More than 90% of people living with HIV suffer from skin rashes. An HIV rash takes the form of any skin disease and causes symptoms unusual for skin diseases. Skin irritation is the first sign of infection and appears in the first month after infection. Therapy for rashes is aimed at reducing the intensity and suppressing unpleasant sensations.
What does a rash look like in people with HIV?
The characteristics of the rash depend on the skin disease that caused it. The only thing that all types of rashes with HIV infection have in common is more pronounced redness and itching, difficulty in treatment, and frequent relapses. In the photo below you can see in more detail the nature of the rashes in various diseases.
Skin diseases in HIV-infected people are more severe than in uninfected people, and are accompanied by fever, enlarged lymph nodes, intestinal upset, body and throat pain, and sweating.
Seborrheic dermatitis
It is expressed in the appearance of red plaques, which become crusty over time. Inflammations appear first on the face, then spread to the scalp, the inside of the knees and elbows.
Plaques characteristic of seborrheic dermatitis form at an early stage of the disease in half of those infected.
Stomatitis
Bubbles, white plaque and ulcers of various sizes, also covered with white plaque, appear on the oral mucosa.
Stomatitis in an HIV-infected person, which occurs against the background of allergies, is accompanied by fever and sore throat. Rashes in the mouth are one of the first external signs of HIV infection.
Allergy
In patients with immunodeficiency, allergic urticaria is noted, which is accompanied by the appearance of red spots and a rash similar to an insect bite.
Kaposi's sarcoma
Characterized by skin spots and lumps in the form of burgundy colored bumps. The rashes are localized on the face, mouth (tongue), genitals, from where they spread to the torso, arms and legs. A year after HIV infection, the disease enters the final stage, in which many malignant neoplasms appear on the patient’s skin and mucous membranes.
Kaposi's sarcoma is more common in HIV-infected men.
Fungus
In case of fungal diseases, such as candidiasis, lichen, rubrophytia, foci of inflammation with pronounced peeling, redness, severe itching, and a white coating appear on the patient’s skin.
Irritation is first localized on the hands, feet and groin area, then quickly spreads throughout the body.
Exanthema
Rashes occur when the body becomes infected with an infection. Exanthema appears as a colorless or bright red papular rash. The location of the rash depends on the pathogen, but most often appears in the torso and groin area.
In HIV-infected people, exanthema is caused by herpes virus, cytomegalovirus, Coxsackie virus, enteroviruses, hepatitis C virus, molluscum contagiosum, and human papillomavirus.
Psoriasis
It appears as red plaques with clear boundaries, covered with gray scales.
The severity of skin lesions depends on the degree of impairment of the immune system.
Scabies
Scabies affects up to 30% of HIV-infected people. The disease is characterized by intense itching, worsening at night.
White or red S-shaped itch burrows appear on the hands, between the fingers, on the mammary glands, under the armpits, and in the groin.
Pyodermatitis
The rash occurs against the background of inflammation of the hair follicles and takes the form of burgundy pimples and pustules, reminiscent of a teenage rash.
Syphilis
With secondary syphilis, a pink or red maculopapular rash appears on the patient’s body, which spreads throughout the body.
Secondary syphilis occurs 3-4 months after infection with Treponema pallidum.
What is HIV? What is HIV infection
The human immunodeficiency virus, or HIV, was identified and described relatively recently. Invading the human body, it primarily affects macrophage cells and T-lymphocytes, which are responsible for recognizing and destroying hostile bacteria. Thus, the body's immune barrier loses its ability to resist both external bacterial attacks and internal opportunistic flora.
The immunodeficiency virus is transmitted exclusively through sexual contact or through direct contact of a healthy body with infected blood. Transmission of the virus through household or food contact is impossible.
HIV infection is a slow-onset disease caused by a virus and occurs against a background of suppressed immunity. It can take years from the introduction of the virus to the clinical manifestations of the disease. During this entire period, the virus does not manifest itself in any way, and its presence can only be diagnosed using a laboratory method.
Diagnosis of rashes on the body
With HIV and AIDS, it is difficult to visually determine the type of rash - the nature of skin inflammation in infected people is different.
To determine the type of rash and its cause, the following diagnostic measures are carried out:
- Clinical analysis of blood and urine.
- Blood test for sexually transmitted viruses.
- Skin scraping. The method is used to detect intradermal mites and fungi that cause skin diseases.
- Blood tests for antibodies to allergens and allergy skin tests.
- Hormonal studies.
- Biopsy of skin lesions. They detect the presence of cancer cells, which is important for diagnosing Kaposi's sarcoma.
Features of plaque in HIV
You should know! HIV infection is insidious - in many infected people the pathology is asymptomatic for many years, while the patient is a source of infection for all his partners.
The clinical picture is varied, but the constant accompanying signs are infectious diseases of an aggressive nature.
First of all, HIV affects the condition of the oral cavity . Typical manifestations are:
- A dense, thick yellowish coating on the tongue, palate and inner surface of the cheeks due to HIV infection.
- Various painful inflammations - ulcers, blisters, erosions.
- Poor condition of the teeth - darkening of the enamel, plaque, instability, formation of tartar.
- Deterioration of the gums – redness, bleeding, suppuration.
Note! As the disease progresses, the clinical picture worsens and periods of remission become shorter and shorter each time.
Diagnosis, examination and differential diagnosis
The only reliable way to diagnose HIV is a blood test. The most widely used method is enzyme-linked immunosorbent assay (ELISA), which shows the presence of HIV antibodies in the blood. If less than 6 months have passed since infection, antibodies to the virus will not have time to develop, and the analysis will show an erroneous negative result.
If a positive result is obtained after ELISA, the second stage of the examination is prescribed - immunoblotting. The principle of its operation is the presence of an electric field, which detects antibody molecules with a guarantee of an accurate result.
Manifestations of HIV in the oral cavity must be differentiated from other bacterial and viral diseases (herpes, tuberculosis, syphilis), from some autoimmune diseases (lichen planus). Laboratory tests are crucial for the final diagnosis.
Provoking factors - why infection occurs
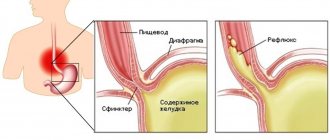
The immunodeficiency virus enters the body through microtrauma to the mucous membrane during unprotected sexual intercourse, or into the bloodstream when the integrity of the skin is violated with a non-sterile syringe. Virions are delivered through the bloodstream to the lymph nodes, where they are integrated into the RNA of immune cells - lymphocytes. Reproduction of the virus inside the cell blocks its ability to protect the body from foreign agents, which leads to multiple diseases of the organs and systems of the infected person.
The virus gradually reduces the ability of the mucous membrane in the mouth to resist fungi and bacteria. The possibility of destruction of atypical malignant cells by lymphocytes of the dentofacial area is also blocked. HIV-associated lesions in the mouth arise as a result of failure of the general immune system.
Treatment methods
Therapy for HIV infection and its manifestations in the oral cavity should be comprehensive and carried out with the participation of an infectious disease specialist, dentist, and otolaryngologist. If necessary, doctors of other specialties (surgeons, oncologists) should be involved in treatment. It is mandatory to monitor the patient once every 4 months for timely detection of possible complications.
General
Antiviral therapy is prescribed for treatment. Drugs and dosage are selected individually for each patient by the attending infectious disease specialist.
Modern therapy allows a person to live to a ripe old age, provided that they take prescribed medications and undergo periodic blood tests to determine the effectiveness of treatment and viral concentration in the body.
Maintaining a healthy lifestyle is important - quitting smoking, alcohol, drugs, maintaining a daily routine, balancing nutrition, dealing with stress, moderate physical activity, and physical exercise.
Dental care
Dental care for HIV-infected people is provided on an equal basis with other patients in all dental institutions of the Russian Federation. Treatment is divided into 3 groups:
- Etiological – carried out for bacterial and viral infections. Antibiotics and antiviral drugs are selected and prescribed based on the sensitivity of the pathogen to them.
- Preventive – preventing relapse of the disease. Includes filling of carious teeth, removal of dental plaque, and general sanitation.
- Symptomatic – treatment of ulcers and erosions with anesthetics (Lidocaine spray and gel), antiseptics (Chlorhexidine, Furacilin), prescription of healing drugs (Solcoseryl, sea buckthorn oil).
Useful video
From this video you will learn about tongue lesions due to HIV infection:
Unfortunately, today there are no specific means to get rid of HIV infection. However, everyone can do everything they can to reduce the likelihood of infection.
Carefully monitor your own health and try to listen to the signals that your body gives you.
Even such a typical and common ailment as a coating on the tongue can occur as a result of HIV infection.
How to get rid of plaque?
All dental ailments , including plaque on the tongue surface, caused by HIV infection, can be quite successfully eliminated with timely consultation with a specialist.
It is worth noting! The primary task in this case is to increase local immunity and help the microflora resist pathogens so that the disease does not progress.
Otherwise, therapy varies depending on each specific case, but most often it includes :
- Regular dental examination and timely elimination of signs of disease.
- Taking medications . These include various broad-spectrum antibiotics, antiviral and antifungal agents, etc.
The patient himself must select personal hygiene products with special care , regularly use dental floss, toothpaste and mouthwash with bactericidal properties .
To remove plaque from HIV infection, it is permissible to use a special brush or scraper to clean the surface of the tongue.
For your information! Oral care alone will not be enough - to avoid relapse, it is necessary to undergo maintenance therapy.
The surface of this sensory organ must be cleaned, moving from root to tip, using light “sweeping” movements to remove unwanted plaque. You can finish cleaning by rinsing.