What is glossitis?
What do we know about the tongue as an organ? We know that it is located in the mouth, which helps us articulate and pronounce words correctly, helps us mix food, feel all the diversity of existing tastes, that they can be shown indignation, and in some African countries, a demonstration of it can be used to declare war.
Such a significant number of different physiological and social functions may one day be compromised. And the name of this threat is glossitis.
Despite the absolutely clear location of this organ, there are big questions about which doctor deals with its problems: a dentist, gastroenterologist, maxillofacial surgeon or otolaryngologist. This is not an easy question, and sometimes you can endlessly go from one specialist to another. But let's finally understand this intriguing matter.
Why does the disease occur?
The culprits of inflammation on the mucous membrane of the tongue are pathogenic microorganisms (viruses, bacteria) that the local immune system cannot cope with. Most often, glossitis is caused by the herpes virus. It can remain in a latent (sleeping) state for many years after infection and not bother a person in any way. But when immunity decreases, it becomes more active and begins to multiply.
Other possible reasons:
- thermal or chemical burns;
- allergic reaction to toothpaste,
- drinking tongue-burning drinks;
- frequent mechanical injuries from the edges of decayed teeth or sharp edges of fillings, biting the tongue;
- abuse of spicy foods;
- excessive passion for mouth fresheners, rinses with aggressive composition.
People over 50 years of age, smokers, and lovers of caramel and lollipops are at risk. The oral cavity is an ideal place for the proliferation of pathogenic microorganisms, therefore, ignoring hygiene and chronic dental pathologies also cause inflammatory processes in the tongue area.
In most cases, glossitis acts as a symptom of disorders of the digestive system, dysbacteriosis and autoimmune diseases.
Forms and types of disease
Inflammation of our organ of taste occurs frequently and does not always manifest itself with symptoms, proceeding completely hidden from us.
There are several forms and types of the disease:
- According to the duration, the disease is divided into acute (develops quickly and lasts no more than a month) or chronic glossitis (lasts more than a month);
- According to the form of the lesion, the catarrhal form (proceeding with redness and swelling) and the desquamative form (proceeding with a change in appearance) are distinguished;
- purulent forms - phlegmon and abscess (a purulent focus in the thickness of the organ tissue itself);
- a separate group includes neurological diseases of the nerves innervating this organ.
Cellulitis and abscess occur acutely, they are associated with infection and require urgent surgical intervention. They manifest themselves as severe pain, chills and swelling of the lymph nodes of the neck - this form can be confused with acute inflammation of the salivary glands, so diagnosis using ultrasound and x-rays is needed. It is better not to delay these symptoms and seek medical help as an emergency.
The catarrhal form of glossitis manifests itself with a sharp blood supply - the tongue swells, becomes bright red - this can manifest itself, for example, with scarlet fever, or an allergic reaction, which, in addition to the organ of taste itself, spreads to the soft palate with the tongue. Treatment in this case is aimed at eliminating the allergic reaction and inflammation.
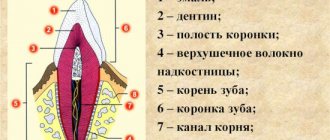
The largest and most heterogeneous group is desquamative glossitis. It is difficult to list the number of factors (external, internal) that can provoke this form of the disease. We will not make a mistake if we say that “the tongue is the mirror of the digestive tract.” Since it contains many nerve receptors and papillae of different shapes and purposes (filamentous, cone-shaped, mushroom-shaped, leaf-shaped, groove-shaped), a change in each link of its anatomy outwardly reveals a hidden disease. Let's take a little look at the most common diagnostic signs of these conditions.
Other symptoms and signs
Often desquamative glossitis of the tongue is accompanied by additional symptoms:
- a burning sensation, discomfort in the tongue area;
- tingling;
- irritation while eating;
- problems related to taste.
This disease can significantly reduce the quality of life because it constantly reminds itself, especially during meals.
You may also hear the name of the disease as “geographic tongue.” This is due to the fact that the appearance of the surface gives the impression that in front of you is a geographical map - such a bizarre pattern is made up of various uneven foci.
Changes in appearance depending on the disease
One of the common types is “geographical tongue,” in which its upper surface resembles a map with the borders of countries and continents. This is the most common form of glossitis, which does not manifest itself in any way and does not require medical intervention unless complications arise (numbness, burning). This form occurs in waves, provoked by rough or spicy food, and hormonal cyclic changes. But the loss of the pattern of the papillae may indicate the presence of hypo- or hyperacid gastritis (that is, with increased or decreased acidity of gastric secretions) - such symptoms are typical for patients with gastroesophageal reflux, when hydrochloric acid and bile are thrown from the stomach into the oral cavity.
"Geographical language"
The second most common type of glossitis is a folded tongue. This is an independent type of glossitis. In this case, the back of the tongue seems to be riddled with deep cracks and it feels like there are folds in it. This form of glossitis sometimes accompanies neurological diseases (for example, Melkerson-Rosenthal syndrome) and is present in people with acromegaly (hormone-active pituitary tumor).
"Folded tongue"
Also characteristic are manifestations of various anemias, which are reflected in the appearance of the organ: iron deficiency anemia can manifest itself as a burning sensation on the tip of the tongue, the appearance of cracks on it and an erased pattern of taste buds. Pernicious anemia (B12 deficiency), in which the tongue has a “varnished” appearance with a smooth, swollen surface, sometimes quite painful, with burning symptoms, is the main cause of Gunther-Miller glossitis.
"Lacquered Tongue"
A large group of pathological conditions of this organ are ENT-associated symptoms associated with chronic tonsillitis - here the symptoms are non-specific, ranging from a dirty coating on the tongue to manifestations of diphtheria with white masses that are difficult to remove.
They also distinguish the formation of ulcers on the tongue - aphthous glossitis, which, as a rule, has a viral cause and goes away on its own. This is a recurrent disease, with more frequent episodes it is necessary to exclude pathology of the immune system.
When visiting a doctor, you will often notice pronounced teeth marks on the side of the tongue - a sign of long-term swelling. This occurs in patients with enterocolitis, kidney disease and cardiovascular diseases. The reason for this condition is water retention in the body.
Imprints from teeth on the lateral surface of the tongue
In the presence of abundant white plaque, accompanied by pronounced redness of the oral mucosa, one should suspect a fungal infection, often of a candidal nature. In this case, HIV must be excluded. Also with HIV, “hairy leukoplakia” occurs, when the tongue appears to have white hairs on the side surface, similar to flames - this condition is specific to HIV.
"White Hairy Tongue"
It is worth noting the existence of a “black hairy tongue”, which is a symptom of gastrointestinal disorders, less commonly a fungus.
"Black Hairy Tongue"
As you can see, our organ of taste reflects deep processes in the body, and it is difficult to single out one specialist responsible for its treatment. It is worth involving doctors of different spectrum in therapy, conducting studies based on data from smears and blood tests. But what general recommendations can we, as doctors, give to patients?
Causes
One hundred percent causes of this disease have not been identified. And first you need to find out what type of disease we are talking about. If this is the primary type, then the factors are usually external. If secondary - internal, associated with pathologies and diseases of internal organs.
Given the diversity of situations, there are many potential causes of desquamative glossitis, for example:
- tongue injuries due to burns, dentures, teething, etc.;
- chronic diseases of the gastrointestinal tract, gall and liver;
- violation of vitamin and mineral metabolism. For example, when the body lacks vitamins B3, B6 or B1, folic acid, iron, etc.;
- diseases of the hematopoietic system;
- endocrine changes, including during pregnancy;
- autoimmune diseases: rheumatism, lupus, systemic scleroderma;
- chronic dermatoses - the same as psoriasis;
- acute infections: from influenza to typhoid fever;
- helminthic infestations;
- drug intoxication. It can occur due to improper or uncontrolled use of antibiotics and other medications;
- heredity.
It is obvious that with such a variety of causes of desquamative glossitis, effective treatment begins with a thorough diagnosis. First, the doctor needs to rule out a huge number of diseases - and only after that it will become clear how to act.
Care instructions
- Hygiene. We brush our teeth, but forget about our tongue. Thanks to advertising in the media, people are more likely to buy toothbrushes with a special brush for cleaning the tongue - and this is important. After all, bacteria live in the gap between the taste buds and food particles remain that must be removed from there.
- Caring for your oral health. Do not forget about the cleanliness of the palatine tonsils and the presence of reflux of gastric contents into the oral cavity.
- And the most important thing is to monitor your general health, undergo a timely examination by a doctor to identify the cause of inflammation - primarily to the dentist, but if you even consult a therapist or an infectious disease specialist, or an ENT doctor - you will not be mistaken, since there are almost no diseases, which would not affect such an important organ one way or another.
Treatment
Depending on the causes and situation, treatment of desquamative glossitis may involve a combination of different methods:
- the use of local preparations (rinses) to relieve itching and discomfort;
- elimination of underlying diseases that affect the appearance of such a symptom;
- a gentle diet that does not irritate the tongue while eating;
- use of anti-inflammatory, vitamin-mineral, antihistamines, sedatives and other drugs - as prescribed by a doctor;
- novocaine blockades if the pain is severe and complicates the patient’s life;
- physiotherapy: ultraphonophoresis, ultrasound therapy, etc.
During the treatment process, it is important not to miss the underlying disease, which affects the appearance of signs of desquamative glossitis (if any). Otherwise, the patient will return to unwanted symptoms again and again until the main disease is discovered.
Hairy black tongue (villous glossitis)
This form of glossitis is characterized by the growth and keratinization of filiform papillae (they become hair-like). The mechanism of development of this disease is not fully understood. According to one version, the development of villous glossitis is facilitated by the influence of local irritating factors, as well as candidiasis that develops while taking antibiotics.
Treatment of this form of glossitis includes mechanical (tweezers) removal of filiform papillae and subsequent treatment of the surface of the tongue with a solution of copper sulfate. For candidiasis, antifungal agents are prescribed.
Main manifestations of pathology
Symptoms vary. The severity and nature of the disease depends on the form of glossitis and the cause of its occurrence. Characteristic manifestations:
- discomfort or pain when talking or eating;
- change in tongue color - from pale pink to brown;
- swelling, changes in the size and shape of the organ;
- ulcerative lesions, sometimes with purulent contents;
- bleeding wounds;
- the appearance of plaque;
- smoothing of the taste buds, causing the surface of the tongue to become smooth.
An increase in temperature does not always occur. At the initial stage, a person feels only pathological changes on the surface of the tongue; changes in general well-being occur only as a result of the development of intoxication.
In a complicated course, without the necessary treatment, the pathology manifests itself:
- increased salivation;
- bad breath, even with good oral hygiene;
- difficulty swallowing;
- speech disorders due to swelling and deformation of the tongue;
- change in taste or its complete absence;
- burning.
With the villous form, there is no unpleasant painful sensation. But the main symptom is the formation of the so-called “hairy tongue”. Dark, dense growths of a dark color, similar to villi, appear on the surface of the organ. An accurate diagnosis can only be made by a doctor after examination and examination.