Every third appeal to an oncologist on social networks or on remote consultation portals is formulated something like this: “save, help, I have enlarged lymph nodes.”
As a rule, young people write, usually from 18 to 25 years old, and I don’t remember a case when it eventually turned out that the situation required treatment from an oncologist. Most often, enlarged lymph nodes were caused by a sore tooth, sore throat, conjunctivitis, and so on.
It is clear that fear and fears for one’s health in such cases force one to immediately run to an oncologist.
However, is everything so simple, and is it worth rolling your eyes about any treatment with an enlarged lymph node?
My personal statistics show: if a person comes for a face-to-face consultation, he is already one of those few whose situation was not limited to the banal “it got sick and went away.”
Let's take a closer look at how the lymphatic system works and understand the nature of enlarged lymph nodes.
Fact #2
Lymphatic vessels are not something abstract.
It is worth crossing or ligating them, for example, during surgery on the axillary lymph nodes for breast cancer, and lymphostasis is likely to develop - swelling of the limb, which, again, most likely will not go away.
The most visible to us from the point of view of examination - the so-called peripheral lymph nodes (in the neck, supraclavicular, axillary and inguinal) can increase, and this is in most cases a manifestation of reactive lymphadenopathy - an inflammatory reaction indicating the fight against infection.
Erysipelas due to lymphedema
Erysipelas is a bacterial hypodermal cellulitis that is usually associated with streptococcal infection. Most often it is a complication of chronic lymphedema. The first signs are a sudden rise in temperature and chills. The clinical feature is an inflammatory dermatitis with clearly defined boundaries, which is often accompanied by fever. Inflammatory skin thickening contributes to lymph stagnation and the progression of lymphedema.
Erysipelas, as such, is mainly treated with antibiotics. Relapse prevention is an important goal. Because lymphedema is a major risk factor for recurrence, aggressive treatment is necessary.
Risk factors for erysipelas
The lymphatic system plays an important role in protecting the body from infection. Stagnation of lymph during lymphedema contributes to the penetration of infection into dilated lymphatic capillaries. Infectious complications are mainly bacterial, most often erysipelas (cellulitis), and sometimes lymphangitis (inflammation of the lymphatic vessels). The most common causative agent of erysipelas is β-hemolytic streptococcus (groups A, C, G). Bacterial complications are facilitated by the abundance of proteins characteristic of edema in lymphatic insufficiency associated with obstructed lymphatic drainage. This high protein content in the interstitial fluid provides an ideal breeding ground for bacterial growth.
Erysipelas is a dermo-hypodermal bacterial infection without involvement of the superficial aponeurosis. Erysipelas complicates lymphedema in 30% of cases and aggravates its course.
With lymphedema, chronic inflammation of the skin is very common; it may not be associated with infection, but only with stagnation of lymph. However, the presence of streptococcus in changed skin is always a risk factor for erysipelas. And the use of hormonal ointments on the skin of patients with lymphedema can provoke deep purulent-necrotic damage to the subcutaneous tissue and fascia.
Symptoms
Erysipelas often occurs suddenly, with pronounced systemic signs - fever >38 ° 5, chills and general malaise. Local signs develop within a few hours: redness, local fever, pain and rapid spread of the lesion, with centrifugal expansion over several days. Erysipelas can begin at any stage of lymphedema and can spread to all or part of the changed skin tissue.
Diagnosis
The diagnosis of erysipelas is established clinically:
The sudden onset of an inflammatory lesion that spreads over several days, preceded or accompanied by fever and chills, as well as general malaise.
Streptococcus is isolated only from 4% to 35% of cases in patients with erysipelas. If the most sophisticated methods are used (immunofluorescence, polymerase chain reaction), then streptococcus is isolated with a frequency of 70% to 80%.
Differential diagnosis
Erysipelas must be differentiated from other infections sometimes seen with lymphedema, such as lymphangitis, most often streptococcal (less commonly staphylococcal) or necrotizing fasciitis (most often streptococcal).
Lymphangitis is characterized by the appearance of an inflammatory streak (red, hot and painful) along the superficial lymphatic vessels (which themselves are satellites of the superficial venous system). Accompanied by fever. There is no spread of the lesion into deep tissues.
Other acute forms of dermo-hypodermal bacterial infections are caused by Erysipelotrix rhusiopathiae (swine erysipelas), the bacterium pasteurella multocida, and borrelia borgdorferi. They have a less inflammatory and febrile clinical presentation without the typical chronology of erysipelas.
Thus, the diagnosis of erysipelas is purely clinical in nature and does not require any laboratory tests, in particular bacteriological ones.
Treatment
Antibacterial treatment is carried out with amoxicillin tablets (3-4.5 g/day, in 3 doses) for two weeks.
Hospitalization is necessary if:
- There is doubt about the diagnosis, or there are serious systemic features, comorbidities, or a social context that makes home treatment impossible for the patient.
- Fever persists for more than 72 hours. In such cases, treatment is carried out with intravenous penicillin g (10-20 million units in 4-6 infusions per day).
Relapse Prevention
Erysipelas with lymphedema often recurs and aggravates its course. To avoid recurrence of erysipelas, treatment is carried out with long-acting penicillins. (Extencillin or Retarpen 1 gram per week for 4 weeks during a possible exacerbation).
Treatment of lymphedema using conservative and surgical methods, maintaining the disease without progression helps reduce the likelihood of relapses of erysipelas.
Fact #3
Most often, the cervical and submandibular lymph nodes become inflamed, because in the facial part of the skull there are many open mucous membranes and associated infections.
A sore throat, carious or rotten teeth, and ear and eye bacterial and viral infections are the most common causes of cervical lymphadenopathy. The axillary and inguinal nodes react according to the same principle.
Therefore, if a lymph node is bothering you, first of all you need to go to a therapist, dentist, or ENT doctor.
If the genesis of lymphadenopathy is unclear, the doctor will prescribe an ultrasound, and during this study, attention will be directed mainly not to the size of the lymph node, but to its shape and differentiation of the structure.
Causes of inflammation of the cervical lymph nodes
There are many factors that can trigger the appearance of inflammation in the body. There are several groups of lymph nodes in the neck area: superficial and deep. The action of the former is aimed at protecting the external integument, while the latter prevents the penetration of infection into the internal organs. Bacterial or viral infection of the pharynx, larynx, trachea, upper esophagus, as well as the oral cavity, nose and ear are the most common causes of inflammation of the cervical lymph nodes.
They can call him:
Fact #5
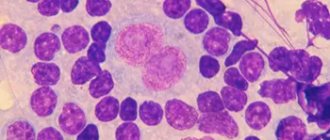
Lymph nodes enlarge during cancer because cancer cells enter the lymphatic vessels draining a certain area, which then settle in the “filters” (lymph nodes) in the form of metastases and begin to grow there.
Such lymph nodes do not shrink after treatment of infectious diseases, but only increase, merging with other lymph nodes into conglomerates, extending beyond the lymph node and fixing it in the surrounding tissues. Such lymph nodes are rarely painful, they are dense, very dense.
Often in cancer, lymph nodes are affected by a “chain” that is clearly visible on palpation. With lymphomas, conglomerates are often visible from the outside. Of course, with such manifestations you need to go to an oncologist and hematologist.
For suspicious nodes, a biopsy will be performed in the absence of other causes. This is either a puncture with a needle and collection of material, or an operation to completely remove the lymph node for histological examination.
PHYSICAL EXERCISE FOR LYMPHOEDEMA
Special exercises will help improve lymphatic drainage, prevent fibrosis, increase the tightening effect, expand the range of motion of swollen limbs, and help prevent stiffness of the joints. Patients should be encouraged to move the swollen limb as often as possible because muscle contraction stimulates both lymph flow and blood circulation. Walking is an excellent exercise. If it is impossible to perform active movements, then the patient should perform passive physical exercises at least twice a day.
It must be remembered that too vigorous, strenuous exercise can sometimes be harmful, as it causes dilation of blood vessels and increases lymph flow. Patients with swollen feet should not sit or stand for long periods of time. Activities such as moving heavy objects should be avoided as they reduce blood and lymph flow.
The arms should not be raised at an angle of more than 90 degrees, as this position reduces the space between the collarbone and the first rib and impairs blood circulation, which can lead to increased swelling.
Continuous use of arm support wraps should be avoided as this may cause stiffening of the shoulder and elbow joints. A wide arm support bandage can be used while the patient is walking, but should be removed when the patient is resting (the arm can be placed on a pillow). The sling can also be used to support a paralyzed arm, to prevent subluxation or dislocation of the shoulder joint, or when the back muscles are severely weakened.
What to do if your lymph nodes hurt?
Treatment of lymph nodes depends entirely on the causes of inflammation. In order not to “overlook” the disease, it is enough to be attentive during a visual examination. With inflammation, the lymph nodes enlarge - the familiar, for example, submandibular relief becomes smoother. There are about a hundred diseases associated with this condition, so self-diagnosis is a bad idea. A much better decision would be to contact a therapist: he will be able to conduct a comprehensive examination, after which he will refer you to a specialist, depending on the nature of the inflammation.
Characteristic symptoms of the course of inflammation are also a change in the consistency of the lymph node (it can become soft from suppuration, or hard due to the development of cancer cells of the lymph tissue), the occurrence of painful sensations during palpation or swallowing, redness of the skin at the site of the lesion, as well as apathy and fatigue characteristic of many diseases , headaches and fever, which is inevitable during inflammation.
If the lymph nodes in the neck hurt from a sore throat or any other disease in which such sensations are only a symptom, then the pain will go away along with the end of the underlying disease. Mild symptoms (mild pain or tingling when swallowing or pressing, general weakness and frequent colds) indicate a general deterioration of the immune system.
In the second case, the most common treatment method is ultra-high frequency therapy - a painless and discomfort-free procedure performed using special equipment. Antibiotics and anti-inflammatory drugs can be prescribed by a doctor in case of urgent need, but in general it is enough to adhere to bed rest, take vitamins and drink plenty of warm fluids. Echinacea tincture will help ease the course of the disease - a truly magical plant, a natural antiseptic that eliminates inflammation and strengthens the immune system. Decoctions of mint, chamomile or calendula will help you feel better, and rinsing with salt and soda will help fight inflammation.
Remember that inflamed lymph nodes should under no circumstances be heated, rubbed, or an iodine mesh applied to this area. Such procedures aggravate the course of the disease and accelerate the spread of infection.