Corrective osteotomy of the knee joint is a proven method of surgical treatment of deformities of the tibia and femur. This operation reduces the load on the articular surfaces, eliminates existing pathologies and slows down the degeneration of the lower limb.
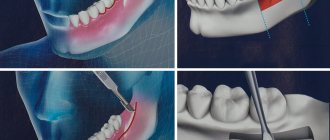
Schematic representation of the operation.
What is a knee osteotomy?
Corrective osteotomy of the knee joint is an operation that eliminates congenital and acquired bone deformities. During surgery, the doctor excises a pre-designated area of bone tissue and connects the loose bone fragments with implants. As a result, the axis of mechanical load is transferred to the healthy area of the joint. The operation is performed under complete or spinal anesthesia. After treatment, the orthopedist immobilizes the patient's lower limb with a plaster cast during recovery. Rehabilitation is underway.
Osteotomy with metal structure.
The described correction method is traditionally compared with knee replacement. Osteotomy is a less traumatic treatment method. This medical procedure is perfect for young patients suffering from late stages of gonarthrosis. The choice of osteotomy as a method of restoring mobility of the lower limb makes it possible to delay endoprosthetics for a long time.
Osteotomy has been used for two centuries. After the discovery of replacement arthroplasty methods, this surgical intervention faded into the background, but this method of treatment is still used. At the beginning of the 21st century, modern methods of fixing bone areas were developed, reducing the duration of rehabilitation.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Possible complications
Some complications arise already during osteotomy, others during the rehabilitation period.
- Incorrect fusion of bones. Occurs due to improper fixation of bone tissue fragments during surgery. With such a complication, repeated intervention is necessary.
- Non-union of bones. It may occur due to severe concomitant pathologies, smoking, impaired blood supply to the operated area, or osteoporosis. For treatment, a repeat operation is performed and special rehabilitation is prescribed.
- Compartment syndrome. Occurs if, during surgical manipulation, the muscles were strongly compressed by a tourniquet. For treatment, certain drugs are prescribed; if the case is severe, a fasciotomy is performed.
- Improper functioning of the joints located next to the surgical field. This complication is typical for the absence or violation of rehabilitation rules. Exercise therapy is prescribed.
- Infections. They can be introduced during surgery or due to improper wound care. An antibiotic is prescribed for treatment; in severe cases, revision surgery will be required.
- Nerve damage is a surgeon’s mistake or a peculiarity in the location of the patient’s nerve endings. The function of a damaged nerve cannot be restored.
- Thromboembolism. Occurs when anticoagulants are prescribed incorrectly, getting out of bed late, or the inability to wear compression stockings. To eliminate this complication, high doses of antiplatelet agents and anticoagulants are needed.
Indications for surgery
The main indication for surgical intervention is gonarthrosis. This is a degenerative disease of the knee joint, manifested by the gradual destruction of cartilage tissue and deformation of the lower limb. In the later stages of gonarthrosis, patients develop valgus and varus deformities. The range of motion is limited, and chronic pain occurs.
Arthrosis of the condyle.
Other indications:
- Congenital deformity of the lower limb.
- Curvature of bones after injury.
- Preparation for knee replacement surgery.
- Displacement of the axis of the lower limb in pathologies of the articular ligaments.
- Rickets, osteitis deformans and other bone diseases.
The intervention is recommended for satisfactory condition of the cartilaginous surface of the bones and isolated damage to one area of the knee joint. This correction method makes it possible to maintain mobility of the lower limb in young patients.
The essence of the operation and the result
The main goal of the intervention is to distribute pressure and friction evenly across the knee joint, reducing this impact on the most affected areas by loading those that are more preserved and functional.
As a result, the axis of the load on the limb is shifted, giving it a more physiological position, and, as a result, a more balanced distribution of the load (and let us remember, when walking it is about four body weights on one knee, when running - about eight), and reducing pressure on the “sick” area of the joint surface.
In what cases will osteotomy not help?
The effectiveness of treatment depends on the age, gender and body weight of the patient. Unsatisfactory results of the operation may be due to the patient's advanced age, significant bone damage and destruction of hyaline cartilage.
Conditions in which intervention is inappropriate:
- rheumatoid arthritis;
- osteoporosis;
- extra-articular pathologies;
- lack of blood supply to the lower limb;
- impaired bone growth;
- absence of meniscus;
- severe obesity (BMI: 40 and above).
If the indications are not properly assessed, osteotomy can accelerate degeneration of the knee joint. Before treatment, doctors conduct laboratory tests, take photographs of the lower limb along its length and prescribe additional diagnostic procedures.
Soft tissue operations
Operation Silver
The essence of the technique is cutting off the tendon of the adductor muscle of the big toe. As a rule, it is one of the stages of combined techniques.
Operation McBride
The adductor tendon is not simply cut off, but transferred. Quite often combined with Shede's operation.
The illustration shows the creation of a “tunnel” through the metatarsal head and the passage of the adductor tendon through it. In various modifications of McBride, the tendon can be sutured to the capsule and head of the metatarsal bone, or fixed on the back of the head. The modifications have the same goal: to reduce the angle between the metatarsals.
Operation Mann (RA Mann)
Distal soft tissue procedure. It is currently an integral part of many combined operations. The goal of the procedure is to restore the position of the sesamoid bones in the thumb area.
Sesamoid bones are displaced laterally during valgus deformity. Returning them to their previous anatomical position is carried out by cutting off the tendon of the adductor pollicis muscle from the lateral sesamoid bone, excision of the lateral collateral ligament, making releasing incisions on the outer surface of the joint capsule and intersection of the metatarsesamoid ligament. It can be performed through an arthroscope. In this case, the traumatic nature of the operation is significantly reduced.
Types of surgical techniques
Interventions are classified according to the location, method of tissue excision and the nature of bone grafting. The structure of the tibia or femur is corrected. Classification according to the nature of the plastic surgery includes open, closed, lateral and direct osteotomies. Tibial correction can be high or low. The specific surgical technique is selected by the doctor individually based on the results of a preliminary examination.
Main types of osteotomy:
- Wedge-shaped closed. A skin incision is made in the lateral or anterior region of the knee to access the superior epiphysis of the tibia or the inferior epiphysis of the femur. After excision of the tissue, the free surfaces of the bone are fixed with metal plates or staples.
- Wedge-shaped open. After a skin incision is made in the anterior or lateral area of the knee, a partial osteotomy is performed. The end of the tibia separates into two parts to form a diastasis. Next, the bone areas are connected with a metal plate and an autograft from the patient’s pelvis.
Knee osteotomy: visual representation of the procedure.
The bone tissue is removed using an osteotome. To prevent damage to the vessels and nerves passing through the knee joint, the correction is carried out under the control of a fluoroscope or X-ray machine. After plastic surgery, the skin is stitched and the lower limb is fixed with a plaster cast or splint.
There is no single method of surgical intervention suitable for any indication. When choosing a surgical technique, the doctor takes into account the planned correction angle. Imaging methods help more accurately restore the axis of the lower limb. In modern orthopedics, an open wedge osteotomy of the tibia above the level of the tuberosity is most often performed.
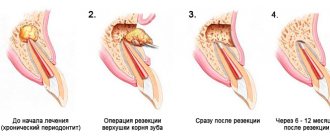
Sequence of maxillary osteotomy
The orthodontist is the first to treat any malocclusion. Then - dental surgeons.
- An orthodontist installs braces on the upper and lower jaws to straighten the teeth. For some period of time (~9-10 months), because of this, the teeth stop closing.
- The patient is given general anesthesia. The incision is made from the palatal side (from the inside of the mouth) so that there is no scarring. Cuts are made on the jaws, bone fragments are set in motion and placed so that the shape of the face is most attractive. The new position of the jaws is secured with small titanium plates, which take root well, do not ring metal detectors at the airport, and allow MRI scans to be performed without difficulty. Most often, the plates remain in the body forever and are not felt at all. The muscles, mucous membranes and other tissues are sutured so that there are no disturbances in the nearest nerve branch, an antiseptic bandage is applied to the wound, and the person is taken to the ward to wake up after anesthesia.
Rehabilitation
Long-term treatment results depend on rehabilitation measures. After surgery, the doctor conducts follow-up examinations and selects methods for restoring mobility of the knee joint. The goals of rehabilitation include pain relief, prevention of postoperative complications, and restoration of the muscular system of the lower extremity.
Rehabilitation methods:
- Physiotherapy: electrical stimulation, cryotherapy and heat. Physical therapy relieves pain and reduces tissue swelling in the postoperative period.
- Massotherapy. Manual therapy improves blood flow in tissues, relieves pain and normalizes muscle tone.
- Physiotherapy. Exercises can be done at home. The main task is to restore flexion and extension movements in the knee joint.
- Orthopedic rehabilitation to prevent relapse of the disease. The patient is advised to wear a knee brace or elastic bandage to secure the joint. For the first time after surgery, it is necessary to use a cane and wear shoes with orthopedic insoles to reduce the load on the articular surfaces.
The rehabilitation plan is drawn up by an orthopedist and a physical therapy doctor. Drug therapy is selected. Full restoration of motor activity occurs within a year.
Advantages of the method
- Relatively low invasiveness of the intervention. Surgical access is achieved by making an incision of only about one centimeter;
- follows from the previous one. This manipulation does not always require anesthesia, and in the vast majority of cases it is performed using regional, spinal or epidural (less often) anesthesia;
- as a result of the manipulation, the patient is discharged from the clinic with his knee completely preserved, and, subject to a number of conditions, a complete restoration of its functions is possible;
- the duration of the operation is about one and a half hours, it is well studied, with many years of experience;
- length of hospital stay is about three days;
- the time to return to the full range of activity of the limb is about two months.
Life after treatment
The prognosis is determined by the initial diagnosis, the chosen surgical treatment technique, the surgeon’s qualifications, the patient’s age and other criteria. According to the G. A. Ilizarov Medical Center, positive results were noted in 95% of patients after the intervention. For 10 years after bone grafting, there is no pain or other symptoms of gonarthrosis. Young people who have undergone osteotomy return to a full life after rehabilitation. Subsequent replacement arthroplasty is facilitated.
The long-term results of the correction are difficult to predict. Patients are advised to regularly visit an orthopedist and undergo examinations to monitor the condition of the joint. Osteotomy as an independent treatment method does not completely eliminate arthrosis, but only slows down the development of degenerative processes. In some patients, relapse occurs as early as 4 years after the intervention.
Among the methods of surgical expansion of the atrophied alveolar ridge (AC), a special place is occupied by intercortical osteotomy, based on the vestibular movement of the outer cortical plate in the edentulous area [1, 4, 5, 11, 15, 16].
Its advantages in achieving long-term results of dental implantation are presented in a number of publications [2, 3, 8, 10], etc. However, it is reported that it is problematic to ensure the primary stability of a dental implant (DI) and the optimal thickness of the soft tissue covering it, or the so-called biological the width of the adjacent gum, which is understood as the zone of connective tissue and epithelial attachments to the coronal part of the bone crest [9, 13, 14]. There are also conflicting opinions about the structure of the cut-out flap, which promotes better blood supply to the osteotomized fragment in the postoperative period [14, 17], and the rationality of simultaneous elimination of soft tissue deficiency [6, 7, 12].
This report presents the main surgical stages of the AMCO alveolar intercortical osteotomy technique, patient selection criteria and some aspects of the prevention of postoperative complications.
Surgical intervention begins with cutting out a combined (full-thickness in the caudal part, split-thickness in the cranial part) flap on the outer side of the corrected area of the AH, where dental implantation is planned; then, through an intercortical osteotomy, vestibular movement of the outer bone wall is performed to increase the width of the ridge.
Dissection and detachment of soft tissues
Rice. 1. An incision along the ridge and skeletonization of the vestibular surface of the coronal part of the alveolar process.
A linear horizontal incision is made:
— within the keratinized attached gum;
- along the apex or palatal cranial edge of the ridge, in the space between 2 adjacent teeth or supposed vertical cuts (in the absence of teeth);
- with dissection of the periosteum, i.e. to the bone;
— in the form of intrasulcular and marginal incisions in the area of the gingival papillae of adjacent teeth, while the gingival edge of the tooth neck remains intact.
An important condition when dissecting tissue is, if possible, preventing the lines of bone cutting and suturing the edges of the wound from coinciding in order to reduce the likelihood of developing postoperative complications in the form of divergence of its edges and infection.
Peeling of the combined flap begins with skeletonization of the apex of the bone AG approximately 3-4 mm from the vestibular (crossing the mucogingival border) and palatal sides, including in the projection of adjacent teeth. In fact, at this stage of the operation, the coronal part of the vestibular flap is cut out, including the periosteum (Fig. 2).
Rice. 2. Formation of a combined flap; in the coronary part the flap includes the mucoperiosteal layer, and in the apical part it includes a split layer.
Next, the periosteum is dissected along the entire length of the flap (Fig. 3), penetrating with the tip of a scalpel into the wound 1-2 mm parallel to the surface of the bone (to prevent perforation of the usually thin mucous membrane in this area - SO) with the intersection of the existing muscle attachments. Further detachment of the flap is performed: a) acutely; b) on top of the periosteum, i.e. in the submucosal layer; c) to the projection of the upper fornix of the vestibule of the oral cavity, holding the scalpel parallel to the surface of the movable S.O. Thus, the large or apical part of the combination flap, approximately 6-7 mm wide, is split, since the periosteum is not peeled off. This allows you to preserve the blood supply to the bone and increase the mobility of the relocated flap, while avoiding additional vertical loosening incisions, which has a beneficial effect on the trophism of local soft tissues.
Rice. 3. Mobilization of the flap by linear incision of the periosteum.
In those clinical observations when, in order to improve the long-term functional and aesthetic results of AMCO, it is necessary to increase the volume of the attached gum (if its thickness is less than 2 mm) and (or) eliminate recession in teeth adjacent to the implantation zone, the so-called bilaminar technique according to G. Zucchelli is used (2013), the essence of which is the coronal movement of the vestibular flap in combination with a free connective tissue graft (CTT).
When expanding the edentulous narrow AG in the frontal part of the upper jaw (MF), it is necessary to take into account that the contour of the outer surface of its ridge usually has a concave shape, which is unfavorable for achieving aesthetic results of dental implantation. Recreation of the convex shape of the outer contour of the ridge is achieved as follows: immediately after a horizontal cut to a depth of 8-10 mm, a wedge-shaped chisel is installed into the resulting intraosseous lumen and expanded to 2 mm, then in the projection of the planned dental implantation a drill with a diameter of 2.0 mm is used to form osteotomy hole, which is gradually enlarged in the bucco-lingual direction using a special set of expanders1. By successively using expanders of increasingly larger diameters, they compact the spongy substance, move and “straighten” the outer bone wall, the thickness of which, as has been repeatedly noted, should be at least 2 mm. Next, vertical cuts are made through intraosseous access in a manner similar to that described. In addition, a feature of surgical intervention in the anterior part of the HF is the location of the DI neck deeper than the cemento-enamel junction by 3 mm, which corresponds to the biological width. The latter, as is known, is composed of 3 anatomical structures of the gum: the gingival sulcus, zones of epithelial and connective tissue attachments.
Intercortical osteotomy
carried out using 2 cuts, starting with a horizontal one in the middle of the apex of the bone AG (Fig. 4); then 1 vertical cut is made from its medial and lateral ends. The splitting of the ridge within the made cuts is carried out by vestibular movement of the outer cortical plate according to the type of subperiosteal fracture at its base.
Rice.
4. Horizontal cut in the middle of the apex of the AG using a piezo scalpel. The success of horizontal cutting is ensured by the following technical techniques: a) minimize bone loss during splitting using thin instruments (piezo scalpel, diamond disk, cutters, sharp chisel, etc.); b) crest osteotomy is performed to the cancellous bone and somewhat in the outer direction, maintaining the thickness of the vestibular bone plate (VBPL) within 2.0-2.5 mm; c) all bone cuts are made at a distance of at least 2 mm from the roots of adjacent teeth.
Vertical loosening dissections of the compact layer of bone (Fig. 5) are performed: a) with a piezo instrument or a fissure carbide bur installed intraosseously, followed by advancement to the vestibular side; b) perpendicular to the horizontal cut, starting from the top of the ridge (from its medial and lateral ends, respectively) for approximately 8-10 mm; c) at a distance of at least 2 mm from the projection of the periodontal ligament of the tooth adjacent to the intervention zone; d) being careful not to injure the proper periosteum.
Rice. 5. Vertical cuts were made in the compact layer of bone.
The osteotomy is completed with a thin pointed chisel, which, through a horizontal dissection of the bone, is installed into the resulting gap between the outer and inner cortical plates to the depth of the vertical cuts (Fig. 6). In this intraosseous position, the chisel is tilted vestibularly from the basal part of the ridge, and at the base of the osteotomized bone fragment it is broken (a “greenstick” fracture) on the periosteal pedicle and moved. To control the displacement of the fragment, the index finger is placed on the outer surface of the VCP. The palatal bone plate must remain intact.
Rice. 6. A thin chisel is inserted into the cut to carry out the final stage of the osteotomy.
At this stage, the resulting wound defect is assessed to determine the advisability of immediate or delayed implantation according to the standard protocol. Depending on the stability of the displaced VCP on the periosteal pedicle, implantation can be carried out in 1 or 2 stages. It is very important that after the splitting is completed, the minimum thickness of the bone walls is at least 2 mm; otherwise, it is recommended to use delayed D.I. setting. In a two-stage protocol, the intraosseous space is first filled with osteoplastic material (OPM) and implantation is performed in a delayed period after bone regeneration has been achieved. The use of OPM also makes it possible to prevent the return of split cortical plates to their original position. Small gaps (1 to 3 mm wide) are often restored without additional bone grafting. When performing dental implantation, the resulting intraosseous space is additionally filled with autologous bone chips obtained using burs or a scraper. To improve graft stabilization, a barrier membrane is used.
Formation of the bone bed and installation of DI
After completion of the intercortical osteotomy at the level of the base of the AH, guide holes are prepared using cutters with a diameter of no more than 2-2.5 mm of the corresponding implant system, which are installed during the same surgical intervention, provided that sufficient primary stability of the externally retracted VCP is achieved (Fig. 7). In this case, it is necessary to minimize its trauma by: a) preserving cancellous bone on it; b) palatal position of the osteotomy hole (taking into account the dentoalveolar arch and occlusion); c) carefully screwing it into the formed DI bed (Fig. 8).
Rice. 7. The vestibular bone wall is retracted using an expander.
Rice. 8. The bone expander is screwed into the prepared implant bed.
In the lateral section of the HF, a prerequisite for successful primary stability of the DI is its immersion by 2/3 of its length into the bone tissue and 0.5-1 mm below the free coronal edge of the ridge. For the same purpose, a movable VCP can be additionally attached to the palatal bone wall using microscrews. To prevent ingrowth of surrounding tissues, a plug is installed in the internal threaded channel of the DI (Fig. 9).
Rice. 9. Installation of intraosseous DI.
When deciding to carry out delayed implantation, the surgically created gap between the cortical plates must be filled with osteoinductive and (or) osteoconductive material (Fig. 10), which is left for 4-6 months. A mixture of autogenous bone chips obtained from nearby areas using a bone scraper and xenogeneic material (Bio GEN, Gen Os, Easy Graft, etc.) is used as OPM. If necessary, provide coverage of the OPM with a barrier membrane, which is installed under the inner surface of the detached mucoperiosteal flap so that it covers the entire outer surface of the introduced material.
Rice. 10. The bone deficiency is filled with bone replacement material, and a bioresorbable barrier membrane is laid.
Suturing the edges of the surgical wound
Rice. 11. Suturing the wound.
After completion of the regenerative intervention or installation of the DI, the cut out flap is moved caudally and, without tension, fixed with separate interrupted and horizontal mattress sutures (5/0 or 6/0 diameter) to the original attachment site. At the same time, the existing removable or bridge prosthesis is relined to prevent contact with the surgical wound.
Patients with removable dentures are not recommended to use them until the sutures are removed (i.e., within 10-14 days after surgery). Subsequently, the removable dentures are repositioned so that they do not place excessive pressure on the implantation area.
It should be understood that in some cases, AMCO is the most realistic treatment option that allows for optimal results. Deep knowledge of the topic of anatomical bone and soft tissue structures, analysis of these and clinical and radiological data before the upcoming surgical intervention can reduce the risk of unforeseen technical problems associated with it and unwanted side effects in the postoperative period.
The South Korean Split help kit contains 5 expanders with a diameter of 2.5 to 4.5 mm, which makes it possible to install a DI of the optimal size.
What are the dangers of malocclusion?
- Violation of dental contacts makes it difficult to chew food and provokes the development of diseases of the gastrointestinal tract.
- Severe malocclusions so limit the possibilities of normal nutrition that they are a reason for deferment from the army.
- Changing the angles of inclination of the teeth affects the distribution of the load during chewing, leads to overload of the periodontium, the development of gum inflammation and, ultimately, earlier tooth loss.
- Teeth crowding, combined with misalignment, affects the natural cleaning of teeth, further leading to the development of gum disease and an increased likelihood of tooth enamel destruction. If tooth loss has already occurred, then violations of the jaw relationships can create difficulties in prosthetics.
- Malocclusion leads to a change in the trajectory of jaw movement during chewing: the temporomandibular joints are overloaded, and dysfunction of the temporomandibular joints develops.
- Some types of malocclusion are anatomical prerequisites for narrowing the airways, for the appearance of snoring and such a serious condition as sleep apnea.
Jaw osteotomy surgery
Historically, the first operations were performed on the lower jaw. And the surgeon’s task was precisely to restore normal jaw relationships. But today operations on the lower jaw alone account for no more than 10% of operations performed. Because the surgeon’s tasks have changed: now it is not only the correction of the bite, but also the improvement of facial aesthetics.
Double-jaw osteotomy is an operation on the lower and upper jaw simultaneously, which allows you to achieve aesthetically favorable proportions of the face both in front and in profile, eliminate asymmetry, and make the smile brighter by eliminating dark corridors - shading of the lateral teeth of the upper jaw. We can say that surgery on one jaw is only a correction of functionality, on two – functionality and aesthetics.
Indications for the operation:
- violation of the closure of the dentition, which cannot be corrected orthodontically;
- pronounced facial disproportions that have aesthetic significance.
Contraindications:
- unpreparedness of the dentition for surgery (insufficient orthopedic or orthodontic preparation);
- diseases of internal organs that prevent surgery or anesthesia.