased pain when chewing, opening the mouth, and dry mouth. In the oral cavity, you can see swelling and hyperemia of the mucous membrane of the pharynx and around the opening of the excretory duct. The swelling of the gland lasts for 2-4 weeks.
Acute mumps can be accompanied by damage to the nervous system (meningitis, meningoencephalitis, neuritis), the digestive system (dyspepsia), the cardiovascular system (pain in the heart, shortness of breath), the organs of vision, and hearing.
Differential diagnosis of mumps
Differential diagnosis of mumps is carried out with false mumps, parenchymal mumps, and Mikulicz's disease.
False parotitis is a unilateral acute serous lymphadenitis of the intraglandular lymph nodes of the parotid region. Develops as a complication of difficult eruption of third molars. With this disease, salivation remains normal.
Parenchymal parotitis is characterized by a long chronic course with periods of exacerbation.
With Mikulicz's disease, all salivary and lacrimal glands are affected.
Treatment of mumps
Treatment of mumps is aimed at eliminating symptoms and preventing complications, since there is currently no specific therapy. Patients are prescribed bed rest for 7-15 days, pureed food, warm compresses, and rinsing the mouth with antiseptics. Antibiotics are prescribed for prophylactic purposes.
In case of suppuration, surgical treatment is performed. Incisions are made in the direction of the branches of the facial nerve, the skin and subcutaneous fat are dissected with a scalpel, and the capsule and gland are separated with a hemostatic clamp. The wound and excretory duct are washed with antibiotics.
Prevention of mumps
Prevention of mumps involves isolating the patient for the duration of the illness and 14 days after all symptoms disappear.
Vaccination with mumps-measles and mumps live vaccines is also carried out. Included in the mandatory vaccination calendar. Vaccination is carried out at 12 months and revaccination at 6 years.