20.01.2017
Upper micrognathia or underdevelopment of the upper jaw is a rather rare type of deformation of the upper jaw, which can be caused by both endo and exogenous factors. Differential diagnosis of this pathology can be carried out in comparison with the false form, the cause of which is excessive development of the lower jaw.
Visually, underdevelopment of the upper jaw has the appearance of a mesial bite. Externally, true micrognathia is manifested by a sharp forward expression of the nose and retraction of the upper lip, and the expression of the nasolabial furrows. At the same time, functional malocclusion is expressed in difficulties in biting off food due to the lack of antagonists. Speech is often impaired. Diagnosis is carried out using tomography of the maxillofacial area.
Anomalies of dental development
The most common anomalies in the structure of hard tissues are systemic or local hypoplasia of permanent or temporary teeth. Systemic hypoplasia looks like a white or yellow spot with a smooth surface. It is impossible to determine it using x-rays. Pits or grooves appear in the image as areas of clearing.
Local hypoplasia develops most often due to injury to the follicle or against the background of chronic inflammation of the periodontium of a milk tooth - in a permanent tooth. Enamel hyperplasia is rare and appears on an x-ray as a more intense, dense shadow.
Prognathia: causes of occurrence
Distal bite, as this defect is also called, is most often congenital, hereditary in nature - the risk of developing such an anomaly is higher in people whose parents or grandparents also suffered from bite problems. But there are several other reasons why a child develops prognathia:
- pathologies of intrauterine development of the fetus;
- pathologies of postnatal development;
- improper nasal breathing in childhood;
- incorrect method of artificial feeding, when the baby makes almost no effort to suck milk from the nipple - the lack of load on the masticatory muscles leads to disruption of the development of the bite;
- too early loss of baby teeth, especially canines;
- a complication after rickets - a disease of infants and young children, which leads to impaired bone formation and insufficient mineralization due to vitamin D deficiency.
Anomalies in the number of teeth
The number of teeth may decrease due to the absence or death of rudiments, or increase. Primary adentia occurs mainly in the permanent dentition. With complete teeth, all teeth are missing; with partial teeth, the upper lateral incisors and lower second molars are missing. This happens with ectodermal dysplasia.
Supernumerary teeth are characterized by an irregularly shaped crown. They erupt for a long time and remain in the jaw. An x-ray - panoramic study - allows you to determine this or that anomaly.
Sometimes a tooth is missing from a row due to retention - retention of the tooth in the jaw bone. It is provoked by its incorrect initial position, lack of space or narrowing of the dentition. X-ray examination allows you to determine the position of the impacted tooth and its relationship with the surrounding anatomical formations. For this purpose, special techniques are used - tomography, oblique projections, etc.
What is microgenia (micrognathia) of the lower jaw
Microgenia of the lower jaw is nothing more than a small underdeveloped chin. A defect in appearance caused by a lack of bone in the chin area.
A young girl contacted Platiennetal with complaints about a small chin and asymmetry of the chin area.
A chin augmentation was performed using a Porex implant, Bisha's fat bags in the cheek area were partially removed. It was possible to visually narrow and “stretch” the oval of the face, making it harmonious.
Performed by: plastic surgeon Andrey Iskornev
Photo from the patient’s personal archive. Surgeon: Iskornev A.A.
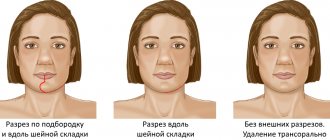
Performed: upper blepharoplasty, ️installation of a chin implant, medial and lateral platysmaplasty with neck lift through an incision in the earlobe. Performed by a surgeon - Maxim Vasiliev .
A small or sloping chin spoils any face. And if a small chin in men can still be hidden under a thick beard (for those who find the strength to wear this “decoration”, which makes the owner look ten years older), then a small chin in women cannot be disguised.
Looking at a human face, we often see only the whole and do not notice the details.
A short chin in itself is not noticeable and is not perceived as a flaw. But with its size it violates the proportions. From the side, a fuzzy oval of the face, early wrinkles, folds on the neck and a premature double chin are visible. And only a specialist - a maxillofacial surgeon or an orthodontist - will understand that the reason is the insufficient size of the chin.
Anomalies of jaw development
These abnormalities may be congenital or occur after illness, injury, endocrine disorders, or radiation therapy.
- Congenital clefts
of the hard palate and alveolar process are recognized in clinical practice and are often caused by genetic causes. The pathology is often accompanied by dental anomalies, delayed development of permanent dentition, and deformation of the nasal cavity. - Cranioclavical dysostosis
is a congenital systemic disease, which is characterized by changes in the dental system. Due to anatomical pathologies, the upper jaw remains underdeveloped, and the hard palate is shortened; permanent teeth erupt by the age of 20-30, and many of them are impacted, supernumerary and dystopic. - Craniostenosis, or craniofacial dysostosis
, is premature synostosis of the sutures in the bones and base of the skull, when the skull is stretched vertically, intracranial pressure changes, and other pathological processes develop. - Maxillofacial dysostosis
- on X-ray images it is indicated by underdevelopment of both jaws, the zygomatic arch and bone, deformation of the orbits, as well as malocclusion and abnormal development of molars.
There are anomalies of the dental system caused by endocrine disorders. For example, in the category of children with incorrect functioning of the thyroid gland, delayed teething is diagnosed, multiple caries often develops, and underdevelopment of the jaws is also observed.
If there is a history of deficits in the functioning of the anterior lobe of the pituitary gland, the roots of baby teeth may not be resolved, but remain for life, interfering with the eruption of permanent ones. In turn, with hyperfunction of the pituitary gland, the roots grow too quickly, the time for eruption is reduced, and hypercementosis develops at the tips of the roots. Children with Down syndrome begin to erupt primary teeth at 4-5 years of age, but they often do not fall out until 14-15 years of age.
Underdevelopment of the upper jaw - a clinical case
A patient with skeletal asymmetry due to underdevelopment of the upper jaw came to us for further planning of orthognathic double-jaw surgery.
Rice. 1. Photo of the patient. Skeletal asymmetry. Underdevelopment of the upper jaw.
Rice. 2. Intraoral photograph of underdevelopment of the upper jaw.
Cone beam computed tomography (CBCT) was performed with further planning for orthognathic bimaxillary surgery.
Fig.3. Planning for orthognathic double-jaw surgery.
Orthodontist consultation
At the consultation, orthodontist M.P. Sleptsova conducted an examination and made a preliminary diagnosis, telling the parents how to correct a child’s malocclusion, approximately how long it would take for treatment and the approximate cost. Based on the results of the examination, we can say for sure that there will not be enough space for the eruption of permanent teeth and the teeth may begin to grow crooked. The fact is that permanent teeth are larger in size than baby teeth, and there is clearly not enough space in the jaw.
It is possible to say more precisely how much it will cost to correct a child’s bite after an orthodontic diagnosis, which includes taking impressions and calculating the impressions, performing a tele-roentgenogram of the head in frontal and lateral projection, as well as a panoramic image of the teeth and calculating x-ray images, consultation with an ENT specialist, speech therapist and osteopath. Diagnostics is needed to make an accurate diagnosis and develop the correct treatment tactics.
Photos of teeth before treatment:
Panoramic photo of teeth before treatment:
Diagnostics showed that there is a narrowing and shortening of the upper dentition, biretrusion (the upper front teeth are located behind the lower ones and should overlap them), displacement of the lateral teeth to the center, tortoanomaly (teeth rotated around their axis), hypertrophy of the tonsils, adenoids, infantile swallowing, mouth breathing.
Commentary by the chief physician of Dial-Dent S.V. Tsukora: “The causes of malocclusion in children may be improper swallowing, incorrect position of the tongue, the presence of a bad habit of constantly sucking a finger, pen, toy, etc., mouth breathing due to a constantly stuffy nose or due to habit, lack of solids in the diet food. The sooner parents show their child to an orthodontist, the easier it is to stop developing problems and prevent serious malocclusion. We have all the necessary specialists in our clinic - orthodontists, pediatric dentists, ENT specialists, speech therapists, osteopaths, so we can help in the most difficult cases, and the treatment result will be stable, since in addition to simply straightening teeth, we work with the cause of malocclusion.”
Development of tactics for correcting a child’s bite
Since the child is at an age when baby teeth are actively falling out and permanent teeth are erupting in their place (changeable bite), it is necessary first of all to create a place for the normal eruption of permanent teeth. Based on the current situation, it is necessary to increase the size of the upper jaw. Then you need to move the displaced teeth into place, allow all permanent teeth to erupt and align their position if necessary.
Commentary by speech therapist, myofunctional therapist T.B. Zukor: “When carrying out orthodontic treatment, it is not enough to just correct the position of the teeth; it is necessary to eliminate the cause of the malocclusion. In this case, mouth breathing was observed, as there were ENT problems. I, as a myofunctional therapist, can retrain a child from habitual mouth breathing to nose breathing, but only on condition that the nose is breathing! That is, the participation of an ENT specialist is required, who, for his part, will eliminate the existing problems. The stability of the result of bite correction directly depends on eliminating the causes of the disorder! If you don’t normalize breathing through your nose and restore the correct balance of the muscles of the tongue, cheeks and lips, you will have to wear retainers for a very long time, and maybe for life, since the teeth will constantly strive to get back into position incorrectly.”
Treatment plan:
Stage 1 - Expansion of the upper jaw.
A McNamara appliance will be used to expand the upper jaw. This is a fixed orthodontic plate appliance with a screw. The device is made individually based on impressions and is attached with rings or trays to the distant teeth. Using a screw, the device moves apart, stimulating the expansion of the upper jaw.
Stage 2 – Distalization (movement) of chewing teeth.
The chewing teeth that have been displaced due to the early removal of baby teeth must be moved to their place and pushed back. To move the teeth a sufficient distance, the Pendulum device will be used, which applies pressure to individual teeth, causing them to move in a given direction. The device is made individually using dental impressions and is fixed on the teeth for permanent wear.
Stage 3 – Eruption of permanent teeth.
At this stage, the child will not wear any orthodontic appliances, but will only be under the supervision of an orthodontist.
Stage 4 – Teeth straightening with braces.
Braces will be installed on permanent teeth, which will help set the teeth in the correct positions and create physiological interdental contacts.
Throughout all 4 stages of treatment.
It is recommended to undergo treatment by an ENT specialist (to eliminate the causes that interfere with breathing through the nose) and correction of the balance of the facial muscles by a speech therapist - myofunctional therapist to obtain a stable result of bite correction.
Commentary by orthodontist M.P. Sleptsova: “The child is still small, his teeth are only baby teeth, and the narrowing of the upper jaw is significant. Braces cannot correct this; they do not expand the jaw. In addition, sufficient distalization (movement back) of the distant teeth was necessary to prepare the site for the eruption of permanent teeth. Braces cannot cope with this task either. If the parents had not contacted the orthodontist in time, then it would have been possible to straighten the teeth only by removing some teeth or by surgically widening the jaw. It is also important to involve an ENT specialist and a speech therapist in the treatment in order to eliminate the incorrect type of breathing and get a stable result.”
According to the literature and clinical observations, it is noted that in most cases, underdevelopment of the lower jaw, both congenital and acquired, includes not only shortening, but also a significant narrowing of the branch. In the methods described in the literature, the elimination of underdevelopment of the mandibular ramus is performed using horizontal osteotomy and vertical distraction of the mandibular ramus. In this case, the regenerate formed during the distraction process is narrow in width (due to the initial narrowing of the mandibular ramus). The load placed on it during movements of the lower jaw does not correspond to its functional capabilities, which leads to a reduction in the formed regenerate and entails a relapse of the disease. In order to prevent such complications, it is necessary to first increase the width of the branch to create a regenerate of sufficient size that can withstand the functional load placed on it.
To accomplish this task in childhood, the most optimal way is to use compression-distraction osteosynthesis, which is confirmed by a number of studies (Roginsky V.V., 2000, 2001, 2002; Komelyagin D.Yu., 2006; Lekholm, 1999; Binger et al. , 1999). The use of compression-distraction osteosynthesis allows one to avoid complications inherent in bone grafting methods, and restoration of facial symmetry is achieved exclusively through local tissues.
Currently, there are a number of works devoted to eliminating underdevelopment of the lower jaw branch, each of which proposes different surgical techniques. When using compression-distraction osteosynthesis, various modes of distraction and retention periods are indicated; there are no indications for performing distraction at different age periods. All this indicates the absence of a unified approach in the treatment of patients with underdevelopment of the lower jaw branch. In the available literature, no treatment methods or special devices for their implementation have been found that would allow expansion of the mandibular ramus using compression-distraction osteosynthesis.
Material and methods.
From 2010 to 2015, 27 patients with congenital and acquired underdevelopment of the lower jaw branch were treated in the Department of Maxillofacial Surgery of the St. Vladimir Children's City Clinical Hospital using compression-distraction osteosynthesis. The age of the patients was 6–18 years. All patients were divided into the following groups: congenital unilateral underdevelopment of the lower jaw branch - 13 (48.2%); acquired bilateral underdevelopment of the lower jaw branch - 6 (22.2%); acquired unilateral underdevelopment of the lower jaw branch - 8 (29.6%).
The group of patients with congenital underdevelopment of the lower jaw included patients with syndrome of the I-II branchial arches. The group with acquired underdevelopment of the lower jaw included patients with consequences of traumatic and inflammatory diseases of the lower jaw of various origins: consequences of hematogenous osteomyelitis of the head of the lower jaw during the neonatal period - 3 (21.4%); consequences of birth trauma accompanied by a fracture of the condylar processes of the lower jaw - 6 (42.9%); consequences of fractures of the mandibular ramus, condylar process of various levels, for which surgical treatment was performed - 5 (35.7%).
Treatment was carried out according to functional and cosmetic indications. Treatment algorithm for patients with underdevelopment of the lower jaw branch: before starting treatment, all patients underwent a general clinical examination, a general blood test with hemosyndrome, an analysis for group and Rh factor, a biochemical blood test, a general urinalysis, an ECG, an orthopantomography was performed, and diagnostic impressions were taken by the orthodontist. and production of plaster models. After this, spiral computed tomography of the facial skeleton was performed with a step of no more than 1.0 mm according to the program of the paranasal sinuses, followed by 3D reconstruction. Based on the computed tomography data, a plan for the upcoming surgical intervention was drawn up. In all cases, specially designed external compression-distraction devices (CDD) with a stroke of 15 and 20 mm were used.
The CDA for expanding the mandibular ramus consists of a tubular body, inside of which there is a lead screw, on which there are carriages with linear-shaped legs fixed to them, located on both sides of the device body at an angle of 70°. The tarsi have holes for bone screws for attachment to osteotomized fragments. At the end of the lead screw, a cardan shaft is secured by means of a hinged drive, at the end of which there is a head for a socket wrench.
Surgical interventions were performed under endotracheal anesthesia. From a surgical approach in the submandibular region, a CDA was fixed to one or both branches of the lower jaw, and the drive screw of the device was removed through an additional linear incision in the postauricular region. According to the planned scheme, a vertical osteotomy of the jaw ramus was performed along a line parallel to the posterior edge of the mandibular ramus and passing through the middle of the semilunar notch, after which the fragments were compressed, and the wound was sutured. Sutures were removed on days 7–10 after surgery. Distraction began on the seventh day after surgery, 0.8 mm per day: 4 times a day, 0.2 mm, and continued until the width of the jaw branch was reached, similar to the healthy side, or until the apparatus was completely untwisted. During distraction, in order to assess the density of the regenerate and individually select the speed of distraction, an ultrasound scan of the area of regenerate formation was performed 2 times a week. After completion of distraction, an orthopantomogram was performed. When the position of the osteotomized fragments was satisfactory and the required degree of expansion of the mandibular ramus was achieved, the lead screw of the apparatus broke off, and the wound in the postauricular area healed by secondary intention.
The retention period varied depending on the type of pathology: in patients with acquired underdevelopment it was at least 3 months, in patients with congenital pathology it was at least 5 months. After the end of the retention period, an ultrasound and a control orthopantomogram were performed to assess the condition of the regenerate. Removal of the CDA was performed only if there were signs of bone regeneration. If subsequent lengthening of the mandibular ramus was necessary, a new CDA was applied during removal of the apparatus, an osteotomy was performed in the horizontal direction, and vertical distraction of the ramus was performed.
Results.
A good functional and cosmetic result was obtained in all patients - an increase in the width of the mandibular ramus was achieved, when the devices were removed, bone regenerate was discovered, complete restoration of the function of the lower jaw was noted, and facial aesthetics were improved. Healing of surgical wounds occurred by primary intention. The distraction time was 15–28 days. In 4 (14.8%) patients, an individual distraction schedule was established due to the slow formation of the regenerate in patients with congenital underdevelopment of the lower jaw - 3 times a day, 0.2 mm.
Conclusion.
All patients with underdevelopment of the mandibular ramus, if it is narrowed, must have it widened before lengthening the ramus. The degree of expansion of the mandibular ramus must be brought closer to the width of the healthy side to achieve a lasting treatment result. The most optimal way to expand the mandibular ramus is compression-distraction osteosynthesis. The use of a device of the proposed design makes it possible to achieve the following advantages: the presence of fixing legs on both sides of the device body allows you to reliably fix osteotomized fragments, eliminate the possibility of rotation of the fragments along the axis of the device and ensure the formation of regenerated bone density; linear-shaped fixing legs are completely placed on the branch of the lower jaw, which allows for rigid fixation (6 screws for each osteotomized fragment), ensuring gradual adaptation of the surrounding soft tissues to the changing size of the branch, creating an objectively controlled volume of bone tissue, which increases the effectiveness of this method and low risk of complications and relapse; rigid fixation of bone fragments provides the possibility of early functional loading; the location of the fixing legs at an angle of 70° allows for distraction parallel to the occlusal (chewing) plane, which leads to the formation of the mandibular branch of the correct shape (the angle of the lower jaw is located in line with the base of the lower jaw); the presence of fixing legs remote from the front end of the device body makes it possible to completely position the KDA body inside the tissues, which allows you to remove the drive screw in the most acceptable cosmetic area, and after distraction, remove the drive screw, allowing the wound to heal in the place where it is located and to exclude contact of the device with environment; the ability to significantly expand the mandibular ramus (up to 2.0 cm). Taking into account the above-described features, this method can be used both in preschool children and adolescents 16-18 years old.
External manifestations and consequences for the body
Having understood what prognathia is and why it occurs, we can move on to the question: is it worth treating? After all, this is not congenital or acquired adentia, when there are no teeth at all - in this case, you cannot do without the help of a dentist, at least to restore normal chewing. But with bite defects, all the teeth are in place - so why carry out treatment then?
Let's start with the issue of aesthetics. With physiological prognathia, the alveolar processes (that is, the anatomical part of the upper jaw in which the teeth are located) and the front teeth are tilted forward. When you smile, you immediately notice that they protrude forward at an angle.
In a person with such a developmental anomaly, the lower jaw is small, and the upper jaw hangs over it, causing the proportions of the face to be disrupted. The face looks disharmonious and even unpleasant: as if a dissatisfied expression was forever frozen on it.
Proper chewing of food with this position of the teeth is also difficult. The worse a person chews food, the higher the risk of developing gastrointestinal diseases. In addition, incorrect positioning of teeth often causes diction defects. Due to the fact that the entire dental system does not work correctly during prognathia, over the years a person develops problems with the temporomandibular joint. The most noticeable manifestation of such problems for the patient is the clicking of the jaw when chewing food, opening or closing the mouth. Also, diseases of this joint cause headaches, tinnitus, and sometimes even insomnia.
And finally, such a malocclusion provokes serious dental problems. Due to the atypical distribution of chewing load, the frontal zone is almost not involved in the work of the dental system. However, if almost the entire load falls on the chewing teeth, then they begin to quickly deteriorate, including due to increased abrasion. The gums in the chewing area often become inflamed, which increases the risk of tooth loss.
Moreover, in the case of prognathia, orthopedic treatment is very complicated and sometimes almost impossible. Dentures (crowns, veneers, bridges) often break due to abnormal closure of the dentition. In addition, the orthopedic dentist will not be able to fix them well enough.