Where does the feeling of a lump in the throat come from?
The sensation usually occurs on the front of the neck.
The patient is concerned about the feeling of a lump in the throat, soreness, numbness and a feeling of a foreign body in the respiratory tract. There is a desire to swallow saliva, but a spasm that causes a feeling of a lump in the throat prevents this from happening. In many patients, the lumen of the esophagus narrows, which makes it impossible to eat normally - the bolus of food does not move towards the stomach, causing pain, salivation and vomiting.
What is a lump in the throat?
Many patients are bothered by a slight feeling of fullness in the throat, which does not cause severe discomfort or difficulty breathing. The feeling of a lump in the throat may occur for just a few seconds, or may last for several days in a row. However, the sensations can be more intense: a spasm of the larynx appears, which makes it difficult to breathe and causes a feeling of fear of death. This syndrome was described by Hippocrates, calling its nature “hysterical”³.
Feeling of a lump in the throat with VSD
Very often you can find in people suffering from VSD the sensation of a lump in the throat. It's one thing when there is a logical, although there may be an unpleasant and frightening explanation, for example, a tumor or severe inflammation that causes a narrowing of the larynx. But what to do in cases where there is a lump, but there are no reasons for it, and turning to a variety of specialists gives the same result: the person who contacts them has no reason to feel a lump.
What are the symptoms of a lump in the throat?
This symptom of VSD, like a lump in the throat, appears completely suddenly. One fine morning there is a feeling that something is interfering, preventing you from swallowing and breathing deeply as usual. At the same time, five minutes ago everything was in order, but any ordinary or everyday situation, accompanied by a little excitement, an increase in blood pressure and an increase in heart rate - and now, the feeling that someone is squeezing the neck. All you have to do is drink a sedative, come to your senses a little, and your condition will return to normal. But in any other stressful situation, the feeling of a lump in the throat appears again.
Unpleasant sensations can be either constant or periodic. At the same time, the sensations may differ from person to person; it may be a tickling sensation, a tingling sensation, a feeling of squeezing, or the inability to swallow, whether it is saliva or solid food.
Sometimes the feeling of a lump can develop into a state in which a person may realize that he has forgotten how to swallow and cannot do it. Then it comes to a panic attack. So, over time, a fear of swallowing in general and eating solid food may develop.
Causes of a lump in the throat with VSD
Vegetative-vascular dystonia in itself is a nervous disorder; suffering from VSD, a person is constantly in panic and fear of something. This, in turn, is triggered by the release of large doses of adrenaline into the blood.
Which part of the body the adrenaline will choose to express itself is not clear. For some, this manifests itself in pain in the chest area, for others, the gastrointestinal tract suffers, and for others, they experience spasms of the laryngeal muscles, which is the very sensation of a lump in the throat.
It is worth remembering that no other disease, for example, an enlarged thyroid gland, osteochondrosis or aneurysm, gives symptoms similar to a coma, no matter what anyone says.
What could be bothering your throat?
People who first feel a lump in their throat first think of the worst, of course, cancer. What else could create such sensations of interference if not a tumor? And the more panic moods grow in a person, the stronger the lump is felt.
You need to know that the most important difference between a lump in the throat during VSD and any serious disease of the larynx, esophagus or other respiratory organs is that during sleep the lump is not felt at all. When I wake up, everything is fine too. But as soon as you get up and feel more energetic, the sensations return. The whole point here is that until the brain woke up, the body felt good, but as soon as the brain returned to working condition, it remembered that there should be a lump, and the patient felt it again.
It is the normal state of the throat in the first five minutes after waking up that should assure a person that the issue here is not some mythical disease, but the state of the nervous system.
How to treat a lump in the throat?
In fact, it is very difficult for any person suffering from VSD to admit to himself that the problem is not a disease at all, but a disorder of the nervous system. Treatment for coma is the same as for VSD therapy.
- Taking psychotropic medications that reduce panic attacks to a minimum and have a calming effect in a dosage that is relevant for a particular patient.
- An attempt to come to terms with the fear of death and liberation from oppressive terrible thoughts. You can seek advice on this issue from a psychotherapist, but you will have to work on yourself on your own.
The feeling of a lump in the throat will not go away on its own and will poison your life.
He needs to be treated. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Causes of a lump in the throat
The feeling of a lump in the throat can occur spontaneously during a certain emotional state of the patient: when he is in a stressful situation or, for example, feels proud, sad, etc. A lump in the throat can also occur due to purely physiological reasons, for example, when sitting for a long time with your face down.
Other reasons include the appearance of a lump in the throat due to various pathologies, each of which deserves separate consideration.
Scheme 1. Causes of the sensation of a lump in the throat. Source: Medportal
Nervous stress
In most cases, the sensation of a lump in the throat occurs as a result of nervous tension. According to the International Classification of Diseases, 10th revision (ICD-10), the feeling of a lump in the throat belongs to the group of neurotic and somatoform disorders associated with stress.
It occurs in people prone to depression or suffering from nervous tension (both at work and at home). Sometimes in women this symptom occurs during premenstrual syndrome against the background of exacerbation of anxiety and irritability.
Com and psychosomatics
In medicine there is such a thing as psychosomatics - it means a close relationship between a person’s psychological state and the health of his body. Often, a lump is attributed specifically to psychosomatic manifestations. In this case, the feeling is of short duration - as a rule, the symptom goes away within a few minutes or even seconds.
Gastroesophageal reflux disease
When a patient experiences reflux (the release of stomach contents back into the esophagus), gastric juice, which includes hydrochloric acid, irritates the walls of the esophagus, which causes spasm and a feeling of a lump in the throat¹.
Skeletal muscle diseases
Patients suffering from skeletal muscle diseases such as myasthenia gravis and myotonia may experience spastic phenomena (spasms) in the throat muscles, which provoke a foreign body sensation.
Zenker's diverticulum
In a patient, in the initial part of the esophagus, which borders the pharynx, a protrusion of the mucous membrane occurs through the smooth muscle of the esophagus. In this case, the sensation is no longer subjective, since the protrusion itself acts as a foreign body, that is, a coma.
Oncological neoplasms
As in the previous case, the sensation of a foreign body is no longer subjective. With neoplasms in the throat area, the feeling of a coma is not paroxysmal in nature, as with nervous overstrain - it haunts the patient constantly.
Eosinophilic esophagitis
This disease is an inflammation of the walls of the esophagus, most often occurring as a consequence of allergic reactions. A lump in the throat occurs due to pain in the esophagus, which is caused by inflammation and reflux.
Osteochondrosis
This disease is accompanied by degenerative changes in the cartilage and bone tissue of the spine. This, in turn, leads to compression of the radicular nerves, which are responsible for the innervation of the larynx and pharynx, that is, their connection with the central nervous system. As a result, paresthesia may occur - distorted sensations, which include a lump in the throat.
Thyroid diseases
The feeling of fullness and the presence of a foreign body in the throat often occurs with diffuse or nodular goiter. With thyroiditis, the tissues of the thyroid gland become inflamed, so the feeling of a lump is accompanied by pain.
ENT diseases
Due to inflammation with sore throat, tonsillitis and pharyngitis, a sensation of a lump in the throat may also occur. In addition to this, the patient is also bothered by a sore throat and painful sensations.
Sjögren's syndrome
This is a disease of autoimmune origin, in which the body perceives its own cells as foreign and produces antibodies that attack healthy tissue. This, in turn, leads to inflammatory phenomena.
Sjögren's syndrome affects the lacrimal and salivary glands. The feeling of a lump in the throat occurs as a result of inflammation and dryness in the mouth and larynx. Patients usually complain of soreness in the larynx and that a lump in the throat prevents them from swallowing food. The disease develops mainly in women over 30 years of age.
Allergy
In some people, a feeling of coma occurs as a result of allergic reactions due to swelling of the throat.
Food poisoning
In this condition, the patient often experiences spasms of the gastrointestinal tract and esophagus. This may make it feel like a lump in your throat is making it difficult to swallow.
Important! Most often, complaints of a lump in the throat come from adult patients aged 41–50 years. However, the feeling of a lump in the throat is not always associated with any disease. Doctors note that during a medical examination, 46% of practically healthy patients complained of this feeling.
Swallowing disorders: causes, “coma in the throat” syndrome
The swallowing process is repeated periodically, not only while awake, but also during sleep. Like breathing, this process often occurs involuntarily. The average frequency of swallowing is 5-6 times per minute, however, with concentration or strong emotional arousal, the frequency of swallowing decreases. The swallowing process is a clear sequence of muscle contractions. This sequence is provided by a region of the medulla oblongata called the swallowing center.
Swallowing difficulties can develop without a person noticing. Impaired oral feeding, weight loss, a significant increase in the time it takes to swallow food - all this can be a manifestation of a violation of swallowing function. Signs of difficulty swallowing may include:
- throwing back the head or moving the head from side to side, helping to move the food bolus;
- the need to wash down food with water;
Despite pronounced difficulties in swallowing, the tongue and the muscles that lift the velum palatine can function normally.
A swallowing disorder is medically called dysphagia.
What diseases cause difficulty swallowing:
Swallowing disorders can lead to serious consequences:
- exhaustion of the body, weight loss;
- cough during and after swallowing, constant choking;
- feeling of lack of air while swallowing;
- pain and shortness of breath;
- development of pneumonia;
Depending on the causes of swallowing disorders, there are:
- Mechanical (organic). A similar violation can occur when the size of a piece of food and the lumen of the esophagus do not match.
- Functional. This type of swallowing difficulty occurs when peristalsis and relaxation are impaired.
Both mechanical and non-mechanical problems can occur for a variety of reasons. Organic (or mechanical) swallowing disorder is associated with direct external or internal pressure on the esophagus. In such a situation, the patient says that it is difficult for him to swallow food. There may be several reasons for mechanical impact:
- Blockage of the esophagus by any foreign body or food;
- Narrowing of the lumen of the esophagus, which can occur due to:
- edema resulting from an inflammatory process (stomatitis, sore throat, etc.);
- damage or scars (burns from taking pills, scars from operations or after inflammation);
- malignant and benign formations;
- stenosis;
3. External pressure may be a consequence of swelling of the thyroid gland, compression by blood vessels, etc.
Functional swallowing disorders include disorders associated with impaired muscle function. Violations can also be divided into 3 groups:
- Disorders associated with tongue paralysis, brain stem damage, sensory disturbances, etc.
- Disorders associated with damage to the smooth muscles of the esophagus. Such violations lead to weakness of contractions and impaired relaxation.
- Disorders associated with diseases of the muscles of the pharynx and esophagus;
Other causes of difficulty swallowing include: Parkinson's disease, parkinsonism syndrome, inflammation of the esophageal mucosa and connective tissue diseases.
“Lump in the throat” syndrome The feeling of a lump in the throat (globus pharyngeus syndrome) is one of the most common complaints when visiting an otolaryngologist. During their lifetime, approximately 45% of people experience this sensation. This syndrome began to be studied as one of the manifestations of hysteria, but during the study it became clear that only a part of the cases were due to psychiatric reasons.
There are several reasons for the sensation of a lump in the throat:
- There really is something in the goal and this object interferes with swallowing. The sensation of a lump in the throat in this case can be caused by swelling of the uvula of the soft palate, a tumor or cyst, or an enlarged palatine or uvular mendala. The cases described above are quite rare and can easily be excluded during examination at a doctor's appointment.
- There is a feeling of a “lump in the throat”, but there are no objects directly in the throat that could interfere with swallowing. These are the most common cases. Most often, this sensation is caused by reflux disease. Reflux is the backflow of stomach contents into the esophagus and further into the throat. Muscle spasm in the throat, which causes the feeling of a “coma,” is provoked by gastric contents (the acidic contents of the stomach burn the mucous membrane of the esophagus and throat). Also, the symptom of “coma in the throat” can be accompanied by chronic pharyngitis.
- Psychological factors. Often the appearance of the “coma in the throat” syndrome is facilitated by stressful situations, a state of strong excitement or fear.
The “globus pharyngeus” syndrome has not been fully studied to date, but in most cases it does not pose a threat to human life, and the causes that caused it are quite easy to eliminate. However, to determine the exact causes and prescribe timely treatment, an in-person examination by a doctor is necessary.
If you have difficulty swallowing or feel a lump in your throat, get a consultation or make an appointment on the Clinical Brain Institute website.
What to do if you have a coma in your throat? How to fix it?
The feeling of a lump in the throat makes you nervous.
Photo Source: Krakenimages.com / Depositphotos It is important to try to determine under what circumstances this feeling occurs and how long ago it was noticed. Even before going to the doctor, you can use the instructions below.
How to make sure that a lump in your throat is not a consequence of your lifestyle?
- Determine if there have been any stressful situations at work or at home recently, and try to minimize them.
- Try to understand if there is tension in the neck muscles due to a long sitting position facing down. If your job requires a sedentary lifestyle, you need to take short breaks every 15-20 minutes. In this case, it is advisable to walk a little and make several turns of the head alternately to the right and left.
- Fitness activities can also contribute to the appearance of a lump in the throat. You need to reduce physical activity and see if the feeling goes away.
- You need to temporarily give up smoking and alcohol and not strain your vocal cords (do not sing, do not shout).
- You should switch to fractional meals in small portions at least 5 times a day. Avoid fried, salty, smoked and spicy foods. It is not recommended to lie down or exercise after eating.
- See if the sensation arises in one specific place. This may be the result of an allergic reaction, such as to dust or wool. In this case, you need to limit contact with the allergen.
- Female patients should pay attention to whether this sensation appears exclusively before the onset of the menstrual cycle against the background of a heightened emotional state.
If the tips described above do not help you cope with the feeling, you should consult a specialist.
Lump in the throat
The appearance of a lump in the throat
is a very common problem. Many patients browse the Internet every day to understand why they have a lump in their throat and what to do in such a case. In the practice of an endocrinologist, patients who seek consultation regarding a lump in the throat are encountered almost every day.
What diseases can cause such sensations? A lump in the throat occurs with diffuse enlargement of the thyroid gland, the appearance of thyroid nodules, thyroid tumors, inflammation of the thyroid gland (thyroiditis), tumors of the anterior surface of the neck, tumors of the esophagus, neck abscesses, osteochondrosis, neurosis.
Which doctor should I contact?
Since the causes of a lump in the throat are different, you can first consult a general practitioner. Based on complaints and physical examination data, he will prescribe appropriate diagnostic tests and refer the patient to a specialized specialist.
You can also try to determine on your own when this unpleasant feeling arose and what its symptoms are, and then visit the appropriate specialist:
- neurologist - if the feeling occurs against the background of fatigue, insomnia or nervous stress, is paroxysmal in nature, and its duration does not exceed several minutes;
- otolaryngologist - if, in addition to the sensation of a foreign body, the patient is bothered by pain when swallowing, redness of the throat or fever;
- gastroenterologist - the patient is worried about heartburn, sour belching, a feeling of heaviness after eating, painful sensations in the stomach or esophagus, and the feeling does not go away for several days;
- endocrinologist - if the patient also experiences symptoms such as hoarseness, attacks of dry cough, decreased performance and libido, difficulty breathing, attacks of dizziness, decreased or increased salivation, gastrointestinal disturbances;
- oncologist - for prolonged weakness, increased fatigue, weight loss and a feeling of fullness in the neck that does not go away within several days;
- a vertebrologist or neurologist - if the patient is also concerned about pain in the spine, headaches, blurred vision, numbness of the extremities, poor sleep, a feeling of pins and needles in the upper and lower extremities.
Psycho-emotional disorders and lump in throat
But most often a lump in the throat is caused by psycho-emotional disorders. Occurs after acute or chronic stressful situations, unresolved problems and protracted grievances. Here, as a rule, there is a feeling of anxiety, restlessness, possible sensations of lack of air and panic attacks, sleep disturbances, and mood swings . Then a lump in the throat can be regarded as the first symptom of an anxious or depressive state. In such cases, treatment should be carried out comprehensively by a neurologist and psychiatrist.
But in order to be sure that the lump in the throat is exclusively psychogenic in nature, it is necessary to exclude diseases of all other organs that can give the same sensations. In addition, a combination of several diseases is possible. For example, we may have GERD and chronic pharyngitis along with an anxiety disorder, so we need to treat all three diseases in parallel.
Diagnosis of a lump in the throat
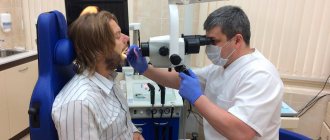
Instrumental diagnosis of a lump in the throat.
Source Photo: macniak / Depositphotos Diagnostic tests used for PCG depend primarily on the data obtained from collecting complaints and the characteristics of clinical symptoms - all of this together allows the doctor to make a preliminary diagnosis.
To confirm this diagnosis, as well as for the purpose of differential diagnosis (that is, excluding other pathologies with a similar clinical picture), the doctor prescribes a set of diagnostic tests. However, there is no uniform examination tactic. When prescribing tests, the doctor sets himself the task of excluding pathologies - tumors, ENT pathologies, changes in the volume of the thyroid gland and others.
Investigations for coma in the throat
Research methods depend on the cause. The simplest situation is with nervous stress - the doctor, based on the examination data and the patient’s complaints, will be able to get an idea of the mental state of his patient. In other cases, the patient may be prescribed blood tests, bacteriological cultures, ultrasound, MRI, radiography and other studies - not necessarily at the same time, it all depends on the preliminary diagnosis.
Blood tests
The doctor usually orders one or more tests. Depending on the type of study, the patient’s blood is taken from a finger or from a vein.
General analysis
The most common blood test, for which blood is taken from a finger (less commonly, from a vein). This study allows you to get an idea of the level of hemoglobin, red blood cells, platelets, white blood cells and ESR. If any of these indicators deviate from the norm, you can determine:
- the presence of inflammatory processes,
- anemia,
- blood clotting disorder.
The study is carried out in the morning on an empty stomach. You should not drink alcohol 2-3 days before the test, and a few hours before the test you should refrain from smoking.
Testing for tumor markers
As can be understood from the name, this test is prescribed when the development of tumor processes is suspected, when the patient experiences a constant increase in body temperature, pain, weakness, loss of appetite and weight loss. Tumor markers are a special type of proteins that are secreted by tumor cells.
Analysis to determine TSH levels
The level of thyroid-stimulating hormone (TSH) increases or decreases when the thyroid gland is not functioning properly. The basis for prescribing this study, in addition to the feeling of a lump in the throat, may be changes in appetite, nervousness, sleep disturbances, and deterioration in the condition of hair and skin. In rare cases, TSH levels increase in pregnant women.
IgE test
The study is aimed at identifying the level of IgE, that is, immunoglobulins E, which are antibodies whose level in the blood plasma of healthy people is very low. However, with allergic reactions and eosinophilic esophagitis, it increases.
Blood sampling for the above studies is carried out from a vein. A week before the test, it is advisable to limit physical activity and alcohol intake. The test is taken on an empty stomach - at least 8 hours must pass between the time of blood sampling and the last meal. It is important to refrain from smoking 1–2 hours before the test.
Sowing for microflora
Prescribed for inflammatory diseases of the throat. . The purpose of culture is to identify the causative agent of the infectious process and determine its sensitivity to antimicrobial drugs. The procedure is short and painless: the doctor uses a sterile swab to make a swab from the throat. There is another way: the patient rinses his mouth with a saline solution, and then spits it into a sterile container.
X-ray of the spine
This hardware test is prescribed to a patient if osteochondrosis is suspected. Using an X-ray of the spine, the doctor gets an idea of the condition of the bones and intervertebral joints. If an intervertebral hernia is suspected, an MRI may be prescribed as an additional study.
Esophagoduodenoscopy
This is an endoscopic examination of the esophagus, which is prescribed for suspected eosinophilic esophagitis and gastroesophageal reflux disease. The patient swallows a thin endoscope, with which the doctor evaluates the condition of the esophagus. In addition, during esophagoscopy, if necessary, a biopsy sample (a small fragment of tissue) is taken for histological examination. The procedure is unpleasant, but short. It causes the greatest discomfort in patients with a pronounced gag reflex. You should refrain from eating 6–7 hours before the test.
Salivary gland biopsy
Used in the diagnosis of Sjögren's syndrome. Biomaterial is collected not only from the salivary glands, but also from the inner mucous membrane of the cheeks. Using a syringe with a thin long needle, a puncture is made and biomaterial is collected for subsequent histological examination. This diagnostic procedure is performed under ultrasound guidance using local anesthesia. It is prescribed relatively rarely, since in most cases a blood test for autoantibodies allows a specialist to confirm or refute a preliminary diagnosis.
Ultrasound of the thyroid gland
Prescribed for the diagnosis of diffuse goiter, thyroiditis and other pathologies of the thyroid gland. This is an absolutely painless examination that does not require special preparation from the patient: you can eat, exercise, and even smoke before the ultrasound.
Contrast radiography of the esophagus
This study is relevant when diagnosing Zenker's diverticulum. With its help, the specialist gets an idea of the localization of the protrusion, as well as its size and shape. Before the x-ray, the patient is asked to drink a glass of barium suspension to improve contrast. This diagnostic procedure requires special preparation: you should not eat food 6–7 hours before the test.
Treating a lump in the throat
Lack of stress is an important fact when treating a lump in the throat.
Source Photo: IgorVetushko / Depositphotos After clarifying the diagnosis, the specialist prescribes a comprehensive treatment for the disease that causes the sensation of a lump in the throat. Therapeutic measures combine an impact on both the root cause of the disease and the elimination of associated symptoms.
Nervous tension
First of all, it is necessary to eliminate the cause of stress. If it is due to the specifics of the job, the patient is recommended to move to a position associated with less nervous tension. It is important to normalize your sleep schedule (at least 8.5 hours a day). If necessary, the doctor prescribes sedatives, antipsychotics and antidepressants.
Gastroesophageal reflux disease
It is recommended to limit the consumption of alcohol and confectionery products to prevent weakening of the lower esophageal sphincter tone. For the same purpose, it is advisable to quit smoking. Among medications, antacids are recommended, that is, drugs that reduce the secretion of gastric juice (hydrotalcite, omeprazole).
Skeletal muscle diseases
Priority treatment methods are massage, physical therapy and physiotherapy (electrophoresis, paraffin therapy). It is important to avoid hypothermia and ensure regular physical activity. In severe cases, the doctor may prescribe immunosuppressive therapy (prednisolone, cyclophosphamide, human immunoglobulin).
Zenker's diverticulum
In the initial stages, you can do without surgery: the patient should switch to fractional meals (at least 5 meals a day). You should also give up the habit of lying down after eating. In later stages, surgical treatment is indicated. This is done in two ways:
1. Classic surgical. The most common method in which the protrusion is corrected and sutured to prevent recurrence.
2. Endoscopic. This technique is also known as intraoperative video endoscopic transillumination. The operation is performed through an endoscope without tissue dissection. The advantage of endoscopic correction of protrusion is that after this manipulation the patient is left with no scars².
Oncological neoplasms
The main method is surgical removal of the tumor. Radiation therapy is used as an adjuvant treatment to destroy cancer cells. Chemotherapy is used to prevent relapses. As part of drug treatment, targeted therapy is prescribed, which is aimed at the targeted destruction of cells that provoke malignant processes.
Eosinophilic esophagitis
First of all, it is necessary to exclude highly allergenic foods (milk, eggs, seafood, nuts). Local corticosteroids, which are available in the form of sprays (fluticasone, budesonide), are also indicated. They are sprayed into the mouth and then swallowed.
To reduce the production of gastric juice, H2-histamine blockers (ranitidine, nizatidine) are prescribed. To increase the tone of the esophageal sphincter, prokinetics (metoclopramide, domperidone) are indicated.
Osteochondrosis
As with muscle diseases, the main treatment is massage and physical therapy. It is very important not to neglect regular physical therapy sessions. If necessary, the course of treatment is supplemented with non-steroidal anti-inflammatory drugs, vasodilators and chondroprotectors - medications that help improve the condition of cartilage and joints.
Thyroid diseases
As part of drug therapy, propylthiouracil and thiamazole are indicated. The action of these drugs is aimed at improving the functional state of the thyroid gland. In severe cases of the disease, the doctor prescribes glucocorticoids (prednisolone). For diffuse and angular forms of goiter, preference is given to surgical treatment. The patient also needs to give up bad habits and normalize sleep (sleep at least 8.5 hours a day).
ENT diseases
One of the main mistakes made by patients suffering from tonsillitis or pharyngitis is self-treatment using folk remedies. For these diseases, the use of antibiotics (penicillins and cephalosporins) is indicated. In addition, you should gargle with antiseptic solutions every hour. It is strongly recommended to quit smoking, alcohol and spicy foods for the entire period of treatment.
Sjögren's syndrome
To date, no pathogenetic treatment has been developed. This means that therapeutic measures for Sjöngren's syndrome are aimed at eliminating the symptoms, and not the cause of the disease itself. To relieve dry mouth that makes swallowing difficult, drinking frequently and chewing sugar-free gum are recommended. To enhance salivation, pilocarpine and cevimeline hydrochloride can be used (these drugs are contraindicated in patients with glaucoma and bronchospasm). It is also important to avoid taking antihistamines, which can worsen dry mouth.
Allergy
First of all, it is necessary to identify the allergen and eliminate all contact with it. The patient is prescribed a hypoallergenic diet (fried, smoked, salty, canned foods, chocolate, citrus fruits are excluded from the diet) and regular good sleep. Wet cleaning of the house must be done at least once every 2 days. If possible, you should get rid of carpets and curtains that accumulate dust. The patient is advised to take folic acid to increase the body's defenses. The phenomena of sensitization (increased sensitivity to allergens) are eliminated by antihistamines based on chloropyramine, cetirizine and fexofenadine.
Food poisoning
For mild to moderate poisoning, help is allowed at home. First you need to drink 1-2 liters of pale pink potassium permanganate or a 2% solution of baking soda. This will help induce vomiting and provide gastric lavage. Activated carbon is used to remove toxic substances from the intestines (at least 2 tablets per 10 kg of body weight). In severe cases, when these measures do not give the expected result, it is recommended to consult an infectious disease specialist.
Laryngopharyngeal reflux in gastroenterological practice
Gastroesophageal reflux disease (GERD) is one of the most common pathologies of the gastrointestinal tract. At the International Congress of Gastroenterology, held in Montreal in 2005, a unified definition of the disease, a description of symptoms and a classification of the disease were developed, which formed the basis of the Montreal Consensus [1]. The Consensus divides the clinical manifestations of GERD into esophageal and extraesophageal syndromes. The presence of reflux-associated symptoms in the absence of damage to the esophageal mucosa is regarded as esophageal syndrome, manifested solely by symptoms, and in the presence of damage to the esophageal mucosa - as esophageal syndromes with damage to the esophagus (complications). Extraesophageal syndromes were divided, in turn, into syndromes whose connection with GERD has been established, and syndromes whose connection with GERD is suspected. Extraesophageal syndromes with an established connection with GERD include reflux cough, reflux laryngitis, reflux asthma and reflux-induced destruction of tooth enamel, and syndromes with a presumptive connection with GERD include pharyngitis, sinusitis, pulmonary idiopathic fibrosis and recurrent otitis media [ 2, 3].
The word “reflux” itself literally means “reverse flow”. GERD is detected in many patients with chronic laryngitis. Otorhinolaryngologists often refer to this condition as laryngopharyngeal reflux (LPR), which represents the retrograde entry of stomach contents - acid and pepsin, as well as bile acids into the laryngopharynx [4, 5]. There are a number of synonyms for LPR, such as extraesophageal reflux, reflux laryngitis and laryngeal reflux. There is currently no gold standard for diagnosing LPR, and therefore data on its epidemiology are limited. In one study of 105 normal healthy volunteers, 86% had laryngopharyngeal reflux during laryngoscopy [6]. In a meta-analysis by AL Merati et al. analyzed data from pH probe readings in 264 patients with LPR; as a result, gastroesophageal reflux was detected in 10–60% of patients [7]. Studies such as these show that LPR is common in the general population, but needs to be diagnosed in some patients before adequate treatment can be given.
Normally, the upper esophageal sphincter and, to some extent, the larynx protect the lower respiratory tract from the entry of contents from the esophagus and stomach. The larynx is very well innervated and any esophageal reflux in a normal person will cause a protective cough. In patients with LPR, this “safety mechanism” may fail. For example, JE Aviv et al. The study showed that sensory deficits may play a role in the formation of LPR. The authors found a decrease in the laryngeal reflex in response to endoscopic air insufflation in patients with documented LPR [8]. Most researchers propose two main pathophysiological mechanisms for LPR, which directly or indirectly cause damage to the larynx by the contents of the esophagus and stomach. The direct mechanism is the result of the action of gastric contents (acid, pepsin and/or bile acids) acting directly on the mucous membrane of the hypopharynx. The indirect mechanism manifests itself as a result of the effect of reflux on the reflex structures of the larynx. This irritation is thought to cause bronchospasm, which in turn stimulates the vagal response, usually resulting in a nonproductive cough. The delicate ciliated epithelium of the posterior wall of the larynx, which normally evacuates mucus from the trachea, is significantly damaged by contact with gastroduodenal chemical agents, which can lead to mucous stasis in the larynx and discomfort [9]. Recently, it has been suggested that the enzyme carbonic anhydrase, which stimulates bicarbonate secretion, protects laryngeal tissues from reflux and that this protective mechanism may be impaired in the larynx of patients with LPR [10].
Most patients diagnosed with LPR may not have the classic symptoms of GERD. The main symptoms of LPR are respiratory complaints such as pain or burning in the throat, chronic cough (51%), excessive expectoration of mucus (42%), dysphonia (71%), dysphagia (35%), lump in the throat (47%), vertical (daytime) reflux, laryngospasm [11]. Researchers estimate that up to 50% of patients with laryngeal and voice disorders have reflux [12]. Based on laryngoscopy data, a special scale of “reflux signs” (SRS) was developed in 2001, which included 8 characteristic laryngoscopic symptoms with a general assessment of their severity from 0 to 26 points, which are presented in table. 1 [13]. Conducted by MF Vaezi et al. studies have shown that the presence of more than 7 points on the SRS correlated by 95% with positive data from 24-hour esophageal pH monitoring and suggested the presence of LPR [14]. Many patients with LPR often turn to a phoniatrist because they do not have pathognomonic complaints. If a patient’s dysphonia continues for more than three months, he or she should be screened to detect LPR [15].
Unfortunately, the specificity of laryngoscopic findings and their assessment using the presented SRS is not very high [6]. In 2002, the authors who developed the SRS also proposed the “Reflux Symptoms Index” (RSI) questionnaire, recommended for assessing the effectiveness of LPR treatment with proton pump inhibitors (PPIs), which consists of 9 questions and includes a dynamic assessment of a number of indicators (Table 2). Each IRS symptom is rated over the past month on a scale from 0 (no problems) to 5 (severe problems). A score of more than 13 correlates with a positive result of pH monitoring [13]. It is a self-administered tool that helps clinicians assess the clinical severity of LPR symptoms at diagnosis and then over time after treatment. The IRS is significantly higher in patients with LPR than in healthy controls (21.2 vs. 11.6, p < 0.001). However, this indicator is rarely used by general practitioners and otolaryngologists [16]. In 2004, R. Williams et al. proposed a scale for assessing the severity of chronic laryngitis in otorhinolaryngological manifestations of the extraesophageal form of GERD: degree 0 - no signs of inflammation, degree I (mild) hyperemia and/or swelling in the area of the arytenoid cartilages and interarytenoid space, degree II (moderate) - distribution of hyperemia and/ or edema beyond the area of the arytenoid cartilages and the interarytenoid space to the vocal folds, degree III (severe) - the presence of ulcerations in the area of the arytenoid cartilages and the interarytenoid space or the spread of the inflammatory process to the subvocal part of the larynx [17].
As is known, the most sensitive test for practical diagnosis of pathological acid gastroesophageal reflux is daily intraesophageal pH monitoring, when intraesophageal pH is continuously recorded at a distance of 5 cm above the lower esophageal sphincter. As a standard test for diagnosing LPR, ambulatory 24-hour intraesophageal hypopharyngeal pH monitoring using two pH sensors is proposed, with the second (proximal) pH sensor for fixing supraesophageal reflux as a cause of ENT disorders installed 5 cm above the upper alimentary sphincter (VPS) [18]. Unfortunately, although hypopharyngeal pH monitoring is a more sensitive test for identifying patients with GERD-induced ENT disorders, negative results cannot exclude LPR due to the intermittent nature of the disease and variability. Currently, a more accurate and patient-friendly method for diagnosing LPR has been developed by measuring naso- and oropharyngeal pH using a special Restech's Dx-pH measurement system, which allows recording pH fluctuations in the oral cavity and nasopharynx every 1/2 s for 48 hours [14 , 19].
Treatment of patients with LPR should include diet, lifestyle modifications, physical therapies, and pharmacotherapy. Modification of diet and lifestyle involves the patient following the following recommendations:
- after eating, you should avoid bending forward, you should go to bed with your head elevated;
- do not wear tight clothes and tight belts;
- avoid large meals;
- do not eat at night;
- limit the consumption of foods that cause a decrease in the pressure of the lower alimentary sphincter (LES) and have an irritating effect (fats, alcohol, coffee, chocolate, citrus fruits);
- stop smoking;
- normalize body weight.
Foods and drinks containing caffeine, alcohol, chocolate and mint relax the lower esophageal sphincter and increase stomach acid production, while carbonated drinks with/or without caffeine increase reflux and belching. In addition, the intake of acidic foods (with a pH below 4.6), such as citrus fruits and other sour fruits, tomatoes, dry wines and some others, should be limited. Lifestyle modifications that can reduce symptoms of LPR, as well as other manifestations of extraesophageal reflux, include smoking cessation and weight loss. A study by DL Steward et al. [20] showed that lifestyle changes for 2 months or more, with or without PPI therapy, significantly reduced the symptoms of chronic laryngitis.
Drug therapy usually includes PPIs, H2 receptor agonists, prokinetics, and cryoprotectants for the laryngeal mucosa. Empirical therapy with PPIs is justified because it can help in the diagnosis ex juvantibus (from the Latin ex - based on, juvanus - helping), i.e. treatment carried out in order to clarify the diagnosis. To date, studies of the effectiveness of PPIs in the treatment of LPR patients have produced a wide range of responses [21].
Studies evaluating the effectiveness of PPIs in LPR show results ranging from very good, with response rates reaching 70%, to no difference with placebo [22]. A controlled trial using lansoprazole 30 mg twice daily for three months in 22 patients with idiopathic chronic laryngitis found that 50% of patients in the treatment group had a complete response compared with 10% in the control group [23]. However, another study using lansoprazole at a similar dosage and regimen found no difference in response rates in patients with laryngopharyngitis [24]. A large multicenter study involving 145 patients with suspected LPR showed no benefit of esomeprazole 40 mg twice daily for four months compared with placebo [25]. One recent study of 85 patients with LPR found that PPI twice daily was more effective than once daily and that extending the course of treatment from two to four months resulted in more positive responses [26]. In general, for LPR, the use of a standard dose of PPI twice daily for two to three months is justified. Current recommendations do not suggest the use of H2-blockers in combination with PPIs in patients with suspected LPR [27, 28]. To achieve the best results, PPIs should be taken on an empty stomach 30 minutes before meals, with a course of treatment of 2–6 months until complete histological remission of laryngitis is achieved [29]. Patients whose quality of life and symptoms do not improve after two to three months of therapy most likely do not have GERD as a cause of LPR, but they should be evaluated for the presence of mixed reflux using manometry and pH monitoring [30]. If there is no effect from taking a PPI, a reassessment of symptoms with the participation of specialists from a pulmonologist and an allergist is necessary [31, 32].
The necessary comprehensive diagnosis and treatment of LPR was demonstrated by E. F. Kokorina, who assessed, in addition to endoscopic signs of esophagitis, the severity of chronic laryngitis in otorhinolaryngological manifestations of the extraesophageal form of GERD using the Williams scale, the level of dysphonia was assessed using the Consensus Auditory-Perceptual Evaluation of Voice (CAPE) scoring scale. V), proposed by the American Speech-Language Hearing Association, 2003. All patients underwent correction of GERD using PPI drugs; for the treatment of LPR in the main group of patients, the drug Erespal was added according to the standard regimen for 3 weeks. The duration of standard antireflux therapy was 3 months. Dynamic assessment of LPR was carried out several times up to 6 months after treatment; a statistically significant acceleration in the regression of reflux-induced changes in the larynx in patients of the main group was revealed [33]. I. L. Klyaritskaya, A. P. Balabantseva in their study showed that the use of double doses of PPI (pantoprazole) for 12 weeks leads to a significant reduction in symptoms of LPR compared to the control group. The optimal duration of treatment is 6–12 months, and after stopping the medication after 6 weeks it leads to an increase in scores on the Reflux Symptom Index questionnaire [34].
It is necessary to consider the use of prokinetics in the complex treatment of both GERD and LPR, which is a manifestation of GERD. Drugs such as metoclopramide, domperidone, cisapride and tegaserod have been used in patients with GERD in the past, but regular use of these drugs is not recommended by current standards due to limited indications and a high side effect profile [35]. In the treatment of GERD today, according to indications, the prokinetic agents itopride and mosapride are used; unfortunately, the latter is not registered in Russia. Itopride, registered in Russia since 2007, is used in patients with LPR as an adjuvant together with PPIs, as well as for other extraesophageal syndromes, accelerating the rate of reduction of symptoms [36, 37]. E. P. Oleinik et al. recommend the use of itopride, based on their own experience of using it in almost 1000 patients, in the complex treatment of all types of voice disorders due to GERD and LPR [38]. F.V. Semenov et al. A study involving 200 patients with LPR assessed the effectiveness of a two-week course of itopride in the treatment of otolaryngological manifestations of LPR. Its use led to a decrease in subjective complaints of patients and a weakening of the severity of laryngoscopic signs such as hyperemia and swelling of the mucous membrane of the arytenoid cartilages [39].
There are several scientific publications in the literature regarding rehabilitation speech therapy treatment of LPR with special voice exercises that strengthen the muscles of the larynx, and in some centers such therapy is carried out empirically without medical evidence-based support. A report on laryngeal rehabilitation in the treatment of chronic cough associated with GERD was recently published with significant improvement in symptoms [40].
The role of surgical fundoplication in patients refractory to even high (double) doses of PPI remains controversial. In a study by J. Swoger et al. evaluated symptoms in 10 PPI-resistant patients after fundoplication compared with 12 PPI-resistant patients who continued conservative treatment with double doses of PPI, showing that only 1 patient (10%) benefited from fundoplication, which was no different from the group comparison (7%) [41]. However, the role of surgery in PPI-resistant patients who have abnormal non-acid reflux remains important. They can be successfully treated with laparoscopic Nissen fundoplication [42]. Today, the Society of American Gastrointestinal and Endoscopic Surgeons clinical guidelines recommend antireflux surgery for patients who: have failed or are intolerant to medications; have significant extraesophageal manifestations such as aspiration, asthma, or cough; have ulcerative strictures as a complication of GERD [43].
Thus, there are no specific lesions of the larynx with laryngopharyngeal reflux, so the diagnosis of this pathology should be comprehensive and include both ENT and gastroenterological examination methods. Treatment of laryngopharyngeal reflux should also be comprehensive, from lifestyle modification and the use of local remedies to a long course of proton pump inhibitors and prokinetics in adequate dosage, and if they are ineffective, surgical treatment methods should be used.
Literature
- Vakil, N. van Zanden S.V., Kahrilas P. et al. The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensus // Am. J. Gastroenterol. 2006. Vol. 101. P. 1900–1920.
- Katz PO, Gerson LB, Vela MF Diagnosis and Management of Gastroesophageal Reflux Disease // Am J Gastroenterol. 2013. Vol. 108. R. 308–328.
- Lazebnik L. B., Bordin D. S., Masharova A. A. Modern understanding of gastroesophageal reflux disease: from Genval to Montreal // Experimental and clinical gastroenterology. 2007. No. 5. P. 4–10.
- Koufman JA, Aviv JE, Casiano RR, Shaw GY Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of OtolaryngologyHead and Neck Surgery // Otolaryngol Head Neck Surg. 2002. Vol. 127. R. 32–35.
- Ford CN Evaluation and management of laryngopharyngeal reflux // JAMA. 2005. Vol. 294. R. 1534–1540.
- Hicks DM, Ours TM, Abelson TI et al. The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers // J Voice. 2002. Vol. 16. R. 564–579.
- Merati AL, Lim HJ, Ulualp SO, Toohill RJ Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux // Ann Otol Rhinol Laryngol. 2005. Vol. 114. R. 177–182.
- Aviv JE, Liu H, Parides M et al. Laryngopharyngeal sensory deficits in patients with laryngopharyngeal reflux and dysphagia // Ann Otol Rhinol Laryngol. 2000. Vol. 109. R. 1000–1006.
- Hanson DG, Jiang JJ Diagnosis and management of chronic laryngitis associated with reflux // Am J Med. 2000. Vol. 108. R. 112S–119S.
- Johnston N., Bulmer D., Gill GA et al. Cell biology of laryngeal epithelial defenses in health and disease: further studies // Ann Otol Rhinol Laryngol. 2003. Vol. 112. R. 481–491.
- Koufman JA The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury // Laryngoscope. 1991. Vol. 101. R. 1–78.
- Koufman JA, Amin MR, Panetti M. Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders // Otolaryngol Head Neck Surg. 2000. Vol. 123. R. 385–388.
- Belafsky PC, Postma GN, Koufman JA The validity and reliability of the reflux finding score (RFS) // Laryngoscope. 2001. Vol. 111. P. 1313–1317.
- Vaezi MF Sensitivity and specificity of reflux-attributed laryngeal lesions: experimental and clinical evidence // Am. J. Med. 2003. Vol. 115, (Suppl. 3 A). P. 97 S-104.
- Karkos PD, Yates PD, Carding PN, Wilson JA Is laryngopharyngeal reflux related to functional dysphonia? // Ann Otol Rhinol Laryngol. 2007. Vol. 116, No. 1. P. 24–29.
- Ahmed TF, Khandwala F, Abelson TI et al. Chronic laryngitis associated with gastroesophageal reflux: prospective assessment of differences in practice patterns between gastroenterologists and ENT physicians // Am J Gastroenterol. 2006. Vol. 101. R. 470–478.
- Williams RB, Szczesniak MM, Maklean HM et al. Predictors of Outcome in an Open Label, Therapeutic Trial of High-Dose Omeprazol in Laryngitis // Am J Gastroenterol. 2004. Vol. 42. R. 776–785.
- Vincent DA Jr., Garrett JD, Radionoff SL et al. The proximal probe in oesophageal pH monitoring: development of a normative database // J. Voice. 2000. Vol. 14. P. 247–254.
- Ayazi S., Lipham J., Hagen G. et al. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold // J. Gastroenterol. Surg. 2009. Vol. 13 (8). P. 1422–1429.
- Steward DL, Wilson KM, Kelly DH et al. Proton pump inhibitor therapy for chronic laryngopharyngitis: a randomized placebo-control trial // Otolaryngol Head Neck Surg. 2004. Vol. 131. R. 342–350.
- Martinucci I., de Bortoli N., Savarino E. et al. Optimal treatment of laryngopharyngeal reflux disease // Ther Adv Chronic Dis. 2013. Nov. Vol. 4 (6). R. 287–301.
- Vaezi MF Extraesophageal manifestations of gastroesophageal reflux disease // Clin Cornerstone. 2003. Vol. 5. R. 32–38.
- El-Serag HB, Lee P, Buchner A et al. Lansoprazole treatment of patients with chronic idiopathic laryngitis: a placebo-controlled trial // Am J Gastroenterol. 2006. Vol. 96. R. 979–983.
- Havas T. et al. Posterior pharyngolaryngitis: double blind randomized placebo controlled trial of proton pump inhibitor therapy // Aust J Otolaryngol. 1999. Vol. 3. R. 243–246.
- Vaezi MF, Richter JE, Stasney CR et al. Treatment of chronic posterior laryngitis with esomeprazole // Laryngoscope. 2006. Vol. 116. R. 254–260.
- Park W., Hicks DM, Khandwala F. et al. Laryngopharyngeal reflux: prospective cohort study evaluating optimal dose of proton-pump inhibitor therapy and pretherapy predictors of response // Laryngoscope. 2005. Vol. 115. R. 1230–1238.
- Peghini PL, Katz PO, Castell DO Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects // Gastroenterology. 1998. Vol. 115. R. 1335–1339.
- Fackler WK, Ours TM, Vaezi MF, Richter JE Long-term effect of H2 RA therapy on nocturnal gastric acid breakthrough // Gastroenterology. 2002. Vol. 122. R. 625–632.
- Belafsky PC, Postma GN, Koufman JA Validity and reliability of the reflux symptom index (RSI) // J Voice. 2002. Vol. 16. R. 274–277.
- Yuksel ES, Vaezi MF Extraesophageal manifestations of gastroesophageal reflux disease: cough, asthma, laryngitis, chest pain // Swiss Med Wkly. 2012. Vol. 142. R. l35–44.
- Kahrilas P., Shaheen N., Vaezi M. et al. American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease // Gastroenterology. 2008. Vol. 135(4). R. 1383–1391, e1381–e1385.
- Zerbib F., Stoll D. Management of laryngopharyngeal reflux: an unmet medical need // Neurogastroenterol Moti. 2010. Vol. l22. R. 109–112.
- Kokorina V. E. Use of the drug erespal in schemes for the correction of reflux-induced laryngitis // Bulletin of Otorhinolaryngology. 2010. No. 6. pp. 61–63.
- Klyaritskaya I. L., Balabantseva A. P. Comparative effectiveness of high daily doses of proton pump inhibitors for laryngopharyngeal reflux // Ukrainian Therapeutic Journal. 2012. No. 1. pp. 21–27.
- Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease // American Journal of Gastroenterology. 2005. Vol. 100 (1). R. 190–200.
- Ezzat WF, Fawaz SA, Fathey H., El Demerdash A. Virtue of adding prokinetics to proton pump inhibitors in the treatment of laryngopharyngeal reflux disease: prospective study // Journal of Otolaryngology. 2011. Vol. 40 (4). 350–356.
- Chun BJ, Lee DS The effect of itopride combined with lansoprazole in patients with laryngopharyngeal reflux disease // European Archives of Oto-Rhino-Laryngology. 2013. Vol. 270(4). 1385–1390.
- Oleynik E. P., Kochesokova E. A., Ivanchenko G. F., Demchenko E. V. Treatment of patients with dysphonia with gastroesophageal reflux disease // Treating Physician. 2010. No. 9. pp. 7–10.
- Semenov F.V., Gorbonosov I.V., Vartanyan M.S. Experience with the use of itopride for the treatment of otorhinolaryngological manifestations of laryngopharyngeal reflux // Farmateka. 2011. No. 2. pp. 91–95.
- Pacheco A., Cobeta I., Wagner C. Refractory chronic cough: new perspectives in diagnosis and treatment // Arch Bronconeumo. 2013. Vol. l49. R. 151–157.
- Swoger J., Ponsky J., Hicks DM et al. Surgical fundoplication in laryngopharyngeal reflux unresponsive to aggressive acid suppression: a controlled study // Clin Gastroenterol Hepatol. 2006. Vol. 4. R. 433–441.
- Mainie I., Tutuian R., Agrawal A. et al. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication // Br J Surg. 2006. Vol. 93. R. 1483–1487.
- Zerbib F., Sifrim D., Tutuian R. et al. Modern medical and surgical management of difficult-to-treat GORD // United Eur Gastroenterol J. 2013. Vol. 1. R. 21–31.
E. Yu. Plotnikova*, 1, Doctor of Medical Sciences, Professor M. V. Krasnova**, Candidate of Medical Sciences K. A. Krasnov**, Candidate of Medical Sciences E. N. Baranova*
* State Budgetary Educational Institution of Higher Professional Education Kemerovo State Medical Academy of the Ministry of Health of the Russian Federation, Kemerovo ** Municipal Budgetary Healthcare Institution City Clinical Hospital No. 3 named after. M. A. Podgorbunsky, Kemerovo
1 Contact information
Abstract. Ethiopathogenetic mechanisms, clinical indicators and diagnostic methods of laryngopharyngital reflux. Modern treatment methods are described that presumably diet, changing of the mode of life, physical treatment methods and drug therapy as well as indications for surgery.