Local swelling of the root zone, compactions of various sizes, throbbing pain, sensitivity to temperature when eating, enlarged lymph nodes may indicate an acute inflammatory process of infectious etiology. In dentistry, there are several types of diseases, among them periapical abscess. It can be caused by advanced caries, chipping of an element of the dental system, overheating of the pulp due to tooth preparation and various pathologies. This can also happen due to poor-quality root canal treatment.
A periapical tooth abscess is an accumulation of pus between the molar and the gums. Purulent exudate can accumulate both in the inner and outer surfaces of the alveolar process of the lower or upper jaw. It most often begins in a tooth with a non-viable pulp, when the nerve dies, causing infection and progressive inflammation. The infection may gradually spread to surrounding tissue. Clinical symptoms are in many ways similar to acute periodontitis. The patient experiences increased sensitivity, acute pain, the mucous membrane may have swelling, there is active hyperemia, and overflow of blood in the vessels of the circulatory system.
Symptoms
- Intense dull throbbing pain.
- Discomfort when chewing food.
- Swelling in this area.
- Painful sensations when swallowing.
- Enlarged lymph nodes.
- Unpleasant sensations when opening the mouth.
- Change in molar color.
Other symptoms also include malaise, fever, weakness, and bleeding. It should be noted that in some cases the inflammatory process can be practically asymptomatic; activation can occur periodically, for example in the case of hypothermia. In this case, immediate assistance from a dentist is required so that he can quickly and accurately diagnose and establish a treatment regimen for effective recovery.
Causes of abscess
Complications associated with the inflammatory-destructive process can occur due to the following reasons:
- Poor quality endodontic treatment.
- Carious formations.
- Injuries to elements of the dentition.
- Unqualified prosthetics.
- Infectious diseases in the maxillofacial area, such as sinusitis.
Treatment of a periapical abscess without a fistula may be required in case of violation of the endodontic therapy protocol or incomplete obturation of the canal system. Provoking factors can be serious infectious diseases, hypothermia, and a reduced level of the body's immune defense. Leukocyte infiltration also often causes the formation of an abscess and microabscess.
Reasons for development
The appearance of a purulent neoplasm in the oral cavity can be provoked by:
- failure to consult a doctor in a timely manner for the treatment of caries or periodontitis,
- penetration of filling material beyond the root canal during dental treatment,
- jaw injury,
- necrosis of the neurovascular bundle,
- inflammation of soft tissues in the oral cavity.
The risk of tissue suppuration is increased by weak immunity, frequent infectious diseases, vitamin deficiency and other factors that weaken the body as a whole.
Kinds
Based on the nature of the localized accumulation of pus in the elements of the dentition and nearby structures, two groups of abscess are distinguished.
- Periapical abscess without fistula. In this case, transcanal infection of periodontal tissue is observed. The adjacent gum may have swelling, hyperemia is observed, pain is felt when biting on a molar, and the appearance of purulent exudate is recorded. The disease has a pronounced clinical picture.
- Periapical abscess with fistula. With this phenomenon, the inflammatory destructive process spreads to the bone marrow and mucous membrane. The fistula most often opens in the projection of the apex of the root element of the dentition. There may be hyperemia on the mucous membrane, a scar from a fistula, and the gums may be quite sensitive to palpation.
In case of periapical abscess without a cavity and with a cavity, complaints of intense dull throbbing pain, deterioration of general condition, and constant pain are recorded.
Treatment of periapical destructive changes in bone tissue
One of the most important problems that dental surgeons face in their daily practice is the treatment of patients with periapical destructive changes (chronic periodontitis and root cysts).
Analysis of the reasons for unsuccessful treatment of patients indicates that progress in this issue should be associated with improving the technology of surgical interventions and creating optimal conditions for bone tissue regeneration.
This is especially important for large bone defects of the jaws remaining after removal of the pathological focus, since around it the reparative processes are suppressed due to the frequent development of inflammation, which is observed in 47-56% of patients.
After tooth extraction surgery, root apex resection and granulomectomy, osteoblastic and osteoclastic processes occur in the alveolar process of the jaw.
In this regard, the need for targeted use of osteostimulating agents that would create optimal conditions for reparative osteogenesis is obvious.
We have found that during periapical destructive processes, streptococci predominate, and neomycin and ciprofloxacin are the most effective chemotherapeutic drugs against microorganisms.
Based on these data, the method of saturating a bioimplant with an antimicrobial drug using low-frequency ultrasound is scientifically substantiated, which is used in the developed new method for treating suppurating periapical changes (patent for invention No. 2189191 dated 04/05/2001).
In an experiment on rabbits, the features of the restructuring of an allogeneic sponge bioimplant were studied. Its high plastic properties have been revealed.
All this made it possible to obtain scientific data confirming the effectiveness of our proposed method of treating suppurating periapical destructive changes using a bioimplant with an antimicrobial effect.
When studying the nature of reparative osteogenesis of tooth sockets, during their plastic surgery with demineralized bone brefoosteomatrix in experimental animals, high osteoinductive properties of demineralized brefoosteomatrix were established when filling tooth sockets and replacing bone defects formed after organ-preserving operations.
Anthropometric methods of research on plaster models of the upper and lower jaws in patients revealed that the use of demineralized brefoosteomatrix helps to reduce the degree of post-extraction atrophy of the alveolar process of the jaw by 1.7 times, and the combined action of low-frequency ultrasound and antiseptics allows in 84.2% of cases to achieve sterility of the bone wound .
A method has been developed for the preoperative preparation of formalized demineralized brefoosteomatrix in order to reduce its cytotoxic properties, which consists of grinding the graft, placing it in a 0.9% sodium chloride solution for 60 minutes (with sonication for 2 minutes) and repeated sonication for 2 minutes in 0.2% chlorhexidine bigluconate solution (frequency 26.3-26.9 kHz, amplitude 30-35 µm).
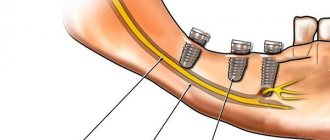
The reparative processes of osteoplastic correction of the alveolar process of the jaw with brefoosteomatrix for subsequent endosseous integration of dental implants were studied.
It was revealed that the volume of bone regenerate after 6 months corresponds to the volume of the former defect and represents organized spongy bone.
Positive treatment results were obtained in 95.4% of patients, complications were observed in 4.6%.
Diagnostics
Diagnosis of an acute inflammatory process of infectious etiology with localization in the hilar region includes a visual examination and radiographic examination. In some cases, thermography may be performed. The dentist assesses the condition of the mucous membrane, hyperemia of the tissue, and changes in tooth color. X-ray examination helps to assess the location of the pus. At the diagnostic stage, the specialist determines the viability of the pulp.
A clinical study allows us to determine the degree of pathology and select the correct endodontic treatment or surgical intervention. If necessary, additional examination methods may be required to determine the condition of the periapical tissues. In each specific case, the treatment method is selected individually depending on the history and clinical examination. The patient’s age, local symptoms, and the presence of general diseases are also taken into account. Additionally, microbiological diagnostics can be performed to identify various types of microbial pathogens.
Diagnosis and treatment
The doctor begins the diagnosis with a general examination. An abscess may appear as a small, red and inflamed lump. The fistula may ooze pus. To determine the size of the tumor, a picture is taken. It also eliminates damage to periodontal and bone tissue.
The first stage of treatment is always the removal of purulent contents. If the fistula is not open, the doctor makes an incision in the gum and installs a drain to ensure the drainage of pus. The next step is opening the tooth cavity. The doctor removes the dead pulp and performs root canals to reduce the risk of relapse. When the inflammation is stopped, the tooth is filled.
If treatment is not possible, the doctor will remove the affected tooth and then clean the capsule of purulent contents. Following treatment or removal, you must take prescribed antibiotics to reduce the risk of infection spreading.
Treatment of periapical abscess
Depending on the stage and form of the pathology, the specialist selects a therapeutic or surgical method of treatment. At the initial stage, the canals are usually cleaned, in particular the elimination of pathogenic microflora between the teeth and gums, and the cavity is treated with antibacterial components. Endodontic therapy may include the installation of a temporary filling and the application of an antiseptic dressing with antimicrobial properties in the root canal. Antibiotics may be prescribed to stop the inflammatory process.
High-quality endodontic therapy allows you to eliminate the infectious focus. As inflammation increases, an element of the dental system can be removed. In some cases, the specialist performs appropriate tooth-preserving procedures, for example, hemisection, that is, removal of one of the molar roots.
The opening of an abscess is always performed using anesthesia; discomfort and pain are excluded during high-quality endodontic treatment. After the abscess removal procedure, drug therapy and surface treatment with special bactericidal compounds may be prescribed. The final step is to take an x-ray to ensure complete recovery.
The specialists of the AlphaDent clinic are always ready to help if you have complaints about a periapical abscess without a fistula or with a fistula. Dentists have the necessary knowledge and sufficient experience to provide high-quality endodontic treatment.
Qualified treatment will eliminate the recurrence of the infection that caused the abscess. Timely dental care will help keep your teeth and mouth in good condition. It is recommended to make visits to the dentist for preventive examinations in order to exclude complex endodontic treatment associated with the removal of an abscess.
Periapical dental x-ray
Periapical dental x-rays, along with interproximal x-rays, are targeted x-ray examinations. Simply put, such an x-ray allows you to take an individual “photograph” of a specific tooth, a maximum of two neighboring ones.
This type of diagnosis has another name – root snapshot. It is done in a vertical plane and reflects not only the crown of the tooth, but also the root. Moreover, the image also captures part of the gum, as well as the bone tissue around the root of the tooth and below the apex - the apical part of the root tip.
Thus, on a periapical image you can see not only painful phenomena in the tooth root or periodontal tissues, but also pathological processes occurring in neighboring tissues - abscesses, the formation of cysts and granulomas, and so on.
Thus, a common phenomenon in advanced dental diseases is a periapical abscess. With a progressive inflammatory process, when tissue begins to break down and the pulp dies, an abscess can occur without pain. In such cases, periapical x-ray allows a definitive diagnosis.
Periapical x-rays of teeth are simply necessary for endodontic therapy - root canal treatment. Most often, dentists send patients with suspected pulpitis for such an x-ray - inflammation of soft tissues with neurovascular endings in the tooth cavity. In this case, an image can give a complete picture: what is the source of damage to the root and whether the inflammatory process has spread to neighboring tissues.
When performing pulp removal, it is also important for the dentist to know the individual characteristics of the patient’s root canal structure. Sometimes the diseased root may “hide”, then it will be necessary to take a repeat periapical photograph, while correcting the angle.
You may also be sent for a periapical dental x-ray after treatment. This is necessary for the doctor to make sure that the root canal is sealed completely and tightly. After all, the remaining cavities can lead to new inflammatory processes.
Thus, according to classical methods, during endodontic treatment it is necessary to take at least three periapical images: upon treatment - a diagnostic image, then an x-ray to determine the size of the tooth canal and, finally, a control image.
Root photographs are sometimes prescribed for mechanical dental trauma. If the damage is fresh, then from such an image a dentist can easily diagnose a fracture of the tooth, in particular, its hard structures.
Periapical photographs are also taken for those who plan to install an implant. Such an x-ray is necessary to assess the height of the vertical bone structures in the implantation area. Sometimes, in order for the implant to hold securely, the jawbone is augmented with bone materials.
Unfortunately, periapical dental x-rays alone cannot always provide an accurate picture of the condition of the tooth. Some details in such a photo may be distorted. In particular, periapical images provide a poorly informative image of the crown. From such an image it is not always possible to see the presence of carious cavities, or to understand the relationship between the root and the crown. Therefore, periapical dental x-rays are most often done during initial diagnosis and at the end of treatment to assess the quality of the work.
If necessary, the dentist may require additional bitewing or panoramic X-rays during treatment. But you shouldn’t be afraid of modern X-rays. New generation digital devices make this procedure safe for the health of patients.