candidiasis in children is an infectious dental disease caused by fungal microflora (microorganisms belonging to the genus Candida). According to WHO statistics, manifestations of this pathology are observed in 5% of newborns and 10% of infants. Illness in pediatric dentistry can be chronic or acute. In this case, candidiasis can act as an independent dental pathology or be one of the signs of severe systemic diseases.
Reasons for the development of candidiasis
Sources of infection for candidiasis are previously infected individuals. In this case, the main routes of transmission of infection to a child are:
- intrauterine;
- aerosol;
- infection during childbirth when moving through the birth canal of mothers suffering from urogenital candidiasis;
- contact.
Factors contributing to the development of the disease are:
- violation of requirements regarding hygienic care of the child’s oral tissues and teeth;
- weakened immunity or the presence of severe disturbances in the functioning of the immune system;
- allergization of the body;
- gastrointestinal diseases;
- anomalies in the structure of the tongue;
- oral acidosis;
- deficiency of vitamin C, B vitamins;
- long-term treatment using antibacterial agents;
- the presence of severe systemic diseases;
- morphological and functional immaturity of epithelial tissues in the mouth;
- undergoing a course of therapy using hormone-containing drugs.
Cystitis in women
1 Diagnosis of cystitis in women
2 Diagnosis of cystitis in women
3 Diagnosis of cystitis in women
Cystitis in women is much more common than cystitis in men. We can say that this disease is more “female”. Among female urological diseases, cystitis is the undisputed leader. Almost every second woman has experienced all the “delights” of cystitis at least once in her life. Thanks to the short and wide urethra, infections from the female genital organs quickly reach the bladder. Cystitis in women quickly passes from acute to chronic form.
Women also often develop cystitis during pregnancy (when the growing uterus begins to put its weight on the bladder).
With cystitis, a woman’s quality of life deteriorates. She has to dress warmer so as not to “catch a cold”, refrain from intimacy with her loved one, and reduce her time in public places, at holidays and events due to inflammation of the bladder. The woman does not get enough sleep (since the urge to urinate continues both day and night), begins to feel worse, experiences psychological discomfort and looks tired.
Signs of the disease
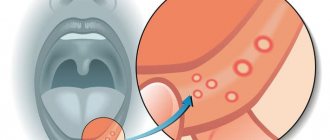
The key sign of the disease in childhood is the appearance of a whitish coating on the epithelial tissues, hiding eroded areas of tissue underneath. Lesions may appear on the tonsils, in the pharynx, on the tongue, in the corners of the mouth and on the edges of the lips.
In children with unformed speech, acute candidiasis can manifest itself in the form of refusal to eat, irritability, tearfulness, somnological disorders, and bleeding from the gums. Older children may complain of pain in the mouth when eating, itching and burning of epithelial tissue in the affected area.
The main signs of chronic candidiasis are:
- swelling of the epithelium;
- the appearance of light brown plaque on epithelial tissues;
- dryness, pain in the mouth;
- systematic bleeding from gum tissue.
Consequences of urethritis
If therapy is not started in time or the disease is not treated, then urethritis can become chronic. In addition, the inflammatory process can spread to neighboring organs, which leads to the following pathological conditions of the body:
- pyelonephritis (kidney inflammation);
- balanoposthitis (inflammation of the foreskin and head of the penis in boys);
- cystitis (inflammation of the bladder);
- prostatitis (inflammation of the prostate gland);
- orchitis (inflammation of the testicles);
- vulvitis (inflammation of the mucous membrane of the external reproductive organs in girls).
Chronic urethritis in adulthood can cause infertility.
Sources:
- Urinary tract infection in children: what a pediatrician and nephrologist needs to know. Zakharova I.N., Osmanov I.M., Mumladze E.B., Svintsitskaya V.I., Bekmurzaeva G.B. Medical Council No. 14, 2015. p. 114-118
- Pharmacotherapy of urinary tract infections in children. Korovina N.A., Zakharova I.N., Zaplatnikov A.L., Mumladze E.B., Goryaynova A.N. Guide for pediatricians, 2006.
- Diagnosis and treatment of urinary tract infections in children: what's new? Zakharova I.N., Machneva E.B., Mumladze E.B., Ivakhnenko Yu.I. Medical advice No. 1, 2021. p. 180-185
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Features of the treatment of candidiasis in children
The disease treatment program involves the use of antifungal agents and the adoption of measures aimed at comprehensively strengthening the body of the infected child. Until recently, nystatin was the drug of choice for this disease, but in modern dental practice more effective and harmless dental agents are used. Foods rich in carbohydrates (sweets, cookies, honey and others) must be excluded from the diet of a sick child.
There are a number of non-pharmacological methods to combat candidiasis in childhood. In particular, the following help to cope with the manifestations of this pathology:
- warm saline solution (used as a mouth rinse for children over three years old);
- lollipops with antiseptic components (prescribed for adolescents and children over 8 years old);
- solution of baking soda (used for systematic wetting of epithelial tissues of the mouth in infants and newborns).
When a disease is detected in breastfed babies, not only the babies, but also their mothers undergo treatment. This approach to therapy helps prevent re-infection of infants during feeding.
Diagnostics
At the first appointment, the urologist collects anamnesis, finds out what the patient is complaining about, and determines possible provoking factors. Next, the doctor conducts a physical examination, which includes palpation of the lower back, abdomen, and examination of the external opening of the urethra.
For a more accurate diagnosis of the disease, the following laboratory and instrumental research methods are used:
- Ultrasound of the kidneys and bladder . This is a basic diagnostic method. Using ultrasound, congenital abnormalities of the urinary system organs are diagnosed, which could lead to inflammation of the urethra. If the inflammatory process is strong, then on ultrasound you can see thickening of the urethral wall, but such data are not always informative.
- Urine tests . With inflammation of the urethra, the following laboratory symptoms are observed: sediment, turbidity, and a shift in pH to the alkaline side. To confirm the presence of inflammation in the urethra, a urine test according to Nechiporenko is prescribed. To establish the exact location of the source of inflammation, a three-glass test is indicated.
- Cystoureterography. It is usually prescribed to babies under one year of age with signs of chronic urethritis for differential diagnosis of vesicoureteral reflux. If the doctor suspects congenital malformations of the urinary system, excretory urography is additionally prescribed. Important! All diagnostic procedures must be performed strictly in the remission phase.
- Microbiological diagnostic methods . To determine the type of pathogen, urine culture, bacteriological and microscopic examination of smears from the urethra are carried out. To diagnose specific infections, PCR and ELISA studies are carried out. To correctly prescribe treatment, a test for antibiotic resistance is indicated.
Based on the clinical symptoms of urethritis in a child, data from laboratory and instrumental studies, the doctor prescribes a course of treatment.
Prevention of candidiasis in childhood
Measures aimed at preventing the occurrence and development of the disease in childhood include:
- limiting contacts between children and carriers of this disease in preschool educational institutions, schools, sections and clubs;
- maintaining the baby’s personal hygiene;
- competent organization of the process of feeding the baby;
- maintaining a healthy diet;
- inclusion in the child’s diet of foods rich in all essential vitamins;
- sterilization of bottles, pacifiers and nipples;
- systematic visits to the pediatric dentist to assess the state of oral health.
It is important to understand that self-medication for oral candidiasis not only does not promote recovery, but can also lead to consequences dangerous to the health and life of the baby. That is why, if any symptoms indicating the development of this disease are detected, it is necessary to contact a dental clinic as soon as possible and undergo a course of treatment according to a regimen drawn up by an experienced dentist.
Treatment of thrush
For the treatment of children, the principle of mandatory elimination (eradication) of the pathogen is applied. It should be remembered that first of all it is necessary to create conditions that are detrimental to the life of cells of the fungus of the genus Candida, and only then eliminate disorders of the vaginal microbiocenosis.
Stage 1: strengthening local and adaptive immunity in the child.
Oral administration of Bifidum BAG in age-specific dosages. Course 40 days.
Locally: for girls only applications on pads or napkins and baths! – 1-3 ml Bifidum BAG 1 time per day. Recommended course is 10-14 days. If necessary, the course can be extended to 28 days.
Stage 2: following a diet for candidiasis for 40 days.
- limit sweets: chocolate, sugar, sweets, buns, sweet carbonated drinks;
- use unrefined unrefined products for food (bread made from wholemeal flour, rolled oats - boiled for 15 minutes, etc.)
- be sure to use dietary fiber in food: corn porridge (mamalyga), brown rice, apples, plums;
- include in your diet foods that actively displace Candida fungi from the body: carrots, cloves, lingonberries, capsicum, etc.
- 5. do not use food products with preservatives, dyes and other chemicals. The human genetic apparatus is not designed for these chemicals. It is intended for food products only.
- remove products with yeast for 1-2 months: yeast bread, kvass, etc.
The use of liquid probiotics Bifidum BAG and Trilact with active bifidobacteria and lactobacilli in basic treatment regimens for urogenital infectious and inflammatory diseases increases the effectiveness of treatment and reduces the frequency of thrush relapses. The effect is enhanced by the combined use of probiotics (externally and internally), i.e. with simultaneous correction of intestinal and vaginal microcenoses.
Prophylactic use of liquid concentrates Bifidum BAG and Trilact in optimal age-related doses prevents the development of dysbiotic disorders of the vagina and associated diseases, such as thrush, in girls.
Relapses of candidal vaginitis with basic therapy are 57%.
If you add Bifidum BAG in addition to basic therapy, it turns out:
a) when taking Bifidum BAG only orally, relapses are observed 3.8 times less often;
b) and with simultaneous sanitization of two biotopes, i.e. when using the drug simultaneously vaginally and orally, the number of relapses is reduced by 12 times.
Conclusion: the same drug, used according to different dosage regimens, gives different effectiveness in gynecology.
In addition to oral and vaginal use, adding nasal drops to the treatment regimen will provide a deeper correction of the microbiocenosis of the entire body, since all mucous membranes are immunologically connected to each other.
Cystitis in men
1 Diagnosis of cystitis in men
2 Diagnosis of cystitis in men
3 Diagnosis of cystitis in men
Cystitis in men is a rather rare phenomenon; the disease can appear as a result of an inflammatory infection, due to which the urethra, ovaries and prostate gland begin to suffer.
To make a correct diagnosis, sometimes men only need to undergo a rectal examination, which will help determine whether there is an enlarged prostate. If the inflammation continues long enough, you will need to do an ultrasound and intravenous urography.
Types and forms of cystitis
Like other diseases, cystitis can be acute or chronic .
Acute cystitis
Acute cystitis manifests itself differently in all people; it can last from 2 to 10 days and occur with alternating periods of exacerbation and remission.
The acute form of cystitis is characterized by fever, chills, general weakness, difficult and painful urination. Urine comes out in small portions, sometimes requiring effort to pass it out. During urination, the patient feels a burning sensation in the urethra, and after it - a pain in the lower abdomen. In acute cystitis, a picture of general poisoning of the body may be observed (body temperature 38-40 degrees, weakness, sweating, dry mouth, thirst). This may indicate that the infection has spread to the tissues of the kidneys and renal pelvis, leading to the development of pyelonephritis. In this case, emergency medical care is required.
Chronic cystitis
Chronic cystitis is characterized by waves of exacerbation and decline of the disease. There is a frequent urge to urinate and pain when passing urine. In chronic cystitis, the symptoms are constant, only their intensity changes during treatment. Microorganisms in the urine in this form of the disease are not detected during laboratory examination. Tuberculous cystitis poses a particular danger.
Forms of cystitis in chronic form:
- latent cystitis (has hidden, implicit symptoms, characterized by the absence of obvious exacerbations);
- persistent cystitis (exacerbations occur more than 3 times a year);
- interstitial cystitis (constant, sometimes unexplained pain in the bladder, frequent exacerbations, deformation of the bladder walls).
There are also other forms of the disease - for example, postcoital cystitis ( cystitis after sex ), as well as “honeymoon cystitis” (occurs in women after defloration). The mechanism of postcoital cystitis lies in the anatomical feature of the female urethra. During sexual intercourse, vaginal mucus is thrown into the urethra, which causes irritation and inflammation. The disease can be triggered by frequent changes of sexual partners.
“Honeymoon cystitis” occurs against the background of disturbances in the vaginal microflora that already exist at the time of the onset of sexual activity. The same “thrush” can cause acute cystitis in a woman. Sexual intercourse is accompanied by abundant discharge of vaginal microflora into the urethra and bladder, which until now have not been subject to such “close” contact with infection.
1 Gynecological examination for cystitis
2 Laboratory diagnostics for cystitis
3 Ultrasound of the genitourinary tract