Candida test
Candidiasis is a disease caused by yeast-like fungi Candida, which can affect the skin, mucous membranes, and internal organs.
Candida fungi are ubiquitous - in soil, water, on vegetables and fruits, everyday items, household items, etc., etc. They are also present in the human body, in small quantities being part of the normal microflora.
The Candida fungus is a round or oval single-celled plant organism. Its wall is constructed in such a way that it reliably protects the microorganism from the effects of adverse environmental conditions and medications. The optimal temperature for Candida growth is from +20°C to 27°C. However, even at a body temperature of 37°C, mushrooms feel quite comfortable.
The genus of yeast-like fungi Candida has about 170 representatives. The most common of all fungi of this species is the species Candida albicans. In the human body, fungi can settle on the skin or mucous membranes - in the mouth, vagina, gastrointestinal tract, etc., without betraying their presence in any way. Candida especially “loves” tissues containing a lot of glucose or its compounds (the microorganism absorbs sugar very well), so candidiasis is often found in patients with diabetes.
The impetus for the development of a number of diseases caused by candida (for example, bacterial vaginosis or “thrush”, pneumonia in newborns, inflammation of the urethra, various purulent diseases, stomatitis, systemic candidiasis) can be factors that cause a malfunction of the immune system or depression its functions, for example:
- severe infectious diseases;
- HIV infection and other immunodeficiency conditions;
- oncological diseases;
- diabetes;
- use of new generation antibiotics;
- use of corticosteroid drugs;
- old age or childhood;
- pregnancy.
The development of a fungal infection occurs, as a rule, within the body itself (autoinfection) on the basis of fungi included in the normal microflora. However, infection can also occur from outside. With candidiasis, the properties of the fungus remain unchanged - only the body’s reaction to it changes (the level of local protection decreases). Candidiasis can occur in one of two forms:
- superficial, in which the skin and mucous membranes are affected;
- deep, with possible damage to several body systems, internal organs, and penetration of the fungus into the blood.
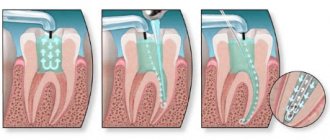
The parasitic fungus attaches to the epithelial cells of the mucosa and penetrates into the thickness of the tissue. The degree of deepening can vary from damage to surface cells to the entire thickness of the mucosa. The body resists the fungus, which can lead to dynamic equilibrium. The essence of this phenomenon lies on the part of the fungus in the desire to go deeper and the impossibility of doing this, and on the part of the body - to force out the uninvited guest, which is also not crowned with success. This balance can be maintained for years. As a result of displacement, either recovery or relapse of the disease occurs. Individuals with immunodeficiency may develop both forms of infection. In an organism with a normally functioning immune system, only superficial candidiasis is observed.
Depending on the lesion, the following types of candidiasis are distinguished:
- candidiasis of the mucous membranes of the oral cavity;
- urogenital candidiasis (fungal infection of the mucous membranes and skin of the genitourinary organs);
- candidiasis of the skin and its appendages (sweat and sebaceous glands, hair, nails);
- visceral candidiasis (affecting internal organs and systems, causing their inflammation);
- Chronic generalized candidiasis (total damage to the body that occurs in the absence of adequate therapy, with the subsequent transition of the disease to a chronic form, and the possible development of candidal sepsis in the absence of further treatment).
Candidiasis of the skin and its appendages is characterized by the formation of lesions in large folds, inguinal cavities, under the mammary glands, and smaller interdigital folds. In people suffering from severe pathologies, the fungus can affect the palms, feet, smooth skin of the limbs and torso. In large folds, under the influence of fungi, small bubbles are formed, which burst to form ulcers. Small ulcers, gradually merging with each other, form one large erosion of a dark red color, which has an irregular shape and is framed by a strip of exfoliating skin. In open areas, red spots, flaky in the middle, are formed, occasionally framed by small bubbles.
Between the fingers of the hands (usually between the 3rd and 4th or 4th and 5th), areas affected by candida appear most often in people who have been in contact with water for a long time. The formation of lesions is accompanied by itching, burning, the appearance of cracks and dark red erosions. Foci of candidiasis on the palms and soles are a flaky surface with detachments of the upper layer of skin or keratinized skin of a dirty brown color, cut by furrows. If candidiasis affects the nails, then swelling and redness appear around the nail, thickening of the periungual fold, thinning and peeling of the skin are observed (you can find out about the study of skin and nails affected by the fungus in the description of item 718 in the “Tests” section on the medical website).
The first place among all areas affected by gastric candidiasis is the oral cavity. One of the pathologies caused by the fungus is candidal stomatitis. It most often affects newborns and people with dentures. A typical sign of the disease is the appearance of a characteristic white cheesy coating, as a result of which the disease has another name, better known to the general public - “thrush”. The onset of candidal stomatitis is characterized by the appearance of swelling of the mucous membranes of the tongue, gums, cheeks and minor areas of redness on them. As the disease progresses, the lesions enlarge and merge into large areas of the damaged surface. A cheesy coating appears on them, which first covers small areas, and then merges, forming films of various configurations and sizes. Once the films are removed, areas of a shiny, dark red surface are revealed underneath. When candidal stomatitis becomes chronic, the plaque becomes coarser and denser. It fits tightly to the affected area, and after removal it leaves erosion underneath. Infection of the tongue with fungus is manifested by an increase in its size, the formation of deep grooves on it with a yellow-white coating on the bottom. When the pathological process leaves the oral cavity, a candidiasis can form, which is an open wound or crack of a grayish-white color and has a clearly defined contour. With candidiasis of the lips, peeling is observed with the formation of grayish plates, thinning of the skin and the formation of folds, and the appearance of a bluish border along the contour. Oral candidiasis does not cause increased body temperature or inflammation of the lymph nodes.
Candidiasis can be not only superficial, but also visceral (i.e., affecting internal organs and systems of the body). One of its forms is gastric damage. Typically, a favorable factor for the onset of gastric candidiasis is peptic ulcer. Also, the fungus can develop intensively when the acidity of gastric juice is low. To create colonies, the fungus chooses a place with ulcerated or erosive mucosa, slowing down the healing of wounds, causing pain and bleeding.
The development of intestinal candidiasis usually occurs with long-term use of modern antibacterial agents. This pathology can be identified by studying its microflora. Symptoms of intestinal candidiasis may include bloating, diarrhea, and abdominal discomfort.
Urogenital candidiasis (fungal infection of the genitourinary system) in women causes vulvovaginitis (inflammation of the mucous membrane of the female genital organs - vulva and vagina), and in men - a combination of balanitis and urethritis (inflammation of the glans penis and urethra). Thrush of the female genital organs, as it turns out, quite often occurs due to the excessive use of “advances of civilization,” in particular, synthetic underwear and pads, which create a “greenhouse effect” that causes disruption of the structure of the outer layers of the skin. Signs of thrush are curdled discharge from the genital tract, the appearance of red spots with a whitish coating in the vagina and its vestibule, and sometimes the appearance of small blisters around the affected area. All this is accompanied by burning and itching, intensifying in the afternoon and at night, during menstruation, during long walking, after water procedures.
Symptoms of balanitis in men are itching, redness of the head of the penis, and the formation of erosive areas on it covered with a white coating.
The development of chronic generalized candidiasis occurs in children when the functioning of the immune system, the functionality of the thyroid and pancreas is disrupted. Initially, the mucous membranes of the oral cavity are affected, then the infection spreads to the lips, scalp, skin, nails, and genitals. Externally, the affected areas are similar to the manifestation of psoriasis (a non-infectious dermatological disease of an inflammatory nature) or pyoderma (a purulent skin lesion that occurs when pyogenic cocci are introduced into it). The next stage in the development of the disease may be damage to the eyes and internal organs - heart, kidneys, lungs. An even deeper deepening of the fungus can cause damage to blood vessels and its entry into the bloodstream, which will cause it to spread throughout the body and the formation of new areas of infection. In addition, destruction of tissue by the fungus can cause bleeding. The danger of bleeding is especially high when the gastrointestinal tract is affected. Fungal sepsis (i.e., fungus entering the blood) quite often leads to the death of the patient. Since the fungus is a foreign organism, large amounts of it can cause severe, non-standard forms of allergies. During pregnancy, intrauterine infection of the child can occur, and in extreme cases, spontaneous abortion.
Medicine knows cases of spontaneous healing from candidiasis. However, you should not hope for this - the disease must be treated. With an unscrupulous approach to the treatment of infection, there is a high probability of its transition from acute to chronic form. In this case, the dynamic balance mentioned above is the easiest version of the disease. However, the likelihood of such a situation is small: having lost ground once, the body will no longer be able to resist the attack of the fungus, which will entail its deeper penetration, tissue damage, and degenerative changes in them. This form of candidiasis bears little resemblance to thrush - rather, it resembles a bacterial infection, allergic or autoimmune diseases. With deep penetration into the body, candida becomes invulnerable to the action of external antifungal drugs, and in some cases, even to systemic medications.
Everyone knows that a disease is easier to prevent than to treat. Prevention of candidiasis should be carried out, first of all, for people at risk, which include:
- patients who have been taking modern antibacterial agents for a long time;
- people who have been on long-term immunosuppressive therapy (treatment to suppress unwanted immune responses in the body);
- persons who have been taking hormonal drugs for a long time;
- patients who have been diagnosed with immunodeficiency conditions.
All these categories of people should be promptly examined and, if a fungal infection is detected, subjected to preventive treatment using antifungal drugs.
Since thrush is sexually transmitted, if it is detected in one of the partners, treatment must be carried out on both partners at the same time. The use of antibiotics should be strictly under the supervision of a physician. To increase resistance to infection, it is necessary to engage in sports and hardening. To prevent intestinal dysbiosis, it is necessary to create a balanced diet with the obligatory inclusion of fermented milk products containing bifidobacteria and lactobacilli, pickled vegetables, cereal porridges containing fragments of their shell, and also undergo a course of treatment with drugs that restore intestinal microflora. Items used in everyday life must be clean, and clothing and linen must not create a “greenhouse effect.”
Candidiasis is diagnosed by the presence of characteristic symptoms in the patient, as well as through a number of laboratory methods:
- microscopic detection of fungus in the test sample;
- bacteriological research with inoculation of material on nutrient media in order to clarify the type of infectious agent;
- detection of specific DNA fragments of the infectious agent using real-time polymerase chain reaction (PCR test);
- serological methods (i.e., by detecting antibodies to the infectious agent in the blood serum; high titers of antibodies indicate the fungal nature of the disease).
This test involves a microscopic examination of scrapings from the mucous membranes, urine and feces for the presence of Candida yeast fungus in the biomaterial.
What is it and why?
The oral cavity of every person is very densely populated with microorganisms.
Most of them are harmless saprophytes, among which there are cocci and bacilli.
There are even non-pathogenic spirochetes.
Our body has learned to coexist safely with them, and we simply do not notice them.
But such prosperity does not always happen.
Problems arise when foreign microorganisms enter the oral cavity.
For example, pathogens of sexually transmitted infections that thrive on the mucous membranes of the mouth and genitals.
The list of microbes that are capable of such a change in habitat is quite wide:
- Trichomonas
- treponema pallidum
- human papillomaviruses (HPV)
- herpetic group viruses
- gonococci
- chlamydia
In principle, this list can include almost all STD pathogens.
A smear helps to identify them in the mouth.
References
- Khaitovich, A.B., Voevodkina, A.Yu. Microbiome and its impact on human health. Crimean Journal of Experimental and Clinical Medicine, 2021. - No. 1. - P. 61-70.
- Krasnova, E.I., Khokhlova, N.I., Evstropov, A.N. and others. Streptococcal infection of the oropharynx: approaches to diagnosis and treatment. Infectious diseases, 2015. - No. 4. - P. 30-36.
- Li, N., Ma, W., Pang, M. et al. The commensal microbiota and viral infection: a comprehensive review. Frontiers in immunology, 2019. - Vol. 10.
Diagnostic value of mouth swab
At its core, it is completely, 100% analogous to a urogenital smear.
The only difference is where the diagnostic material is taken from.
A mouth smear helps determine the spectrum of oral microflora in the person being examined, regardless of gender.
This method refers to laboratory-instrumental techniques and performs one task: obtaining diagnostic material for a detailed study of microflora.
Samples obtained using a mouth swab are examined in different ways:
- microscopy of native material and fixed, stained smear
- bacteriological examination (culture)
- immunological studies
- molecular genetic
The main thing is to correctly and accurately collect diagnostic samples.
But before you collect them, you need to determine who needs it.