Flux is a common, non-medical name for a whole group of diseases that require immediate, and in some cases, emergency care. One of the main manifestations of flux is a violation of the shape of the face associated with a complication in an inflamed tooth.
The main groups of diseases that are commonly called flux: periodontitis, periostitis, osteomyelitis, abscess and phlegmon, lymphadenitis, odontogenic sinusitis.
Periodontitis
- inflammation of the tissues of the apical part of the tooth.
Periostitis
– inflammation of the periosteum in the area of the teeth.
Osteomyelitis
– inflammation of the jaw bone, which necessarily ends with necrosis (death) of the affected area of the bone.
Abscess
- This is a limited purulent inflammation of fatty tissue.
Phlegmon
- This is a diffuse purulent inflammation of fatty tissue.
Under the skin, under the mucous membrane, under and between the muscles there is fatty tissue. With an exacerbation of odontogenic infection, pus spreads under the periosteum, axillary and intermuscular spaces, causing inflammatory and edematous-infiltrative changes in the soft tissues of the face and neck.
Inflammatory diseases of the maxillofacial area (flux, abscess, phlegmon) and neck are divided into two main groups according to localization. The first is abscesses and phlegmons located near the upper jaw. The second is abscesses and phlegmons located near the lower jaw.
Lymphadenitis
– inflammation of the lymph node (group of lymph nodes) adjacent to the odontogenic (dental) focus of infection. Odontogenic sinusitis is often an inflammation of the maxillary (maxillary) sinus (sinusitis), caused by the anatomical features of the position of the roots of the maxillary teeth involved in the pathological process, in which the roots of the teeth either stand in the lumen of the maxillary sinus, or are located close to the bottom of the maxillary sinus. In this case, infection of the mucous membrane of the maxillary sinus occurs with the subsequent development of sinusitis.
Content:
- Possible reasons
- Dental causes of inflammation of the lymph nodes on the chin
- How to understand that the problem is in the lymph nodes
- Diagnostic measures
- How are lymph nodes treated?
- Preventive measures
If the lymph nodes are inflamed, it is important to undergo a comprehensive medical examination.
This condition can be accompanied by many diseases, both related to the field of dentistry and not related to it. Lymph nodes are peripheral organs of the lymphatic system. They perform the functions of a biological filter. Passing through their tissues, lymph enters different parts of the body and internal organs.
If the lymphoid structure has increased, it means there is an inflammatory process. It is necessary to find out as soon as possible what functional disorders it is associated with. This will allow you to create an effective treatment plan and prevent the development of severe complications.
Hygroma of the finger
The appearance of a finger hygroma is a tumor-like formation (similar to a lump) localized on the finger, in the area of one of the joints (in some cases, multiple). Often the formation reaches 2-3 centimeters in a few days.
Often, hygroma of the finger looks like an ordinary wart, and only a doctor can accurately determine the pathology during examination.
A hygroma on a finger (a photo of which can be found on the Internet) can spontaneously open and, at first glance, disappear from the finger. But, as a rule, after some time the tumor appears again, since the capsule of the formation itself does not disappear anywhere, but continues to produce fluid and be filled with it. In addition, this can provoke the appearance of one more or even several hygromas on the finger (photo).
Of course, hygroma is not life-threatening, but painful and unpleasant sensations can affect the quality of life for the worse.
Possible reasons
The lymphatic system is the basis of immunity . It prevents the spread of pathological microorganisms and blocks the occurrence of many disease processes. In various diseases, lymphocytes begin to actively multiply to slow down inflammation. Then the lymph nodes enlarge.
If structures localized under the jaw and in the neck area “grow,” it is most likely an infection, that is, the disorder is caused by bacteria. But sometimes the condition occurs in the absence of infection.
Among the most common infectious causes:
- Colds, viruses. Their pathogens affect the ENT organs, and general intoxication is observed. In this scenario, sore throats, pharyngitis, tonsillitis, acute respiratory viral infections, acute respiratory infections, sinusitis, otitis media, etc. occur.
- Tuberculosis. With lymphadenitis, the entire neck swells. In advanced cases, lymphoid tissues located in the abdominal cavity and chest increase. The pathology is treated conservatively and surgically.
- Dental problems. Pulpitis, caries, periodontitis - all these are provoking diseases.
- Toxoplasmosis. People become infected with it from domestic animals (most often from cats). In addition to the growth of nodes, with this diagnosis the following are observed: high body temperature, headaches, an increase in the size of the spleen and liver. But very often the disease is asymptomatic.
- Venereal pathologies. Transmitted sexually. The body reacts very sharply to most of them, so already in the first days the patient notices that the lymph nodes have become enlarged and began to hurt, and severe weakness has appeared.
- Herpes. It manifests itself as an increase in the volume of lymphoid tissue in the neck, under the jaw and in the groin. Requires competent antiviral therapy.
Among the factors of a non-infectious nature that lead to the appearance of an unfavorable symptom:
- Oncology. It does not matter whether cancer of the lymphatic system or any internal organ is diagnosed. But in the first case, cancer cells quickly spread with the lymph flow, which contributes to the formation of metastases.
- Autoimmune pathologies. These are conditions in which the immune system begins to malfunction, causing serious damage to the body. This group includes systemic lupus, rheumatoid arthritis, type 1 diabetes, etc.
- Allergy. It manifests itself differently in all people. The most common symptoms are skin rashes and itching. But lymph can also be involved in the allergic process.
- Traumatic injuries to the head and face. If a strong pathological process occurs, lymphocytes begin to be actively produced.
Treatment
Treatment for flux can be boiled down to a catchphrase in Latin: “Ubi pus, ibi incision,” which translates as “Where there is pus, there is an incision.” Treatment of flux begins with eliminating the cause that caused the flux. That is, from the removal of the causative tooth. Next, they begin to drain (empty) the purulent focus by opening (incision) in the area of the flux. The abscess is emptied, the abscess cavity is washed with antiseptic solutions, and drainage is installed through which pus will be released. Regardless of the type of flux, the principle of treatment remains the same: opening the lesion, drainage.
In the postoperative period, daily antiseptic treatment (washing) with antiseptic solutions is carried out. There is a peculiarity in the treatment of these diseases (flux, periostitis, phlegmon, etc.), which is that immediately after surgery and up to 1-2 days, facial swelling (flux) may increase. This should not be taken as a worsening of the disease. The fact is that any surgical intervention is perceived by the body as an injury, and the body responds to this by increasing tissue swelling in the area of injury. This may be accompanied by increased swelling of the eyelids, cheeks, etc. Painful sensations decrease and subsequently decline as acute inflammatory phenomena subside. As a rule, antibacterial drugs, antihistamines and painkillers are prescribed after surgery.
If there is an advanced case of flux, which is accompanied by a violation of the function of external respiration (the patient may suffocate), then hormonal drugs are prescribed, and even an operation is performed - a tracheotomy. The operation consists of making an incision in the area of the tracheal rings and installing a tube. As the swelling of the upper respiratory tract (pharynx, larynx) decreases, when the threat of asphyxia (suffocation) has passed, the tube is removed from the trachea, and the patient breathes through the natural airways. The duration of prescription of drugs is determined by the attending physician. The drainage in the wound is periodically changed, and the wound is removed when cleansed. The duration of drainage in the wound is also determined by the attending physician, based on the clinical picture of the disease. The drainage can remain in the wound for an average of 3 to 10 days.
If the incision for flux was made through the oral mucosa, then additional suturing of the wound is not required in the future. The wound in the oral cavity will heal on its own (by secondary intention). If the incisions were on the skin side, then after the acute inflammatory processes have subsided, the wound can be sutured. After suturing the wound (and this can be 2-4 weeks after surgery), the patient is also prescribed antibacterial drugs and painkillers, and the wound is drained.
With inadequate treatment, as well as in advanced cases of flux, complications such as suffocation, penetration of infection into the cranial cavity, onto the membranes of the brain, into the neck and into the mediastinum (part of the chest cavity where vital organs are located), penetration into the orbital cavity with damage to the optic nerve and the occurrence of a systemic inflammatory reaction (sepsis), which leads to multiple organ failure and even death.
Soft tissue incisions, which are used in the surgical treatment of flux, must ensure complete sanitation of the purulent focus and adequate drainage. Surgical treatment should not be replaced by the prescription of strong antibacterial drugs. Waiting tactics, delays in performing surgery, and small incisions that do not provide adequate drainage of the purulent focus are unacceptable. We must not forget that surgery for a purulent process in the maxillofacial area and neck is often an operation to save the patient’s life. The occurrence of complications is more likely when the patient has concomitant chronic diseases: diabetes mellitus, coronary heart disease, anemia, diabetes mellitus and others. Elderly and senile age are also factors that can aggravate the course of this disease.
Dental causes of inflammation of the lymph nodes on the chin
Since very often in their work dentists are faced with huge lymph nodes in patients, let us dwell in more detail on the diseases that cause this symptom:
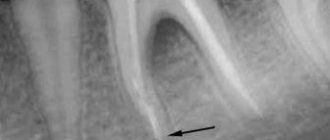
- Periodontitis. It can occur in acute or chronic form. Leads to tooth loosening and severe pain. If you do not receive qualified dental care in time, there will be a need to remove the affected unit.
- Stomatitis. Causes painful ulcers to appear on the mucous membranes of the mouth. It is the result of injuries, low immunity, vitamin deficiency. In advanced cases, the entire oral cavity becomes covered with wounds. Then active production of lymphocytes is observed.
- Pulpitis. Inflammatory lesion of pulp tissues. A very insidious disease. Through the pulp, pathogenic microorganisms penetrate into the lymph nodes and other tissues. It is important to clean the canals and seal them as soon as possible.
- Advanced caries. Despite the fact that many people do not take caries seriously, it is a rather insidious infectious process. If the deep tissues of the tooth are damaged, the lymph nodes come to the aid of the body - they try to neutralize pathological agents by producing lymphocytes. This can be understood by their increased size.
- Periodontal disease. Causes hypertrophy of periodontal tissues, leading to local hypoxia. Periodontal disease does not cause pain, so most often the patient learns about it by chance during a medical examination for some other condition. With periodontal disease, the gums become lighter, the interdental papillae atrophy, and the dental necks become exposed. If treatment is not started in time, the teeth will begin to loosen and fall out.
- Periodontitis. A disease that develops due to metabolic disorders, neurosomatic abnormalities, poor oral hygiene, and deficiency of vitamins and minerals. It manifests itself as bleeding gums, bad breath, and loose teeth.
- Gingivitis. Inflammatory reaction in the gums. Appears against the background of gastrointestinal pathologies, allergies, infections. The patient experiences bleeding gums even with minor mechanical stress. A burning sensation in the mouth bothers me. Ulcerative-necrotic areas may form.
These are not all dental conditions in which the lymph nodes under the chin become inflamed. In medical practice there are many more such diagnoses. This once again proves that the patient himself will not be able to understand why his submandibular area is swollen.
Types of hygroma
There are different types of hand hygromas:
Mucous cysts - hygromas occur against the background of deforming arthrosis of the joints. Most often they form at the distal interphalangeal joint - in this case, hygroma occurs in the area of the nail phalanx, at the base of the nail. Hygroma on the finger develops when osteophytes, present in deforming arthrosis, begin to irritate the skin, underlying tissues and capsular ligamentous apparatus. Because of this, a hygroma occurs - a formation that is hollow inside, in a transparent capsule, with transparent, jelly-like contents.
When a hygroma appears on the nail phalanx, it begins to put pressure on the growth zone of the nail and deform it.
Treatment of hand hygroma
Treatment boils down to excision of the cyst. Due to the fact that with mucosal cysts the skin over the lump on the hand becomes weak, the formation is excised along with the changed skin. After the operation, plastic surgery is performed - both with free skin grafts and with complex skin reconstructions.
A tendon ganglion is a cyst that is formed from the tendon sheaths and the walls of the tendon sheaths. Such hygroma of the hand can cause not only pain, but also limitation of motor functions.
Treatment of a tendon ganglion involves removing the formation - this does not pose any technical difficulty. After operations there are practically no relapses or side effects.
Synovial cysts in the area of the wrist joint (hand hygroma) are the most common type of hygroma.
How to understand that the problem is in the lymph nodes
Among the symptoms indicating damage to the lymph nodes:
- pain in the area where they are located;
- migraine;
- weakness;
- increased body temperature;
- discomfort under the chin;
- unpleasant pulsation in the lower jaw;
- difficulty chewing food;
- swelling noticeable to the naked eye.
If a purulent process develops, the skin in the area of inflammation becomes red and becomes very hot to the touch. Additionally, symptoms characteristic of the disease that provoked the disorder may appear.
Hygroma of the wrist joint
Most often, wrist hygroma occurs on the dorsum of the joint and looks like an ordinary lump on the hand - round and tumor-like. Hygroma is inactive, painless, dense, elastic consistency, with unchanged skin. According to statistics, almost 70% of hygromas are formed on the back of the wrist.
If the hygroma occurs on the dorsum of the hand, then it is clearly visible when the joint is flexed.
Much less commonly, wrist hygroma develops on the palmar surface of the wrist joint, in the area of the radial artery (in the place where the pulse is usually checked). This arrangement makes the surgical procedure very difficult.
Treatment of hygroma on the wrist
Treatment of such a hygroma is very difficult, since you have to very carefully isolate the cyst in the area of the radial artery, trying not to damage it. Carelessness during surgery can result in serious injury to the artery, which can disrupt the blood supply to the hand. Hygroma on the wrist requires the most professional and careful treatment, so only an experienced surgeon can perform a correct and effective operation.
Diagnostic measures
Detecting the problem is very simple - the doctor just needs to feel the area under the chin and carefully examine it. To establish the exact cause of the disease, you need:
- Take blood and urine tests. From them you can understand the nature of the “provocateur” (viral or bacterial).
- Donate blood biochemistry.
- Get an ultrasound of the lymph nodes.
If the doctor suspects oncology, the patient is referred for a computed tomography or magnetic resonance imaging scan or a puncture biopsy. These diagnostic measures allow you to make a correct diagnosis and select adequate treatment.
The structure of the wrist joint
The wrist joint is very complex in its structure and this is largely due to its versatility. In order for us to make various movements of the wrist, various types of bones are “assembled” in the joint (radius, ulna, metacarpal bones, carpal bones, cartilaginous articular disc), connected by ligaments designed to ensure the strength of the joint. It is the ligaments that allow the wrist and hand to move, rotate and rotate in all directions. All these elements, merging in one place, form the capsule of the wrist joint, in the cavity of which there is synovial fluid.
Hygroma, “growing” in the wrist joint, gradually increases in volume, “pushes apart” the surrounding tissues and ligaments and, ultimately, protrudes from the back or palmar side of the wrist, resembling a moving ball in appearance.
How are lymph nodes treated?
The treatment tactics chosen by the doctor directly depend on the characteristics of the clinical symptoms and the diagnosis. If it's all about a bacterial infection, you can't do without antibiotics. For viruses, antiviral drugs and immunostimulants are indicated. In the case of an autoimmune disorder, the focus is on reducing the activity of specific culprit markers. If cancer is confirmed, chemotherapy, surgery, and immunomodulators are necessary.
If the lymph nodes are enlarged due to a certain dental disease, its step-by-step treatment is carried out. Almost immediately after this, the problem of increased lymphocyte production disappears by itself.
It is extremely important that the patient does not warm the lymph node or apply any compresses unless the doctor has prescribed it. Such actions can aggravate the situation and lead to the development of health-threatening complications.
Classification of lymph node cancer
If there is any inflammatory or infectious process in the body, the lymph nodes react to it with enlargement and sometimes even pain. If this condition does not go away for a long time, then this is a reason to consult a doctor, since it is important to detect the pathology at an early stage.
Lymph node cancer can develop in one of two forms:
- Hodgkin's lymphoma (lymphogranulomatosis). The most common variant of the development of lymph node cancer, occurs in 1/3 of cases of detection of such oncology in both adults and children. Hodgkin's lymphoma is considered a more favorable form in terms of cure. Even at stage 4 of the disease, the survival rate is 65%;
- non-Hodgkin's lymphoma. This is a more serious form of lymph node cancer, occurring in 2/3 of cases. The disease progresses rapidly, metastases appear early and spread throughout the body.
Preventive measures
No one is immune from the problem described. But there are ways to minimize the risk of its occurrence. Among them:
- receiving qualified medical care for any ailments;
- annual laboratory tests;
- timely treatment of emerging dental diseases;
- sanitation of the oral cavity every six months;
- following medical prescriptions.
Take care of your health, and the risk of enlarged lymph nodes will be minimized.
Causes and risk factors
Lymph node cancer has several age peaks during which the disease is diagnosed more often. This is the period from 15 to 30 years, people over 50 are also at risk. It is during this time that the risk of developing lymphoma is higher. The exact causes of the disease are unknown. Doctors cite only risk factors that increase the likelihood of developing lymphoma:
- prolonged interaction with harmful substances;
- HIV infection and other types of immunodeficiency;
- smoking and alcohol abuse;
- radiation exposure;
- living in unfavorable environmental conditions;
- pregnancy over 35 years of age;
- Epstein-Bar virus;
- genetic inheritance.
Stages
Different types of lymphomas can have different degrees of spread throughout the body. Taking this into account, there are 4 stages of lymph node cancer.
- First. Only one area is affected; cancer develops in the lymph nodes in the armpit, neck, etc.
- Second. The tumor process has already spread to 2 or more groups of lymph nodes.
- Third. In addition to the lymph nodes, the diaphragm and one organ outside the lymphatic system are affected.
- Fourth. At the last stage, tissues outside the lymphatic system are affected, and in several parts of the body at once. The disease invades vital organs, so treatment becomes less effective.
When to see a doctor
Lymph node cancer requires timely detection at the earliest stage, since the prognosis of recovery depends on this. If you have risk factors or symptoms of the disease, you should immediately consult a doctor for appropriate diagnostic measures. In the case of cancer of the lymphatic system, the patient requires the help of an oncologist. In our oncology center on 2nd Tverskoy-Yamsky lane. House 10 employs the best specialists who specialize in the diagnosis and treatment of various types of oncology.