Causes and duration of pain Mechanism of pain Localization Stages of healing Possible complications When to see a doctor What to do after removal What not to do How to reduce pain
Tooth extraction (removal) is a surgical intervention accompanied by damage to the periodontal tissues (gums, bone socket, mucous membrane). Pain after tooth extraction is a normal reaction of the body to surgery. Depending on the complexity of the clinical situation, the volume of the operation, after the procedure, when the effect of the anesthetic wears off (after 3-4 hours), the patient begins to feel aching pain in the injured area.
Why and how much does it hurt?
Pain occurs due to traumatic swelling of tissues and compression of nerve endings. The more complex and extensive the operation, the more intense the gum pain after tooth extraction. Normally, symptoms after extraction of an incisor or molar are as follows:
- Aching pain persists for 1-3 days
, but subsides day by day; - slight swelling, hematoma, redness around the removed unit (may increase for 2-3 days
and then subside); - formation of a blood clot in the wound;
- the appearance of a whitish coating (fibrin, which accelerates tissue healing).
This is a normal reaction to surgery. How much a tooth hurts after extraction depends on the complexity of the operation, the characteristics of the body, the patient’s pain threshold, the location of the dental unit in the row (after extraction of molars, the injury is more extensive and worries longer). Normally, discomfort lasts
3-5 days
, gradually subsides and disappears on its own.
Tissues are restored
about
10-14 days
. By this time, the mucous membrane has completely healed, new bone begins to form inside the hole, which will completely fill the defect in about six months.
The most difficult to treat and remove is the 3rd molar (figure eight, wisdom tooth). They have very curved, intertwined roots. A wisdom tooth is often completely unerupted (impacted), covered with mucous or bone, and incorrectly erupted (dystopic). The operation is hampered by difficult access to the figure eight. Therefore, healing after a complex 3rd molar extraction may take longer (about a month). But if pain and swelling have not begun to subside a week after the intervention, you need to consult a dentist.
Content:
- Options for local anesthesia of a diseased tooth 1.1. Application 1.2. Infiltration 1.3. Conductor 1.4. Intraosseous 1.5. Intraligamentary
- Contraindications
- Pros and cons of local anesthesia in dentistry
To ensure that tooth extraction takes place with maximum comfort for the patient and is not associated with pain, dentists use special painkillers.
If the case is very complex and local anesthetics do not cope, anesthesia is used. Painkillers used in dentistry block the transmission of nerve impulses from the torn unit to the brain. Due to this, all manipulations carried out by a specialist are calmly perceived by a person.
Mechanism of pain
- Trauma to soft, hard periodontal tissues;
- damage (rupture) of the connective tissue holding the tooth;
- destruction of blood vessels and nerve endings;
- swelling of the injured gum, pressure on nearby areas, poor circulation;
- irradiation of pain along the nerve trunks to other parts of the maxillofacial areas.
Pain after extraction of any dental unit is a natural reaction of the body to the intervention. No matter how carefully the surgeon acts, the integrity of the vessels, nerves, and fibers is inevitably compromised. It is normal for the extracted tooth to hurt for no more than 2-3 days.
, after removing the figure eight, the gums may bother you
for about a week
. If after 7-10 days the discomfort does not disappear, but continues or increases, you need the help of a doctor.
Types of deletion
Wisdom teeth (eights, third molars) are larger than other dental units in the row. They differ not only in size, but also in the complex anatomy of the root system. Eight has from 2 to 6 roots
, which are often closely intertwined with each other. Given the complex arrangement of wisdom teeth, when they are removed, a significant wound is created.
The risk of complications will directly depend on how difficult the figure eight extraction was. With simple extraction, when the tooth is intact, the roots are not intertwined, and there are no other pathologies (pulpitis, periodontitis, etc.), the risk of complications is minimal. In such a situation, the doctor uses forceps or an elevator to remove the tooth from the socket.
If the wisdom tooth is incorrectly positioned (horizontal eruption, severe curvature), intertwined roots, significant destruction of the coronal part, or the presence of inflammation, a more global surgical intervention may be required. An incision in the gum, cutting a tooth into pieces with a drill, removing root fragments through the jaw bone and other manipulations significantly increase the traumatic nature of the procedure. Aching pain, swelling after removal of the figure eight, increased temperature (up to 37.5℃), hematoma on the cheek - this is a normal reaction to the intervention, which lasts no more than 5-7 days.
Localization of pain
As a rule, painful sensations are localized in the area of innervation of nerve endings injured during the intervention. Depending on where the hole is located, the pain can radiate to the throat, temple, or ear. Often, after tooth extraction, the neighboring tooth hurts. The most common reason is damage to soft tissues from instruments, which causes the gums around the wound to swell, begin to hurt, and the pain spreads further to neighboring units.
Incisors and canines usually have 1 root, which makes their removal the least traumatic. Chewing units have 2-3 or more roots, which complicates the operation and makes it more voluminous. The back teeth of the upper jaw border the bottom of the maxillary sinuses; after removal, the pain can radiate to the nasopharynx, cheek, orbit, and ear.
If after the removal of the lower tooth the jaw hurts, especially when it comes to multi-rooted chewing units (7, 8 teeth), this is normal. Usually such sensations go away within a few days. You need to go to the dentist if the pain does not subside after 5-7 days and is accompanied by other alarming symptoms.
Information on the use of drugs
If the procedure was not complicated, it is quite possible that painkillers will not be needed during the recovery period. But it’s better to take an analgesic half an hour before the end of the anesthesia (the doctor will tell you about the approximate time). This will help prevent pain, which is almost inevitable after a complex removal, accompanied by drilling the bone, opening an abscess, cutting out affected tissue, suturing, etc. Drugs such as ketanov, nimesil, nimik, etc. will help you quickly cope with pain. Among other things, they also have an anti-inflammatory effect.
The patient must inform the doctor about his state of health and existing diseases. This is especially important when it comes to arterial hypertension, diabetes, hemophilia, and low platelet levels in the blood. Your dentist should also know if you have a tendency to nosebleeds or have recently had an acute respiratory infection or the flu. In this case, the specialist selects individual methods for caring for the hole.
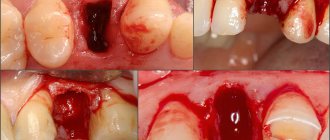
Stages of socket healing
- 2-3 hours
after
a blood clot (thrombus) forms
in the socket . It serves as a barrier to pathogenic microorganisms, preventing them from entering the wound. - The next 2-3 days
- the blood clot thickens, shrinks, the wound
becomes covered with a whitish coating
(fibrin film), the formation of granulation tissue begins inside the hole, the basis for the restoration of mucous membranes. - After 3-7 days
, the thrombus lightens, becomes whitish, the connective tissue has practically filled the hole, swelling and pain are minimal or completely absent. - After 7-10 days
, the hole has shrunk significantly,
new bone begins to form
, which will completely fill the defect after 4-6 months. - After 2 weeks
,
the gums have completely healed
.
What are the possible complications?
The intensity of pain must be carefully monitored. Unpleasant sensations must subside, otherwise it indicates the development of pathology. The gums hurt especially painfully after difficult removal if inflammatory complications develop:
- Alveolitis is an inflammation of the bone socket and surrounding tissues. accompanied by acute, throbbing pain, redness, swelling, the formation of yellow, greenish, dark gray plaque, cloudy pus with a putrid odor. The cause of the complication is poor hygiene in the postoperative period, ignoring the drug therapy prescribed by the doctor.
- Dry socket - there is no blood clot in the socket, it is dry, empty, there is a yellowish-gray coating, a putrid odor. The reason is that the clot was not formed due to a blood clotting disorder; the clot was removed from the socket by the patient during hygiene, intensive rinsing, etc.
- Socket bleeding - may be associated with a blood clotting disorder, excessive damage to tissues, blood vessels, or a fracture of part of the alveoli.
- Facial neuralgia is a rare complication that occurs due to damage to the facial nerve during tooth extraction. Accompanied by numbness in the cheeks, tongue, lips.
- Periostitis is a purulent inflammation of the periosteum that develops for the same reasons as alveolitis. Accompanied by acute, diffuse pain that cannot be relieved with an analgesic. Swelling is pronounced, can spread to the neck, temperature is above 38℃, general intoxication of the body is observed (headache, weakness, etc.).
- Osteomyelitis is a purulent-necrotic lesion of the jaw bone, accompanied by throbbing pain radiating to the ear, temple, fever, swelling of the gums and oral mucosa, spasms of the masticatory muscles, deterioration in general well-being, and enlargement of the submandibular lymph nodes.
Cheek pain after tooth extraction is a very common symptom, the duration of which depends on the complexity of the intervention. Normally, aching pain completely subsides after 2-3 days
. The picture is completely different when complications develop. With inflammatory complications, purulent foci form in the tissues, and the risk of spread of purulent contents through the general bloodstream increases many times over. There is a high probability of phlegmon, abscess, and destruction of bone tissue. Serious surgery and long-term rehabilitation are inevitable.
General information about bone grafting
Bone grafting is a common dental surgery to restore the volume of bone tissue in the jaws. This surgical intervention allows you to restore the patient’s dentition in the most physiological way possible through dental implantation (it is carried out together with bone grafting or after it). This treatment has many advantages over the installation of removable dentures, including the aesthetics of the smile and the correct distribution of chewing loads.
There are several osteoplastic techniques:
- Splitting of the alveolar ridge (the graft is immersed in the cancellous part of the bone, where it quickly and fully takes root);
- Replanting a bone block (engraftment is a little worse, since the graft is fixed on the side of the bone where there are practically no vessels, so it is advisable to use the patient’s own tissue);
- Guided tissue regeneration (a technique in which a very high-quality graft is used, and a positive result is guaranteed by fixation of a collagen protective membrane);
- Sinus lifting (surgery on the upper jaw, which involves the bottom of the maxillary sinus).
The dentist chooses the appropriate bone restoration technique independently. But no matter what technique he chooses, recovery after surgery will be the same everywhere. The patient should not forget that the procedure itself is not a 100% result. It is equally important to follow all the dentist’s prescriptions, including taking medications after bone grafting and sinus lifting (the most common bone restoration procedure).
When do you need to see a dentist urgently?
- Severe, acute, throbbing pain that is not relieved by an analgesic, spreads across the face, radiates to the ear, neck;
- bleeding from the socket that does not stop, but rather intensifies;
- absence of a blood clot in the socket;
- bad breath;
- discharge of pus from the wound;
- the formation of yellow, dirty gray, green plaque on the wound;
- temperature rise above 38℃;
- numbness of a part of the face (gums, cheeks) for more than a day;
- pronounced swelling of the gums and cheeks, which does not decrease 2-3 days after extraction.
Patient's fears
The reason for a person’s patience and postponing the procedure for later is stories from acquaintances and friends about pain and frightening reviews on social networks and forums.
When pain occurs as described by those being treated:
- during surgery - common when a tooth is removed from the lower row and is associated with the structure of the jaw. The dental surgeon needs to use a thin needle of a syringe with an anesthetic to hit the jaw nerve located in the gum; therefore, when the doctor is inexperienced or in a hurry, he does not hit this point, and therefore does not freeze; Also, the reason for the lack of pain relief may be diffuse inflammation, which also reduces the effect of freezing.
- after the procedure - is associated with interference in the body, especially typical for complex removal, which is associated with strong interference in the tissue, and can also cause the development of inflammation of the socket after the removal of a wisdom tooth.
While taking it, listen carefully to your feelings. If you don't feel enough numbness in your tongue and gums, ask for an extra shot to avoid a traumatic experience.
Important! Find out in advance what type of anesthetics are used in the clinic. Paid institutions use derivatives of articaine. Lidocaine has proven to be less effective in these cases.
For competent removal of wisdom teeth without pain, the manual skill and experience of the doctor is important. Correct use of anesthesia will avoid pain, and following the doctor’s recommendations after surgery will protect you from inflammation and swelling.
Aware means armed
Even if you consult an experienced doctor and follow all the advice, side effects may occur in the first days or weeks of removal.
Swelling after wisdom tooth removal is associated with inflammation of the place where the tooth was recently located. If there is bad breath, pain when cold or hot gets on the wound, and there is no special clot that protects against food, then infection is possible. See your doctor.
Numbness of the lower lip - occurs when working on the lower jaw, when the position of the tooth is too close to the mandibular nerve.
Bleeding is common in the patient's chair, but spontaneous bleeding may occur in the following cases:
- apply a swab or rolled cotton wool to the hole and bite down forcefully to compress the wound;
- use ice packs on the cheek;
- take blood pressure medications if necessary
Types of deletion
The division is quite simple: the bottom row, twisted, twisted roots bring more problems, while the bone is dense and uniform.
Simple
Characteristic for the correct positioning of the tooth and easy accessibility of the working area. In this case, after anesthesia, the dental surgeon uses an instrument resembling a scalpel to separate the mucous membrane from the dental tissue, and then begins to loosen it using forceps.
For the top row, an elevator is used - with the help of which it is removed from the hole. The mobile root is then removed with forceps.
The process takes 10 minutes, including suturing.
Complex
Suitable for unerupted lower teeth with branched, crooked roots, severe tilting or curvature, or complete destruction of the upper part of the tooth.
In this case, it is not possible to use forceps for grasping, and the actions are as follows:
- cutting the gums - first, as in a simple removal, the mucous membranes are pulled apart in order to see the roots of the tooth and the bone around it;
- sawing the tooth into pieces with a drill;
- extraction of each root separately using an elevator.
Note! At this stage, the bone under the teeth is drilled to increase loosening and speed up extraction from the jaw.
After the operation, the wound is sutured. Whether to remove the stitches or whether they will dissolve on their own in 7-10 days depends on the clinic and specialist.
For complex manipulations, a preliminary full diagnosis with an X-ray or volumetric 3D computer image is required to develop a removal strategy. With the correct preparatory stage, after the removal of a wisdom tooth, the socket, gums and cheek do not hurt.
Diagnostics makes it easier
A comprehensive consultation is first required, which consists of several stages:
- Anamnesis collection - information about allergies to medications, chronic diseases (diabetes, asthma, blood pressure surges, clotting problems). At the same time, the patient’s data is not personal speculation; it is necessary to donate blood for indicators of interest and, if possible, take extracts from the cards;
On a note! Many drink aspirin uncontrollably, which thins the blood and leads to the development of severe hematomas during intervention, so it is necessary to notify the doctor. Women need to be told about the day of the menstrual cycle, since platelet counts in the first days decrease by 40% and contribute to difficulties in stopping bleeding.
2. After the tooth is removed, the dentist will carefully check whether there are any dental remains left, and if necessary, apply a drug into the socket that will reduce the risk of inflammation and swelling after the removal of the wisdom tooth;
3. Applying sutures even with simple removal is not a classic wound removal, but bringing tissues closer together so that food debris does not fall into the hole, preserving the clot and reducing inflammatory processes by 80%. Some people use self-absorbing sutures, so you don’t have to visit the dentist additionally. Spare no expense, it will save nerves and speed up recovery.
What can and should be done after tooth extraction
- 20-30 minutes after the intervention, carefully remove the cotton swab
; - use cold compresses
for 2-3 hours after the intervention (take a break every 10-15 minutes to avoid tissue hypothermia); - for 3-5 days, make oral baths
with antiseptic solutions (take the solution, hold it in your mouth for a minute, spit); - When carrying out daily hygiene, avoid the injured area
, you can start using the toothbrush on the 2-3rd day, it should be new, with soft bristles; - chew on the opposite side
; - Eating is allowed after the anesthesia wears off (not earlier than 3-4 hours later
).
What is a sinus lift?
One of the most modern and safe operations to correct bone tissue in the alveolar processes is sinus lifting. It is a surgical intervention on the upper jaw, during which the bottom of the maxillary sinus is raised, and osteoplastic material is inserted into the resulting cavity. Rehabilitation after such an operation involves long-term adherence to certain rules and taking medications, for which the patient must be prepared.
Sinus lifting can be open or closed. The first involves the correction of large volumes of the alveolar ridge, and the second allows for immediate implantation of artificial roots. Sinus lift techniques are constantly being modified, so patients can be confident in the safety of surgery.
What is prohibited?
- To prevent accidental washing of a blood clot from the socket, it is forbidden to rinse your mouth. To treat the cavity, oral baths are quite sufficient;
- Hot compresses are prohibited, this stimulates severe swelling, the development of inflammation, and bleeding;
- You cannot puff out your cheeks, blow your nose too much, or sneeze;
- It is forbidden to touch the wound with your fingers, tongue, or objects;
- You can’t eat hot, cold, irritating foods; preference is for soft, warm, neutral foods;
- you cannot smoke or drink alcohol for at least a week - tobacco and alcohol slow down tissue regeneration;
- Hypothermia and overheating must be avoided - going to the sauna, swimming pool, solarium is prohibited for 5-7 days;
- Do not take aspirin or other blood thinners;
- do not engage in active sports, do not subject the body to excessive physical or sports stress.
Is it possible to return to a normal lifestyle?
It is important to pay attention not only to hygienic care of the hole, but also to habits in general. These, as well as lifestyle, can significantly affect healing. Therefore, out of a sense of caution and self-preservation, it is better to temporarily refrain from certain habits. The following points are worth noting:
- It is highly advisable to refrain from smoking and drinking alcohol on the day of surgery (or better yet, several days after). Tobacco dries out the mucous membranes and can cause dry socket syndrome. And alcohol and pills are generally incompatible.
- Do not touch the hole with your tongue or create a vacuum in your mouth. The latter is relevant for those who are used to sucking their lips. These actions can break up the blood clot.
- It is better to refrain from physical education and physical labor for a couple of days, and it is advisable to sleep on a high pillow.
- Ideally, you should avoid high temperatures (steam rooms, baths) and hot compresses, which can cause bleeding.
- After removal, you cannot eat for several hours. Then for at least a week you need to make sure that the food is soft, liquid, not cold and not hot. It is better not only not to chew on the healing side, but also to prevent food from getting there at all.
- You need to brush your teeth very carefully, especially near the wound. In the evening after removal, it is better to abandon the procedure.
How to reduce pain?
Analgesics will help relieve pain after removal of a molar (or any other tooth) - it is better if it is one of the non-steroidal anti-inflammatory drugs (NSAIDs). Antihistamines will help remove swelling, and antibiotics will help prevent inflammation. The doctor will prescribe effective medications according to the clinical picture. Medicines should be taken strictly as prescribed. Treatment for pain after tooth extraction depends on the cause of its occurrence. The most important thing after the intervention is to scrupulously follow the dentist’s instructions and recommendations. This will help reduce recovery time and avoid complications.
Author of the article Voznyuk Vladimir Aleksandrovich Maxillofacial surgeon-implantologist of the highest category
Work experience: 28 years.