Language is a kind of indicator of health status. Some changes in the color, shape, and structure of the taste organ may indicate specific internal pathologies, so you need to pay attention to its appearance.
For example, a raspberry tongue can be a symptom of diseases such as scarlet fever, Kawasaki syndrome, chickenpox, measles . But it can also indicate less obvious pathologies: renal failure, vitamin deficiency. A complete list of diseases that can cause the tongue to turn red, and methods to combat them are listed in the article.
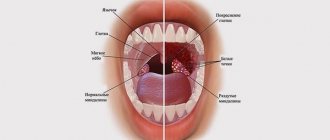
What does a healthy tongue look like?
First, let's remind parents what a healthy tongue looks like. The following signs indicate the state of normality:
- the size is not increased;
- humidity is moderate;
- the color of the tongue is pale pink, without spots or grooves;
- sensitivity is normal, papillae are not enlarged;
- allow for a light coating that is easy to clean;
- There is no bad breath.
If, upon examination of the child, the condition of his tongue corresponds to the signs described above, there is no reason to worry and see a doctor.
Cirrhosis of the liver
A red “varnished” tongue is often found in patients with cirrhosis of the liver.
A red “lacquered” tongue is often found in patients with cirrhosis of the liver, a chronic disease characterized by the formation of fibrous tissue in this organ. This is a deadly disease, from which it is almost impossible to completely recover if it is fully formed - the only reliable option is a liver transplant.
Otherwise, patients begin to complain of weakness, dyspepsia, fever and joint pain. Next, asthenia occurs and weight loss develops, and the liver itself increases in size and becomes deformed. At this stage, the patient is prescribed a strict diet, especially since he begins to suffer from a constant feeling of nausea and vomiting. In the terminal stage of cirrhosis, jaundice develops, swelling of the legs and varicose veins of the gastrointestinal tract occur, followed by bleeding - often fatal.
To prevent the occurrence of cirrhosis, doctors recommend following a proper diet and avoiding alcohol consumption.
Changes that should alert parents
In addition to changes in the color of the taste organ, parents should be wary of other accompanying symptoms, including:
- swelling, against which the imprints of teeth can be seen;
- insufficient moisture or obvious dryness of the surface of the tongue;
- enlarged papillae, especially pronounced in the root part;
- formation of persistent plaque on the surface of the tongue;
- burning sensation and impaired taste perception;
- the appearance of a specific odor from the mouth.
Parents can notice these changes during a visual inspection, which is best done in the morning in natural light. If the situation continues for a long time, the plaque thickens and the color of the tongue does not return to normal, there is every reason to consult a doctor to find out the reasons and identify hidden pathology.
Taking antibiotics
If a person often uses antibiotics, and also does so without the supervision of a doctor, he may subsequently find redness on the surface of his tongue. The muscular organ is not completely stained, but only along the edges and in the center.
If such problems arise, you should immediately consult a specialist, since unlimited use of drugs can cause pathological changes in internal organs, and a red spot in the middle can signal damage to the stomach.
If a person actually uses antibiotics often and a lot and this method of treatment is the only one for him, then the drug should be replaced with another drug that also belongs to the group of antibiotics. A reddened tongue may indicate an allergic reaction.
A red or pale tongue is not the norm!
Both options indicate pathological changes occurring in the child’s body:
- A crimson-red tongue always indicates the presence of an infection (viral, bacterial or fungal). Most often it is tonsillitis, scarlet fever, stomatitis or glossitis.
- A red and shiny tongue is a sign of anemia, exhaustion and severe stomach disease;
- A cherry tint is a sign of influenza and measles, as well as general intoxication or kidney dysfunction;
- A bluish color indicates a lack of oxygen; there is reason to suspect disorders in the cardiovascular system or lungs;
- Purple color may indicate blood and lung diseases, heart failure.
- A too pale tongue, being penetrated by blood vessels, a priori cannot be lighter than blood. In most cases, this sign indicates exhaustion, deficiency of folic acid or vitamin B 12.
Let us remind parents that very often there may be a coating on the surface of the tongue, the color of which also has its own characteristics.
Scarlet fever
Tongue with scarlet fever.
Another probable cause that can provoke redness of the mucous membrane of the tongue is scarlet fever, an infectious disease caused by streptococcus. The disease is contagious and is transmitted both from a sick person to a healthy person, as well as from a recently ill person or simply a carrier.
Scarlet fever is accompanied by a whole range of symptoms, one of which is the so-called crimson tongue: a few days after the onset of the disease, the mucous membrane of the tongue becomes bright red and granular in appearance. Other signs of the disease look like this:
- fever;
- headache;
- malaise;
- small rash;
- angina;
- exfoliation of the skin in the final phase.
Treatment of scarlet fever most often takes place at home, while the patient is prescribed to remain in bed, drink plenty of warm liquids, and follow a gentle diet. Drug therapy includes, first of all, the use of penicillin-based antibiotics (Phenoxymethylpenicillin, Amoxicillin, Ampicillin and others). It is equally important to support the patient’s immunity through the use of vitamins C and B.
Note! In severe cases, if the patient requires hospitalization, intravenous administration of a glucose solution may be necessary to relieve symptoms of intoxication.
Causes of tongue redness
All existing causes of external changes in the language, including its color, can be divided into two groups. The first group of factors are easily solvable problems that do not signal internal disorders and are not a cause for concern on the part of parents. These include:
- consumption of coloring foods and drinks,
- eating too hot (cold) food;
- mechanical trauma from a brush, teeth, lollipop, etc.
The second one combines negative causes that are inextricably linked with pathological processes that are hidden or obvious in the child’s body:
- inflammation of the taste buds;
- any inflammatory processes caused by viruses or infection;
- intoxication of the body due to poisoning;
- taking medications (antibiotics);
- allergic reaction to food, medications.
- lack of vitamins and microelements.
Only a doctor can identify the true cause of changes in the color and texture of the tongue. Parents should not engage in self-diagnosis and self-medication; this will only mask the problem and complicate the doctor’s work.
Prevention
To avoid the reappearance of small red dots on the tongue, you must carefully follow a number of recommendations:
- Eliminating bad habits.
- Scrupulous personal hygiene of the oral cavity, as well as good quality toothpaste and brushes.
- Review your diet and get rid of fast food products that are rich in hot spices.
- Carbonated drinks should not be consumed, especially if they contain a large number of dyes.
- Strengthening the immune system.
- Periodic visits to the doctor.
- It is recommended to harden children, carefully choose a diet, and also exclude the intake of any allergen.
What diseases does a red tongue hide?
A red tongue can be a symptom of diseases of various etiologies, including:
- angina;
- flu;
- chickenpox,
- scarlet fever;
- stomatitis;
- glossitis;
- pneumonia;
- Kawasaki disease;
- gastritis;
- severe poisoning;
- renal failure;
- vitamin deficiency (vitamin B deficiency).
As you can see, the list of diseases is quite wide and requires visiting not only an otolaryngologist, but also, if necessary, other specialized specialists: dentist, endocrinologist, gastroenterologist, etc.
Kawasaki syndrome
The disease is complicated by the increased likelihood of damage to important blood vessels.
A serious disease unique to childhood is Kawasaki syndrome, which is an acute fever. The disease is complicated by an increased likelihood of damage to important blood vessels with subsequent thrombosis and rupture of the walls, which makes it deadly.
The cause of the syndrome has not yet been precisely studied, but the main hypothesis suggests a connection between the body’s immune response to an increase in the number of T-lymphocytes and the presence of antigens to staphylococci and streptococci.
The assumption that a child has this disease is based on prolonged (at least five days) fever, accompanied by any four symptoms from the following list:
- the tongue is red due to infection of the entire mucous membrane of the mouth and throat;
- redness of the eye sclera;
- erythema, peeling or swelling of the hands and feet;
- a rash on the body similar to measles, but without blisters;
- pronounced enlargement of the cervical lymph nodes.
It is impossible to completely cure a child of Kawasaki syndrome, so treatment is symptomatic and includes intravenous administration of immunoglobulins, the use of non-steroidal anti-inflammatory drugs and corticosteroids.
Geographical
If red spots and a white coating along their edges appear on the tongue, then this is a sign of a geographic tongue - desquamative glossitis. The disease is not inflammatory in nature and may indicate some hormonal disorders, worms and problems in the digestive system. Such spots do not have smooth outlines, they quickly change their location and do not bother the child in any way. They can be oval, round or have fancy shapes.
This disease lasts a long time and often goes away on its own after some time, even without specific therapy. Sometimes antiseptics, vitamins and drugs that accelerate tissue regeneration processes are used to treat geographic tongue. But most experts (for example, Dr. Komarovsky) believe that there is no need to treat geographic spots.
Higher medical education
- Abdominal surgery
- obstetrics and gynecology
- Allergology and immunology
- Angiosurgery
- Andrology
- Anesthesiology and resuscitation
- Bacteriology
- Biochemistry
- Valeology
- Laboratory doctor
- Gastroenterology
- Hematology
- Geriatrics
- Hyperbaric oxygen therapy
- Hirudotherapy
- Homeopathy
- Dermatovenereology
- Dermatocosmetology
- Pediatric abdominal surgery
- Pediatric allergology and immunology
- Pediatric anesthesiology and resuscitation
- Pediatric gastroenterology
- Pediatric hematology
- Pediatric gynecology
- Pediatric dermatology
- Pediatric cardiology
- Pediatric cardiology interventional
- Pediatric cardiac surgery
- Pediatric combustiology
- Children's physical therapy
- Children's drug addiction
- Pediatric neuropathology
- Pediatric neurosurgery
- Pediatric nephrology
- Pediatric general surgery
- Pediatric oncology
- Pediatric otorhinolaryngology
- Pediatric ophthalmology
- Pediatric pathological anatomy
- Pediatric plastic surgery
- Child psychiatry
- Child psychology
- Child psychotherapy
- Pediatric pulmonology
- Pediatric rheumatology
- Pediatric X-ray surgery
- Pediatric LUTS
- Children's dentistry
- Pediatric dentistry therapy
- Pediatric dentistry-surgery
- Children's forensic drug testing
- Child forensic psychiatric examination
- Pediatric audiology
- Pediatric toxicology
- Pediatric thoracic surgery
- Pediatric traumatology-orthopedics
- Pediatric transplantology
- Pediatric urology and andrology
- Pediatric physiotherapy
- Pediatric phthisiology
- Pediatric maxillofacial surgery
- Children's extracorporeal detoxification
- Pediatric endocrinology
- Pediatric endoscopy
- Pediatric infectious diseases
- Dietetics
- Immunology
- Infectious diseases
- Cardiology
- Interventional cardiology
- Cardiac surgery
- Clinical laboratory diagnostics
- Clinical pharmacology
- Combustiology
- Computed and magnetic resonance imaging
- Resortology
- Physiotherapy
- Radiation therapy
- Mammalogy
- Manual therapy
- Emergency and disaster medicine
- Medical biology
- Medical genetics
- Medical psychology
- Medical physics
- Medicinal chemistry
- Healthcare management
- Methodology
- Narcology
- Neuropathology
- Neurosurgery
- Neonatological surgery
- Neonatology
- Nephrology
- General practice
- general surgery
- Oncologist-gynecologist
- Oncology
- Otorhinolaryngology
- Ophthalmology
- Pathological anatomy
- Pediatrics
- Perfusionology
- Plastic surgery
- Proctology
- Occupational pathology
- Psychiatry
- Psychotherapy
- Pulmonology
- Radiology
- Rheumatology
- Radiology
- X-ray surgery
- Reflexology
- Sexopathology
- Ambulance and emergency medical care
- Social hygiene and health care organization
- Sports medicine
- Statistics
- Dentistry
- Dentistry-orthodontics
- Dentistry-orthopedics
- Dentistry-therapy
- Dentistry-surgery
- Sujok therapy
- Forensic drug testing
- Forensic psychological and psychiatric examination
- Audiology
- Therapy
- Therapy for teenagers
- Toxicology
- Thoracic surgery
- Traumatology-orthopedics
- Transplantology
- Transfusiology
- Urology
- Physiotherapy
- Phytotherapy
- Phthisiology
- Functional diagnostics
- Cytology
- Maxillofacial Surgery
- Expert histologist
- Expert thanatologist
- Extracorporeal detoxification
- Electrocardiography
- Endocrinology
- Endoscopy
White
In a baby, the appearance of white spots on the tongue most often indicates thrush - a fungal infection of the mucous membranes due to a decrease in immune defense in the body or when taking antibiotics. Such spots are located asymmetrically, can have a variety of sizes, and are often covered with a cheesy coating.
If a child shows signs of thrush on his tongue, then it is necessary to visit a pediatrician who will find out the reasons for its appearance. Delay in treatment can cause progression of the disease and inflammation of the mucous membrane, which will cause pain and discomfort in the child. You cannot try to remove the plaque on your own; this can lead to additional trauma. To eliminate such white spots, it is most often recommended to treat the child’s oral cavity with a weak solution of baking soda or ordinary brilliant green. In more severe cases and with relapse of the disease, it may be necessary to take antifungal drugs.