Causes of glossitis
Glossitis can be an independent disease caused by bacteria, or a sign of a certain systemic pathology. Microtraumas and viruses usually lead to local damage to the tongue. For example, herpes very often not only affects the mucous membrane of the oral cavity, but also causes the occurrence of stomatitis and glossitis.
Inflammation of the tissues of the tongue can be a consequence of a burn to the mouth or frequent consumption of too hot drinks. Open gates for infection that causes glossitis are mechanical injuries to the oral cavity and tongue. Provoking factors also include:
- smoking, alcohol abuse;
- eating spicy foods;
- using a mouth freshener;
- frequent use of mouth rinses;
- poisoning with salts of heavy metals;
- injury to the tongue by destroyed sharp teeth;
- frequent exposure of the skin of the tongue to chemical irritants and electric current.
Causes of chronic glossitis:
- decreased immunity;
- dysbacteriosis;
- conditions that cause autoantibodies to be produced.
Causes of glossitis in children
Glossitis occurs in children for various reasons. Most often it is provoked by the child constantly biting his tongue. An incorrectly selected brace system can also lead to problems. Desquamative glossitis in young patients is a consequence of helminthic infestations, atopic dermatitis, and blood diseases. In this case, there are usually no difficulties when chewing and swallowing food.
Candidal glossitis in children develops against the background of diabetes mellitus and long-term use of antibiotics.
Care instructions
- Hygiene. We brush our teeth, but forget about our tongue. Thanks to advertising in the media, people are more likely to buy toothbrushes with a special brush for cleaning the tongue - and this is important. After all, bacteria live in the gap between the taste buds and food particles remain that must be removed from there.
- Caring for your oral health. Do not forget about the cleanliness of the palatine tonsils and the presence of reflux of gastric contents into the oral cavity.
- And the most important thing is to monitor your general health, undergo a timely examination by a doctor to identify the cause of inflammation - primarily to the dentist, but if you even consult a therapist or an infectious disease specialist, or an ENT doctor - you will not be mistaken, since there are almost no diseases, which would not affect such an important organ one way or another.
Symptoms of glossitis
Glossitis is manifested by the following general symptoms:
- sensation of a foreign body in the mouth;
- burning tongue;
- discoloration of the skin of the tongue to bright red or burgundy;
- swelling of the tongue;
- increased salivation;
- dullness or complete loss of taste sensations (perversion of taste is possible);
- difficulty in swallowing;
- slurred speech, severe pain during conversation.
If treatment for glossitis is not carried out or is illiterate, the disease becomes chronic. Then dense, persistent swelling of the tongue occurs and its structure changes. In advanced forms, growths may form. The onset of an abscess is indicated by an uneven increase in size of the organ. Then the pain syndrome becomes pronounced.
If glossitis is complicated by phlegmon, purulent discharge appears on the surface of the tongue, and the process of chewing and swallowing food is disrupted. Attacks of suffocation may occur and speech becomes difficult. The body temperature rises, the lymph nodes become enlarged, and weakness increases.
Signs of glossitis caused by bacterial and viral microflora
Glossitis of the tongue, which is caused by pathogenic microflora, manifests itself with symptoms:
- local increase in temperature;
- soreness;
- edema;
- hyperemia.
If the disease is provoked by viruses, it may be characterized by vesicles, after opening which small erosions remain on the mucous membrane. In this case, the taste organ becomes too dense or, conversely, excessively loose, and hyperplastic changes are observed.
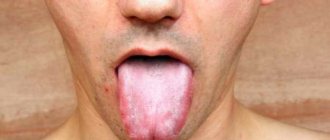
Candidal glossitis looks in the photo as a white coating on the tongue.
Symptoms of different types of glossitis
Desquamative glossitis, which is also called “geographical tongue,” usually develops against the background of gastrointestinal diseases. When examining a patient, the doctor sees a tongue cut with grooves and lines, which may resemble the outlines of the continents. The formation of the disease is promoted by:
- blood diseases;
- metabolic disorders;
- parasites.
Bright red spots with desquamative glossitis are located on the front surface and sides of the tongue. In this case, the patient complains of moderate pain and burning.
Deep glossitis is always localized at the “bottom” of the oral cavity. Inflammation can spread to the neck and chin area. Untimely treatment of this type of pathology leads to an abscess.
Diamond-shaped or median glossitis is manifested by thickening of the epithelium and the formation of diamond-shaped areas in the basal region of the tongue. Their color can be bright red or bluish. The form is prone to chronicity and relapse. Very rarely, rhomboid glossitis can be characterized by other signs. Thus, the diamond-shaped areas may become smooth and atrophy (flat form) or dense, bumpy growths may form on the surface of the tongue (warty form of rhomboid glossitis).
Folded glossitis is a congenital anomaly. These are folds on the back of the tongue. The deepest of them runs longitudinally along the midline of the taste organ. Since the disease does not cause discomfort, no special treatment is carried out (only for aesthetic purposes).
The main symptom of villous glossitis is the proliferation of filiform papillae, which subsequently become keratinized and look like small villi. The problem most often occurs with constant trauma to the tongue or with candidiasis.
Gunter's glossitis indicates the development of folate deficiency or B12 deficiency anemia. The tongue becomes very smooth and acquires a bright crimson color. Taste buds atrophy.
Interstitial glossitis (precancerous form) may indicate infection with syphilis. Part of the muscle tissue is replaced by connective tissue. The tongue looks like a quilt. Some of its parts are elevated, the grooves of connective tissue strongly tighten the edges. If treatment is not started, the muscle tissue completely degenerates into connective tissue.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Forms and types of disease
Inflammation of our organ of taste occurs frequently and does not always manifest itself with symptoms, proceeding completely hidden from us.
There are several forms and types of the disease:
- According to the duration, the disease is divided into acute (develops quickly and lasts no more than a month) or chronic glossitis (lasts more than a month);
- According to the form of the lesion, the catarrhal form (proceeding with redness and swelling) and the desquamative form (proceeding with a change in appearance) are distinguished;
- purulent forms - phlegmon and abscess (a purulent focus in the thickness of the organ tissue itself);
- a separate group includes neurological diseases of the nerves innervating this organ.
Cellulitis and abscess occur acutely, they are associated with infection and require urgent surgical intervention. They manifest themselves as severe pain, chills and swelling of the lymph nodes of the neck - this form can be confused with acute inflammation of the salivary glands, so diagnosis using ultrasound and x-rays is needed. It is better not to delay these symptoms and seek medical help as an emergency.
The catarrhal form of glossitis manifests itself with a sharp blood supply - the tongue swells, becomes bright red - this can manifest itself, for example, with scarlet fever, or an allergic reaction, which, in addition to the organ of taste itself, spreads to the soft palate with the tongue. Treatment in this case is aimed at eliminating the allergic reaction and inflammation.
The largest and most heterogeneous group is desquamative glossitis. It is difficult to list the number of factors (external, internal) that can provoke this form of the disease. We will not make a mistake if we say that “the tongue is the mirror of the digestive tract.” Since it contains many nerve receptors and papillae of different shapes and purposes (filamentous, cone-shaped, mushroom-shaped, leaf-shaped, groove-shaped), a change in each link of its anatomy outwardly reveals a hidden disease. Let's take a little look at the most common diagnostic signs of these conditions.
Diagnosis of glossitis
Pronounced symptoms allow dentists and therapists (it is these doctors who treat glossitis) to judge the presence of one form or another of the disease. To assess the depth and nature of the lesion, as well as to diagnose the disease that provoked the development of glossitis, different methods are used:
- bacteriological;
- cytological;
- biochemical;
- histological;
- serological.
All these diagnostic methods are available in any modern dental clinic
. To exclude the presence of syphilis, microscopy of the scraping is performed for Treponema pallidum, and an anticardiolipin test (allows us to detect antibodies to the cardiolipin antigen present in the blood of patients with syphilis). If it is necessary to determine the causative agent of glossitis, the following is carried out:
- PCR diagnostics (detection of the pathogen by its DNA);
- Enzyme-linked immunosorbent assay (ELISA). For analysis, blood is taken from a vein. The study is aimed at identifying specific antibodies produced by the patient’s body against the pathogen.
Desquamative
This type has other names: “geographical” tongue and migratory or exfoliative glossitis. Its characteristic feature is focal damage to the epithelial layer and desquamation of the papillae, which ultimately leads to the formation of a heterogeneous surface on the tongue, similar to a map, with red spots separated by whitish ridges. It is called migratory because the affected areas tend to recover, while neighboring ones, on the contrary, become inflamed, gradually changing the pattern. This symptom is typical for disruption of the circulatory, digestive and endocrine systems of the body.
How and with what to treat glossitis of the tongue in adults and children
Treatment of tongue glossitis requires elimination of the diseases that led to its appearance. This refers to anemia, gastrointestinal diseases, syphilis, etc. To minimize pain, you need to rinse your mouth with Furacilin, a solution of Chlorhexidine (0.05%) or potassium permanganate, and avoid eating rough food. In case of severe pain, local applications with anesthetics can be made:
- Trimecaine solution (2%);
- Lidocaine solution;
- Pyromecaine solution.
If the tongue is dry, it should be lubricated with a mixture of glycerin and Anestezin.
For a speedy recovery, the skin of the tongue must be cleaned of plaque using a cotton swab soaked in proteolytic enzymes (Chymotrypsin, Trypsin). If there are painful ulcers, these drugs for the treatment of tongue glossitis can be replaced with applications with Iruksol. After the hygiene procedure, it is important to treat the cleaned lesions with antiseptics. This helps prevent secondary infection and also prevents the development of serious complications.
To speed up regeneration processes, gel and jelly-like medicines with solcoseryl, as well as preparations containing vitamin A, can be used. The mixture formed by rosehip oil and vitamin A heals the affected skin well and relieves pain.
If excessive thickening of the stratum corneum of the epidermis (hyperkeratosis) is observed, surgical intervention is ordered. Antifungal, antibacterial and anti-inflammatory drugs are selected taking into account the severity of the disease and the dominant symptoms.
All patients with glossitis can take immunomodulators. Hormones are used extremely rarely - only for difficulty breathing. To avoid atrophy of taste organ cells, Hydrocortisone and Prednisolone ointments are prescribed in short courses.
How to treat tongue glossitis at home
Treatment of tongue glossitis at home can be carried out using traditional medicine recipes:
- decoction of chamomile flowers. 1 tbsp. pour a glass of boiling water over the flowers. Infuse, strain. Rinse your mouth after every meal;
- bedstraw decoction. 1 tbsp. pour a glass of boiling water. Leave for 30 minutes. Take 50 ml orally after meals and rinse the mouth 3-4 times a day. Similarly, you can use decoctions of sage and basil;
- soda solution. Add 2-3 drops of iodine and a teaspoon of baking soda to a glass of warm water. Rinse your mouth 3 times a day;
- natural honey Slowly dissolve a spoonful of honey;
- propolis. Lubricate the areas of inflammation 5 times a day. Instead of propolis, you can use raw carrot/potato juice or rosehip oil;
- tea tree oil. Dilute in equal proportions with olive, sunflower or sea buckthorn oil. Treat glossitis lesions 5 times a day or keep it in your mouth for several minutes.
Candida
The name comes from the pathogens, fungi of the genus Candida, which provoke this disease, so another common name is fungal glossitis. In addition, it is often called yeast glossitis. This disease indicates the presence of a fungal infection in the body and a sharp decrease in the level of immunity. Chronic candidal glossitis is characterized by exacerbations when the body's immune response is weakened due to seasonal respiratory and other infectious diseases. Most often, this disease affects newborn children and people after long-term antibiotic therapy. Yeast is treated with antifungal drugs, as well as immunomodulators.
Mycotic
Mycotic glossitis is not an independent disease, since it appears as a result of damage to the ENT organs by a fungal infection. Most often, this type of glossitis accompanies diseases such as chronic fungal pharyngitis or tonsillitis. A characteristic feature of this lesion is a highly swollen tongue, mottled with furrows and spots of whitish plaque against a background of smooth red areas. In order for the treatment of mycotic glossitis to be successful, it is first necessary to cure the underlying disease.
Catarrhal
This inflammatory process is most often an accompanying symptom of stomatitis, since its development is caused by contact with decayed diseased teeth, dentures, and tartar. In addition, the appearance can be caused by thermal and chemical burns, poisoning, injuries (traumatic glossitis). The body’s reaction to alcohol and nicotine tars, manifested by this inflammatory process, cannot be ruled out. Treatment of catarrhal or traumatic glossitis primarily consists of eliminating the cause that triggered the onset of the disease.
Diet for candidiasis in the mouth
Patients with oral candidiasis should change their diet by reducing the intake of simple carbohydrates. The latter include sugar, sweet fruits and berries, confectionery, honey, apples, grapes, white cabbage, legumes and drinks such as milk, kvass, and beer. This is due to the fact that yeast-like fungi can only use carbohydrates as food.
The second point is that you need to increase the amount of foods consumed that can suppress the development of Candida. The growth of fungi can be controlled by natural yoghurts containing live lactic acid cultures, as well as products with natural antifungal activity (garlic, propolis, hot red pepper).
Features of the disease
With candidiasis, there is an active spread of fungi of the genus Candida. Most often it is Candida albicans. To identify the pathogen, doctors carry out laboratory diagnostics - microscopic and bacteriological examination of the mucous membranes of the mouth, scraping plaque from the tongue.
Oral candidiasis is usually classified into two types:
- Yeast stomatitis. Affects the cheeks, gums, and palate. The tissues become covered with a characteristic white coating that cannot be easily removed.
- Yeast glossitis. The source of infection is the tongue. His back is affected. Small deep grooves are formed on its surface, in which whitish masses are deposited.
Tongue thrush always has clear clinical symptoms. It leads to swelling and inflammation of the tissues, causing severe pain. It gets to the point that the patient cannot chew food or even drink normally. The situation is aggravated by bad breath, which cannot be masked in any way.
folded
Since folded glossitis in most cases is a consequence of a gene abnormality and is present in a person from birth, without causing him any particular inconvenience, treatment of this type is necessary only in cases where the symptoms begin to bother the patient. The main symptom (the presence of a large number of folds) in itself is not a reason to start treatment. If this lesion is provoked by a sharp lack of vitamins, causing keratinization of the epithelial layer, dryness, soreness and the formation of cracks, it is worth considering a course of taking vitamin preparations.
Content:
- Features of the disease
- Causes of yeast glossitis
- How it manifests itself 3.1. Other symptoms of candidiasis on the tongue
- Treatment of tongue candidiasis 4.1. Medicines used for candidiasis 4.2. Traditional methods of combating oral candidiasis
- How to eat during treatment
- How to avoid getting sick
For the full functioning of all parts of the gastrointestinal tract, various fungi and bacteria must be present in the body.
They are called opportunistic pathogens. If their quantity corresponds to the norm, the person feels well and does not experience unpleasant symptoms of the disease. But under the influence of negative external or internal factors, bacteria and fungi can begin to actively multiply. Then their activity becomes abnormal - a disease of the oral cavity or stomach or intestines is diagnosed. It is in this scenario that candidiasis develops on the tongue, throat and cheeks. Let's look at how to treat it and what measures to take to avoid relapse after recovery.
Aphthous
The consequence and logical continuation of the catarrhal form in the absence of timely treatment is most often aphthous glossitis. Or, as it is also called, ulcerative glossitis, since its most striking symptom is the formation of shallow aphthae and ulcers on the upper layer of the tongue. When the lesions become deeper, the tongue swells, and blood begins to ooze from the ulcers, we can talk about the onset of erosive-ulcerative glossitis. In this case, the disease is accompanied by an unpleasant odor and abundant gray plaque. It is more logical to begin treatment of ulcerative glossitis by eliminating the causes of its occurrence, combining this process with local therapy.