The hemostatic sponge is an important tool in the home and travel first aid kit and the best assistant to the surgeon. When used, it is possible to quickly stop bleeding. Today, hemostatic sponges come in a huge variety. They can be easily selected in size depending on the conditions of use.
Features of wound healing after tooth extraction
Before moving directly to hemostatic sponges, what they consist of and how to use them, you need to understand how the wound heals after removal and what can go wrong here. More on this later.
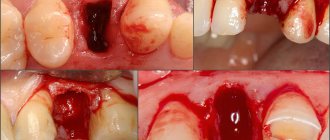
Why is there bleeding after removal?
Bleeding is a natural reaction to surgery. After all, when a tooth is removed, the smallest capillaries that penetrate the gums and ligamentous apparatus - the periodontium, which attaches the roots to the bone socket - are torn. And with difficult removal, the bleeding may be even stronger, because... The dentist makes incisions in the gums and drills into the jaw bone - the tissue is more damaged.
Bleeding is a natural reaction to surgery
Read on the topic: How long can a tooth hurt after extraction - normal and pathological.
How long does bleeding last normally?
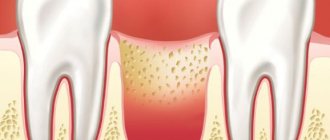
Normally, the blood stops within 15-20 minutes (less often, within 45 minutes) and a blood clot forms in the socket. It seals the hole like a cork, preventing germs from penetrating inside. If the patient has problems that affect blood clotting, then the bleeding time is prolonged, and a clot may not form at all. And this is already fraught with inflammation of the bone socket (the pathology is called “alveolitis”). Therefore, according to indications, the dentist applies a hemostatic drug to the area of the extracted tooth.
On a note! Bleeding may appear again for a short time (and there will be quite a bit of blood) after the anesthetic wears off - if it contained adrenaline. This substance narrows the blood vessels in the intervention area, and as they expand normally, slight bleeding occurs. It goes away quickly.
Why does the bleeding not stop for a long time?
As a rule, after tooth extraction, the dentist says that you should not eat or drink for 2 hours. But few people say that you should not rinse your mouth or suck drinks out of a straw. In the first days, only oral baths are allowed, and it is better to drink in the usual way. Also, do not touch the wound with a brush. It is better to chew food on the healthy “side” of the jaw. Otherwise, there is a risk of moving or “pulling” the clot out of the hole - which will provoke new bleeding or even inflammation, which will result in long-term treatment.
The following groups of patients are also at risk:
- who has not formed a blood clot,
- with blood diseases,
- who takes blood clotting medications,
- having high blood pressure,
- women during menstruation or menopause,
- exposing themselves to physical activity immediately after removal and during the recovery process,
- if there was already inflammation at the extraction site (for example, pericoronitis above a wisdom tooth),
- during complex operations: when several teeth were removed at the same time, or manipulations were performed with increased tissue trauma.
Bleeding may occur during physical exertion after removal.
When you need urgent help
If the bleeding is profuse and does not stop for a long time, if after normalization of the condition the blood begins to ooze heavily again, this is a reason to consult a dentist. In a situation where the patient, in the presence of continuous bleeding, feels weakness, apathy, if the temperature has risen sharply (above 39 degrees Celsius), it is better to call an ambulance or go to the hospital on your own.
What is a hemostatic sponge
Now let's move on to why a hemostatic sponge is placed in the hole left after tooth extraction? Let's first understand the terminology. “Hemo” means “blood” and “stasis” means stopping. Those. a hemostatic sponge is needed to stop bleeding. In simple terms, this is a kind of replacement for a blood clot. The hemostatic sponge in the tooth socket not only seals the open cavity, but also has a hemostatic effect. Firstly, it puts pressure on small vessels, stopping bleeding. Secondly, it absorbs excess blood, increasing several times. The bleeding stops within 2-3 minutes.
On a note! By the way, local hemostatic agents are used not only in dentistry, but also in other areas of medicine - for example, hemostatic bandages successfully replace tourniquets that are applied for bleeding.
What it is
A hemostatic sponge is a medical device made in the form of a compact block of porous natural material that looks like a sponge or sponge. A device is used to stop bleeding and accelerate tissue regeneration during surgery.
The product is used as a wound dressing, closing the cavity, keeping the hole sterile and stimulating the formation of a blood clot. Stopping bleeding occurs by absorbing excess blood and wetting the sponge. The sponge increases in size and compresses the walls of the hole, pinching the capillaries.
There are two types of devices:
- Cubes with dimensions 1x1x1 cm.
- Blocks (10x10x1 cm).
The required piece of sponge is cut from the block or cube using scissors or a scalpel. The final shape of the sponge is modeled taking into account the characteristics of the wound and needs.
Appearance and release form
The hemostatic sponge looks like a cube or plate, which looks like a small sponge or a piece of yellow or white foam rubber. Although in fact it consists mainly of natural collagen with various medicinal additives. The plate is quite soft and easy to cut, which allows the dentist to cut the desired size according to the shape of the hole.
The plate is quite soft and easy to cut
Manufacturers produce both small (1x1 centimeter) and large sponges (10x10 cm). The plates are tightly sealed in transparent bags, and the cubes are sealed in dark, opaque bottles. Hemostatic powders and gels are also produced. Absolutely all collagen hemostatics dissolve on their own in the wound over time.
Types of hemostatic sponges
According to the manufacturing method, hemostatic sponges for teeth are of the following types:
- from donor blood plasma - amben,
- from bones/tendons/blood of cattle - collagen and gelatin.
You need to understand that a hemostatic agent not only stops bleeding (due to aminocaproic acid, for example) and stimulates the formation of a blood clot, but also has an antiseptic effect. It can also accelerate regeneration and relieve inflammation. It all depends on the active components that make up the hemostatic sponge. The drug can be impregnated with the following substances:
- antiseptics: chlorhexidine, furatsilin, silver suspension, boric acid, iodoform,
- local anesthetics: for example, lidocaine,
- preparations for bone regeneration: calcium phosphate,
- antibiotics: metronidazole, chloramphenicol, neomycin, gentamicin, etc.,
- natural substances: propolis, eugenol, etc.
Hemostatic sponges for teeth come in different types
What is she?
So, a hemostatic sponge is an effective hemostatic agent, widely used in various medical fields, in particular, by dentists when removing teeth. The sponge has pronounced antiseptic and sorbing properties, and therefore not only stops bleeding, but also protects the wound from bacteria. In addition, thanks to the described remedy, damaged sockets heal faster.
Main types of hemostatic sponges
So, the described remedy is intended not only to stop bleeding, but also to prevent the occurrence of inflammatory processes if a complex surgical intervention was performed (for example, a wisdom tooth was removed). In standard cases of extraction, bleeding is stopped with the help of a collagen sponge that stops the bleeding.
After surgery, if there is a risk of inflammation in the tooth socket, dentists often recommend using “Alvostaz” - this is a special alveolar compress made in the form of a sponge. "Alvostaz" has an antiseptic and hemostatic effect, in addition, the drug is often used for the prevention/therapy of alveolitis.
About release forms
So, what is a hemostatic sponge? Essentially, it is a yellowish pressed powder that has a faint aroma of acetic acid. These sponges are sold in the form of small rectangular elastic plates (their sizes can be 5x5 cm and 9x9 cm) with a porous dry structure. During production, sponges are placed in PET bags, which are tightly closed, and then placed individually in cardboard packaging.
These sponges - just like regular sponges - perfectly absorb liquid, swelling at the same time. Sponges do not dissolve in cold water, as well as in substances of organic origin, but can partially dissolve in water whose temperature is more than 75 degrees. To make pressed plates, a collagen solution is used - it is obtained from the tendons/skin of cattle. There are also additional components - boric acid and nitrofural.
The above-mentioned “Alvostaz” is considered one of the most effective remedies. The product is sold in the form of small (dimensions - 1x1 cm) hemostatic sponges soaked in a special solution, packaged in plastic jars of 30 pieces. "Alvostaz" is produced in three versions; it contains propolis, eugenol, tricalcium phosphate, iodoform, lidocaine and thymol.
Effect of hemostatic sponges
The product described in the article is used locally (it is used to pack wounds) and has a wide spectrum of action, namely:
- stops bleeding;
- accelerates wound healing;
- protects the hole from bacterial infection;
- prevents swelling of gum tissue;
- stops the focus of the inflammatory process;
- eliminates painful sensations.
Note! The hemostatic sponge is effective for several hours after tooth extraction. After a certain time (indicated by the manufacturer), the sponge placed in the hole dissolves completely.
Manufacturers of hemostatic sponges
Popular manufacturers of hemostatic agents used by dentists in our country are domestic companies. Let's consider them further:
- Alvostaz compress from Omega-Dent: available in the form of cubes, flagella, powders and solutions. The compresses are numbered - “1” with iodoform, “2” with metronidazole and chlorhexidine, “3” with neomycin and chloramphenicol,
- "Gemasept" with gentamicin from the Russian Research Institute of Hematology and Transfusiology of the Federal Medical and Biological Agency",
- “Collagen hemostatic sponge” with silver and boric acid from “Zelenaya Dubrava”,
- “Hemostatic sponge” with furatsilin and boric acid from “Belkozin”.
Indications for use
A hemostatic sponge can be useful after tooth extraction, especially wisdom teeth. Because the “eights” often do not erupt completely, and the dentist has to perform a mini-operation to get to them and remove them along with the roots. When a tooth is removed, a hemostatic agent is placed 3-4 months before implantation to completely eliminate the possibility of complications and problems with the formation of new bone in the socket.
Also, hemostatic sponges or powders are used during operations on the gums1 - plastic surgery, curettage of gum pockets (removal of deep “deposits” of tartar), and when cutting off dead areas of the jaw bone due to osteomyelitis. In the latter case, bone blocks and materials for regeneration of bone substance are additionally planted. In general, the doctor always assesses the patient’s condition in advance - asks about diseases and other conditions, and about the medications taken. If there is a risk of bleeding or poor regeneration, then rest assured, a hemostatic sponge will definitely be placed in the hole.
These sponges are used for bone augmentation
It is important to know! A few days after tooth extraction, it may be necessary to apply a hemostatic sponge if the dentist sees a tendency to worsen. For example, a clot has fallen out or the gums/bone have become inflamed.
How to use the drug correctly
How to use the sponge? The hemostatic sponge is placed into the socket of the extracted tooth only by the dentist. Home use is not recommended due to the risk of infection deep into the tissues. The application procedure is given step by step below:
- tooth extraction or treatment of the hole a few days after removal: in the latter case, purulent masses are removed, irrigation is carried out with an antiseptic,
- a piece of the hemostatic plate is cut off with sterile scissors or a hemostatic cube is taken with tweezers,
- the drug is placed in the hole and pressed with a flat instrument: if the hemostatic agent is pre-saturated with thrombin, the hemostatic effect is enhanced,
- if necessary, an additional piece of hemostatic is applied,
- if necessary, a small tampon is placed on top of the hole (it will be removed the next day),
- suturing the gums - a seam in the shape of the letter “P”: also, if necessary, in most cases you can do without stitches.
A piece of the hemostatic plate is cut with sterile scissors.
Restoration of dental defects is inextricably linked with the use of dental implants. The basic principles of dental implantology that determine the future: achieving an optimal result with minimal trauma for the patient, reducing the duration of treatment, the number of stages, and the cost for the patient. Unfortunately, ideal conditions for installing a dental implant are quite rare. With the loss of chewing teeth of the upper jaw, there is an increase in pneumatization of the maxillary sinus, which leads to thinning of the bone tissue in this area [1, 2]. When the height of the alveolar process decreases in a number of clinical cases, a local increase in bone mass in the area of proposed implantation is necessary.
When analyzing defects in the dentition of the upper jaw, it was found that it is often impossible to do without a sinus lift. Sinus lifting is indicated in cases of insufficient bone tissue height when it is impossible to install a 10 mm dental implant. According to J. Rosenlight [3], generally accepted recommendations for the implementation of this technique are as follows: if there is 3 mm of bone tissue or less, an open sinus lift with implantation delayed for 6 months is indicated; if there is more than 3 mm of bone in height, an open sinus is indicated -lifting with immediate implantation, with a bone height of 5 mm or more - closed sinus lifting with immediate installation of dental implants. A separate group includes patients with teeth that need to be removed due to periodontal diseases, caries and its complications. In such cases, most clinicians take a wait-and-see approach after tooth extraction until the healing process of the sockets is completed. In our clinic, we have been studying the possibility of immediate implantation of extracted teeth into the sockets with a simultaneous sinus lift for many years. An analysis of the literature on the topic showed that in few cases the doctor decides to implant extracted teeth into the sockets in the presence of inflammatory processes in the tooth and to combine such an operation with an open sinus lift operation.
This study was made possible after a thorough analysis of the physiological processes occurring during blood clot reorganization and implant integration, as well as an analysis of the influence of the properties of the hemostatic sponge on the healing process.
It has already been proven that inflammation at the site of tissue damage triggers the mechanism of reparative regeneration and at the same time helps fight infection and eliminate dead tissue. Due to the increase in the permeability of the vascular wall in the area of inflammation, the migration of leukocytes, mainly neutrophils, begins. Studies have shown that the longer the neutrophilic stage of inflammation, the worse the regeneration process. When the macrophage stage prevails, normotypic regeneration occurs, ending with morphogenesis inherent in a particular tissue.
According to the latest data published in the Georgia Institute of Technology, Atlanta, the differentiation of mesenchymal cells into osteoblasts occurs on a microstructured titanium surface without the participation of exogenous factors and depends on the method of processing this surface, but this mechanism has not yet been studied well [7]. After implantation, the interaction of proteins, carbohydrates, fats, blood ions and serum with its surface occurs. Such interactions are determined by the chemical composition, surface energy and micro-nanotopography of the implant surface. Osteoblasts do not come into direct contact with the material, but interact with proteins absorbed by the surface through signaling proteins responsible for osteoblast differentiation. As a result of a series of parallel observations by R. Olivares-Navarrete, L. Postiglione [7, 8], it was established that the layer of absorbed proteins also affects the result of differentiation of progenitor cells. Differentiation into osteogenic cells directly depends on tissue oxygenation, i.e. on the degree of restoration of the microcirculatory network at the site of surgery. It should be noted that macrophages produce an angiogenic factor that stimulates vascular growth. The construction of new bone begins with the synthesis of collagen matrix by osteoblasts. Necessary organic and mineral substances enter the surgical area due to the rapid restoration of the microcirculatory network, the continuity of which is restored in the first 2 weeks. When creating an extracellular bone matrix, osteoblasts synthesize non-collagenous proteins, including bone growth factors - osteocalcin and osteonectin. The latter triggers the mineralization of the organic bone matrix, while osteocalcin stimulates the activation of osteoclasts at the final stage of reparative regeneration. As a result of the actions of osteoclasts, bone morphogenetic protein is released.
When analyzing recent publications on the topic of raising the floor of the maxillary sinus using osteoplastic materials, an increase in rehabilitation time after grafting of bone material was noted. In the bone plastic material there are no living cells - osteoblasts, there is no bone morphogenetic protein, which is why the material has neither osteogenic nor osteoinductive properties, but is precisely a frame, i.e. directly functions as an osteotransducer. The use of D. Sohn, J. Moon [5, 6] of a collagen hemostatic sponge during sinus lift in animal studies showed stable formation of bone tissue 5 months after surgery. The hemostatic collagen sponge, introduced into the cavity during sinus lift, performs several important functions. Firstly, it is a source of collagen, necessary for building bone tissue. Secondly, due to the porous structure of the sponge, its adhesion to the edges of the wound increases; The sponge stabilizes the blood clot in the cavity and induces the process of thrombus formation due to the calcium salts included in its composition, accelerating the processes of clot reorganization.
Material and methods
The study included 878 patients aged 18 to 72 years who were treated at the hospital of the Central Clinical Hospital named after. A.A. Vishnevsky in the period from 2004 to 2009. Patients with a complicated medical history were not excluded from the study. For the convenience of data analysis, patients were divided into 2 groups: group 1 included patients who underwent open sinus lift using a hemostatic sponge with simultaneous implantation, group 2 included patients who underwent open sinus lift using a hemostatic sponge with immediate implantation into the sockets of extracted teeth (see table).
Diagnostics.
The degree of atrophy of the alveolar process, the volume of the maxillary sinuses, and the degree of tooth destruction were determined clinically and radiologically, using orthopantomography data and targeted X-ray images. In cases of difficult diagnosis, computed tomography data was used.
Surgical technique.
Treatment was divided into 2 stages - surgical manipulations and orthopedic therapy.
The technique of surgical intervention can be considered in 2 clinical examples - open sinus lift using a hemostatic sponge and immediate implantation, and open sinus lift using a hemostatic sponge and immediate implantation into the sockets of extracted teeth.
Open sinus lift using a hemostatic sponge and immediate implantation into the sockets of extracted teeth (Fig. 1-8, Fig. 4-6, see color plate).
Figure 1. Orthopantomogram (OPTG) before treatment.
Figure 2. Initial situation in the oral cavity.
Figure 3. Incisions are made, the mucoperiosteal flap is detached; after removing 2.4, 2.7, access to the maxillary sinus was achieved.
Figure 4. After lifting the Schneiderian membrane, dental implants, Xive system, are installed. The cavity is filled with a hemostatic sponge and several granules of the Kollapan material are added.
Figure 5. Adapted PRP membrane.
Figure 6. Wound edges aligned. The wound is sutured with a continuous suture.
Figure 7. OPTG after surgery.
Figure 8. OPTG 5 months after surgery; formation of bone tissue in the area of surgical intervention is observed; during this time, dental implants were installed in the area of missing teeth in the lower jaw, and orthopedic structures were made.
Results and discussion
The study group consisted of 878 patients: 465 (53%) women and 413 (47%) men aged 18 to 72 years (average 44.3±2.1). Of these, 527 (group 1) underwent sinus lift operations using a hemostatic sponge with simultaneous implantation, and 2,371 dental implants were installed. 325 patients (2nd group) underwent sinus lift operations using a hemostatic sponge with simultaneous implantation into the sockets of extracted teeth, 1581 dental implants were installed (see table)
. The implant failure rate in both groups was 2%; it was observed in 17 patients of group 1 (47 implants) and in 11 patients of group 2 (32 implants). Both groups included patients of the older age category, people with a burdened medical history: diagnosed osteoporosis, diabetes mellitus types 1 and 2, chronic sinusitis. There was no statistically significant implant rejection in this group of patients. In the postoperative period, not a single patient complained of significant discomfort in the intervention area. Patients with a history of maxillary sinusitis complained of mild discomfort.
A combined technique was used to perform open sinus lifting operations using a hemostatic sponge with one-step installation of dental implants and open sinus lifting using a hemostatic sponge with one-step installation of dental implants in the sockets of extracted teeth. The goals of using this technique are to show the effectiveness of using a hemostatic sponge as a material that can replace osteoplastic allogeneic and xenogeneic materials, which are traditionally used during open sinus lift surgery, to reduce treatment time, and reduce its cost for the patient.
Based on the results of the study, it can be concluded that the hemostatic sponge used to raise the floor of the maxillary sinus can be recommended as a material replacing allogeneic and xenogeneic osteoplastic materials. Open sinus lift operations using a hemostatic sponge to lift the floor of the maxillary sinus with the simultaneous installation of dental implants both in the edentulous areas of the upper jaw and in the sockets of extracted teeth, followed by prosthetics, can be recommended as a safe and effective method for restoring dentition defects.
Is it necessary to remove the hemostatic agent?
Patients often wonder what to do with a hemostatic sponge after it has been placed in the socket of an extracted tooth? How long should I keep it on, and will it dissolve on its own? The rules of conduct are as follows: carefully but thoroughly observe oral hygiene, and also take medications prescribed by the dentist. There is no need to specially remove the hemostatic agent - after all, it consists of components that will completely dissolve during wound healing. And instead of a hemostatic agent, its own tissues form in the hole.
“When my wisdom tooth was removed, they stuffed it into the wound like a piece of foam rubber. I then saw the houses through the seams. I was also surprised - what is it? And at the next appointment, my dentist told me that this is a special sponge that absorbs blood and protects against infection. And when it resolved, I didn’t even notice)) It probably completely disappeared in a couple of weeks.”
Ekaterina R., review from irecommend.com
Recommendations
The collagen sponge should be removed from the packaging immediately before use. It is important to follow the rules of asepsis to prevent accidental infection in the wound. The hemostatic agent is carefully applied to the bleeding area and held for a couple of minutes. Deep wounds are tightly packed and then bandaged.
After the collagen sponge is saturated with blood, it will slightly increase in size. This will ensure that it adheres tightly to the damaged bleeding area. In cases where it is necessary to close damaged areas of parenchymal organs, a sponge of a suitable size is placed in the existing cavities. To stop bleeding, it is allowed to form several layers from it. After this, it is fixed using a U-shaped seam.
You can now buy a collagen hemostatic tube in pharmacies at an affordable price. It is presented by manufacturers in a wide range. You can also pick up the product in specialized online stores. Now you can use the booking service or order delivery of the product to the specified address.
Before using a collagen-based hemostatic sponge, you should carefully read the manufacturer's instructions. The product should be stored in a dry place where the temperature is maintained in the range of 10°C - 30°C. With high humidity, the sponge quickly becomes unusable. The shelf life of the product, subject to the required conditions, is 5 years.
Contraindications and side effects
The only contraindication to the use of a hemostatic sponge after tooth extraction is an individual allergy to any of the components of the drug. In particular, for antibiotics that are used to impregnate the hemostatic agent. Therefore, be sure to tell your dentist if you are allergic and to what medications. Hemostatic agents should also be used with extreme caution in children.
There are no side effects, because There are no toxic substances or components that affect perception in hemostatics. But if itching, inflammation, or swelling appears, feel free to contact your dentist. These manifestations can be caused either by a newly manifested allergy or by incipient complications - if, for example, the treatment was carried out poorly or the patient did not follow the doctor’s instructions.
1Skulean A. Periodontal regeneration, 2012.
Contraindications
The main contraindication to the use of collagen sponges to stop bleeding is hypersensitivity to any components used in their manufacture. In particular, this is intolerance to nitrofuran drugs. With increased sensitivity to them, severe allergic skin reactions are observed, accompanied by severe itching.
Collagen sponges should not be used to stop arterial bleeding. In this case, a tourniquet must be applied and the person must be urgently transported to a medical facility to provide qualified surgical care.
Contraindications to the use of collagen-based hemostatic sponges are skin lesions caused by pyogenic bacteria. In this case, the wound must be periodically treated with antiseptic agents to remove its purulent contents.