Dental prosthetics is an invaluable invention that has impacted the quality of life of many dental patients. What is prosthetics? This is the only possible way to replace lost teeth, which restores the integrity of the dentition, which means it returns chewing function, comfort and a beautiful smile to people. In modern dental prosthetics, various highly effective methods, technologies, and high-quality safe materials are used. With the help of modern orthopedic structures, it is possible to restore the dentition with edentia of any complexity. However, under certain circumstances, after prosthetics, the patient may encounter complications. In this article we will talk about the risks of prosthetics and how they can be avoided.
What complications arise during dental prosthetics?
The most common problems that occur after dental prosthetics are:
- pain, discomfort in the mouth;
- irritation of the mucous membrane, denture stomatitis;
- dysfunction of the temporomandibular joint;
- galvanic syndrome;
- periodontitis;
- decementing and destabilization of fixed orthopedic structures;
- damage, chips of the facing material of crowns, dentures;
- failure of fixed dentures
- intolerance to orthopedic construction materials.
We will tell you in detail about each problem.
Discomfort from the prosthesis
This problem may arise due to errors during installation of the structure or in the event of a mismatch between the denture and the size and shape of the jaw.
What kind of discomfort can we talk about?
- 1
the prosthesis interferes with the normal pronunciation of words; - 2
there is a constant sensation of a foreign body in the oral cavity;
- 3
the prosthesis rubs contact surfaces (mucosa, gums);
- 4
salivation increases.
Discomfort from wearing a new denture for a few days to 2 weeks is normal. If discomfort in the mouth does not go away for a long time, you need to contact an orthopedic dentist to correct the orthopedic structure itself or correct installation errors.
Accelerate the process of getting used to the prosthesis
- Rinse your mouth with a salt solution;
- Take the process of cleaning your denture seriously;
- Try sucking on lollipops, this process calms you down and distracts you from having a foreign object in your mouth;
- To improve your diction, say tongue twisters, read aloud, and speak more often. It’s also worth trying to pronounce words louder. Often, normal speech is restored within a few weeks;
- For a more reliable fixation of the prosthesis in the oral cavity, it is best to use special gels and ointments; they not only allow you to securely fix the product in the mouth, but also prevent the appearance of abrasion wounds and other mechanical damage to the oral cavity.
- It is necessary to completely exclude various sticky foods from the diet, and not only for the period of getting used to the prosthesis. These can be candies, various chocolate bars with nougat, toffees, etc.), they can not only cause discomfort during chewing, but also damage the structure.
Prosthetic stomatitis
Denture stomatitis is a consequence of the inflammatory process that develops in the gum tissue under the denture.
The cause of inflammation may be:
- improper fixation, excessive pressure of the structure on the gum, due to which blood circulation in the tissues is disrupted, bedsores appear, ulcers form, and the necrotic process begins
- diabetes;
- long-term use of steroids and some antibacterial drugs;
- low quality of oral hygiene.
In response to inflammation of the mucous membrane, the lymph nodes may become inflamed. The treatment program for prosthetic stomatitis will depend on its causes. If necessary, the installation of the prosthesis is corrected. As part of preventative treatment, proper, thorough hygiene is key. Additionally, the oral cavity can be sanitized with antiseptic drugs.
Temporomandibular joint dysfunction
One of the most unpleasant and dangerous complications after prosthetics is disturbances in the functioning of the temporomandibular joints. The dentofacial apparatus is a complex system in which each tooth, facial muscles and joints play a huge role. Any problem with teeth (displacement, loss of one/several teeth) increases the load on the chewing muscles, which leads to their rapid fatigue and the appearance of uncomfortable tension during chewing and when speaking. As a result, we have increased stress on the temporomandibular joints and joint dysfunction.
It is impossible not to notice pathological changes, since with joint dysfunction the patient develops characteristic symptoms: the jaw crunches near the ear when opening/closing the mouth, when chewing, the jaw hurts and movement restrictions appear (it is not possible to open the mouth wide or there is a restriction when moving the jaw in one direction). side). With ANS dysfunction, painful sensations are not limited only to the masticatory apparatus. Patients complain that half of their face and neck hurt, and they often have a headache. A person constantly feels tired.
Pathological processes in the ANS cause the development of other pathologies:
- bruxism (strong teeth clenching, teeth grinding during sleep);
- stoop (due to constant tension of the sternocleidomastoid muscles).
How to avoid temporomandibular joint dysfunction?
The most effective way to prevent dysfunction of the ANS is a thorough diagnosis at the stage of preparation for dental prosthetics. To identify problems in the dentofacial apparatus, a special study is carried out (the so-called “orthopedic diagnostics”), which makes it possible to analyze the relationship of the lower jaw to the upper, the correct occlusion of the teeth, and the work of the masticatory muscles when closing the jaw. Based on the impression, the movement of the patient’s lower jaw is reproduced in a special device (articulator). Such a study provides the specialist with information about the state of the entire dental system, allows for precise prosthetics taking into account the structural features of the jaws and dentition, and eliminates complications from the temporomandibular joint.
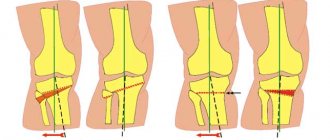
Incorrect (inappropriate) type of fixation
Installation of a hip and knee endoprosthesis involves fixation in one of 2 ways – cemented or cementless. The doctor must decide which option to use in a particular case, taking into account the patient’s gender, age, weight and lifestyle, diagnostic results (density and shape of the bone canal), and the characteristics of the prosthesis components.
At the same time, in practice, some decision-making rules have already been formed:
- cemented knee joint prosthesis is considered preferable for women and older patients (60 years and older), as well as people with severe symptoms of osteoporosis, wide channels and thinned walls of the femurs;
- installation of an endoprosthesis without cement is more often suitable for men and young people without severe forms of osteoporosis.
Errors in choosing the type of fixation
Choosing a cement method instead of a cementless one, and vice versa, can lead to serious complications. So, if a cemented installation is more suitable for a patient, and the elements of the implant were fixed without cement, the likelihood increases:
- crack formation;
- bone fractures (especially if it is the installation of a hip joint endoprosthesis );
- the need for reoperation.
When cementless fixation is required according to indications, and the implant is installed in a cemented composition, the patient will not simply require re-installation due to frequent dislocations or fractures. The revision operation will become significantly more complicated.
Errors when attaching components
An important point: even the correct method of fastening (cemented, cementless) does not eliminate the likelihood of complications associated directly with the process of installing a hip joint endoprosthesis, namely:
- insufficient amount of cement, which must be used to fill the acetabulum and femoral canal when installing a hip joint endoprosthesis using the cement method;
- uneven distribution of medical cement around the elements of the prosthesis (again, we are talking about a cement installation);
- incorrect choice of fixation site (orientation in the space of the bone bed). This error is possible with any method of fixation - cemented or cementless.
LEFT: Normal cement-metal interface (yellow arrow). However, there is weakening at the cementum-bone interface (orange curved arrow). RIGHT: Weakness at the cement-metal interface.
Galvanic syndrome
If metal is present in the denture structure, it is very important that all subsequent dental prostheses are made from this metal. The fact is that different metals have different electro-mechanical characteristics, which can lead to the occurrence of galvanic currents upon contact with an electrolyte (saliva plays the role of an electrolyte in the oral cavity).
Symptoms of galvanic syndrome:
- 1
the appearance of a sour or metallic taste in the mouth, a feeling of soreness;
- 2
changes in taste sensations (for example, a feeling of bitterness when eating sweets);
- 3
burning sensation on mucous tissue, tongue;
- 4
increased saliva viscosity, dryness;
- 5
pathological changes in mucous tissue - the appearance of swelling, redness, numbness;
- 6
sensation of electric current flowing in the gum tissue, along the teeth, tongue or in the palate;
- 7
hypersensitivity of the gums and tongue;
- 8
change in color of dentures (darkening).
Galvanic syndrome causes not only local discomfort in the oral cavity, but can also cause a general deterioration in the patient’s well-being.
Complications during the second stage of the operation
- Removing the intraosseous element of the implant along with the plug.
- Penetration of the implant into the maxillary sinus.
- Formation of a section of bone tissue over the intraosseous element.
The intraosseous element may become unscrewed if the process of reparative bone regeneration is disrupted and implant integration is lacking. In this case, the implant can simply be returned to its original place, the patient can be prescribed calcium supplements, and after a month and a half, the second stage of the operation can be repeated.
Cases of pushing the intraosseous part of the implant into the cavity of the maxillary sinus, as a rule, are the result of subantral implantation and a slowdown or disruption of the course of reparative bone regeneration. In this situation, surgery is required to remove the implant from the sinus cavity.
If bone tissue has formed over the intraosseous implant, this phenomenon is not considered a complication. You just need to make an incision in the periosteum and mucous membrane, remove the bone formation using a saw, and during the installation of the former and the gingival cuff of the implant, make sure that nothing else prevents their correct screwing.
Periodontitis (inflammation of the periodontal tissues)
The development of periodontitis after prosthetics is most often associated with improper formation of the stump for the prosthesis (without a ledge) and the wrong choice of orthopedic design. In this case, the gums acquire a bluish tint, begin to bleed, swell, and over time, recession of the gum tissue begins. This, in turn, leads to the exposure of the unaesthetic gray edge of the orthopedic structure, and can also have unpleasant consequences for the health of the tooth itself, since inflammation spreads to all periodontal tissues, leading to damage and atrophy of the jaw bone, and tooth loss.
Wrong choice of product size
The knee endoprosthesis, as well as the hip joint prosthesis, is now available in a wide range of sizes, shapes and leg widths. Thanks to this, the surgeon can choose the most suitable design for each case.
But choosing products by size is a very responsible, serious process. Mistakes made in it can lead to serious problems:
- when installing a small product, rapid loosening of the elements is likely;
- a design that is too large leads to bone fractures.
Often, a negligent approach and a negative result of treatment are explained not so much by the actions of the surgeon, but by the limitations of a particular clinic (when the patient is fitted with structures that are in stock at the medical center, so as not to delay surgical manipulation).
Peeling off the permanent structure
Artificial teeth are fixed using special dental cements. High-quality cement ensures reliable and stable fixation. However, there are cases when the crown begins to wobble, which indicates decementing or peeling off of the orthoconstruction.
Why is this happening?
- due to heavy loads on the prosthesis;
- due to improper preparation (grinding) of the tooth for a crown;
- if the supporting tooth has several small or one large filling (then the fillings are glued to cement and removed together with the crown);
- due to the large length of the bridge structure;
- if cement of poor quality or expired was used.
Chips in the lining of orthopedic structures
The outer layer of orthopedic products is made of ceramics. Thanks to the veneer, dentures and crowns look like real teeth – natural and aesthetically pleasing. The facing layer is quite durable, and subject to high-quality prosthetics and proper operation, orthopedic structures retain their original appearance and integrity for many years.
Chips of the aesthetic layer are possible for two reasons - errors at the planning stage, manufacturing of the orthopedic structure, and the patient’s violation of the ban on cracking nuts and gnawing bones.
In case of a chip, depending on the nature and size of the damage, you can correct the situation in two ways:
- 1
Replace the ortho construction.
- 2
Restore the facing layer without removing the prosthesis.
Different leg lengths after endoprosthetics
Changes in limb length after endoprosthetics are more often observed when a hip joint endoprosthesis is installed. As a rule, the leg in which the joint was replaced becomes longer, less often - shorter, than the second limb.
Reasons for changes in leg length:
- lack of radiological control during surgery;
- selection of an implant without preliminary collection of parameter measurements (offset, SDU). This error is typical for cases of installation of a knee joint endoprosthesis or hip replacement with cementless monoblock legs.
In some cases, a change in the length of the limbs can also occur with the correct installation of a knee endoprosthesis . A common reason is the lack of quality rehabilitation or its negligent implementation.
Measuring the lateral inclination of the acetabulum. The right minor trochanter is located lower than the left, indicating a leg length discrepancy. Normal horizontal center of rotation (red line).
Failure of bridge orthopedic structures
This problem can occur with temporary plastic and permanent stamped-soldered products due to intense stress. The main reason is technical errors at the stage of modeling and production of the prosthesis. As for stamped-soldered structures, today their failure occurs extremely rarely, since very durable materials are used in the manufacture of dentures.
If a temporary plastic prosthesis breaks, there will not be a big problem, since it can be quickly replaced.
Installation of low quality prosthesis
Initially, in the practice of endoprosthetics, low-quality products were used, which had a number of significant disadvantages. When installing them, repeated operations were required in 70–80% of cases after the first 2 years of use due to:
- periprosthetic infection;
- frequent dislocations;
- prosthesis fractures;
- instability of fixation of implant components;
- displacement of the head of the knee endoprosthesis or hip endoprosthesis;
- destruction of components (primarily the liner).
Today in Russia, knee endoprostheses have been replaced by analogues of a more advanced configuration made from modern materials of high reliability. They solved many problems. Although Russian practice has still not reached the level of prosthetics results in countries with developed medicine (Germany, Israel, USA). For effective surgical treatment, high-quality prosthetic structures are not enough. A set of clear, understandable standards for endoprosthetics and a revision of rehabilitation protocols are also required.
Individual intolerance
An allergy can be to both metal and plastic elements of the orthostructure.
If an allergic reaction occurs, patients complain of an unpleasant sensation in the mouth:
- the gums under the denture become sensitive and itchy;
- burning sensation under the crown;
- pain in the prosthetic bed;
- the appearance of dry mouth.
Moreover, sensitivity of the mucous membrane can occur both in the presence of signs of tissue inflammation, and in the complete absence of external symptoms of the inflammatory process. Allergic rashes around the mouth, difficulty breathing and other symptoms may appear.
Intolerance to materials used in the manufacture of dentures is a complication that is very rare in modern prosthetic dentistry. In case of individual intolerance, the best solution to the problem is to replace the denture with a product made of other materials that do not cause an allergic reaction in the patient.
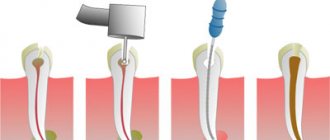
Complications during implantation
- Fracture of the pilot drill or bur.
- Damage to the bottom of the maxillary sinus or penetration of the drill into the nasal cavity.
- Violation of the integrity of the wall of the mandibular canal and damage to the inferior ventricular nerve.
- Damage by bur to the lower and lateral compact layers of the lower jaw.
- Partial or complete absence of primary fixation of the implant.
- Violation of the integrity of the wall of the alveolar process.
Damage to instruments can have various causes: excessive pressure on the fissure bur at the time of longitudinal drilling of the implant bed, violation of temperature conditions for sterilization of equipment, or the implant exhausting its service life in 30 sterilization cycles.
Damage to the floor of the maxillary sinus may be the result of an erroneous determination of the height of the alveolar process or excessive pressure on the instrument. If such a situation arises, you should refrain from installing the implant in this place and, if possible, install it in close proximity to the already formed bed. Another possible option is to install an implant, the length of the intraosseous part of which is two millimeters less than the depth of the finished bed. In this case, the bed must first be filled with bone chips or hydroxyapatite removed from the instrument. The recommended method of implantation in this case is a two-stage one, and it is better to choose a screw or combined intraosseous element.
Damage to the inferior ventricular nerve and injuries to the wall of the mandibular canal can be caused by negligence in preparing the bone bed or incorrect determination of the size of the implant due to possible distortion of the vertical size of the mandible on the orthopantomogram. If the preparation of the canal wall results in the occurrence of an intracanal hematoma and subsequent compression of the nerve, then restoration of sensitivity in the area of innervation can be expected in two to three weeks. In cases of osteoporosis, the wall of the mandibular canal may be defective or absent altogether; in this case, the effect on the lower ventricular nerve can be explained by hemorrhage in the area of the medullary spaces, as well as swelling of the reticular tissue of the bone marrow. Partial loss of sensation (or parasthesia) in the lower lip area may be felt the day after surgery and disappear completely after five to seven days. If the decrease in sensitivity of the lower lip, caused by a violation of the integrity of the wall of the mandibular canal and the inferior alveolar nerve, persists for one to two weeks, then the implant must be removed and the necessary symptomatic treatment performed.
Violation of the integrity of the lower or lateral compact layer of the lower jaw, by and large, is not a complication, but if during control radiographs it turns out that part of the implant extends beyond the jawbone by more than two millimeters, it is necessary to replace the installed implant with another one, whose height of the intraosseous part is less.
A fracture of the alveolar process wall very often occurs as a result of the installation of a plate implant if the bone bed under it was formed of a smaller size than necessary. Another possible reason for this complication is the narrowness of the alveolar process. In this case, you need to press the broken part to the appendage and stitch the wound.
If the implant in the bone bed is mobile and there is no fixation, the reason for this may be either improper preparation of the bone bed or osteoporosis. If the preparation of the bone bed was performed incorrectly, the installed implant can be replaced with a similar one, but of a slightly larger diameter (if this is allowed by the existing anatomical conditions), or the installed implant can be kept in the existing bed, filling the gaps in its upper part with bone chips. If the cause of implant mobility is osteoporosis, it can be fixed by filling the bed with osteoconductive or osteoinductive material. There is another option: replacing the existing implant with an implant of a different design, for example, a cylindrical one with a screw one, without cutting threads in the bed, which was prepared for installing a cylindrical implant.
What are the reasons for complications during prosthetics?
Most complications can be prevented even at the stage of preparation for prosthetics if you know the main causes of these problems.
We invite you to understand the reasons why complications arise after prosthetics:
- Insufficient preparation – if before the prosthetic procedure the patient refused to carry out the necessary treatment, therapeutic and preventive, hygienic procedures (caries treatment, professional hygiene).
- Error in size. If an error was made in the manufacture or selection of the type of orthopedic structure or prosthesis, wearing it will cause discomfort to the patient.
- Unprofessional, poor-quality installation of orthopedic structures. In this case, the patient may encounter various problems - from the accumulation of food debris in the elements of the prosthesis to the development of inflammatory processes in the oral cavity, or breakdown of the prosthesis itself.
- Allergy, the body's immune reaction to denture materials.
- Mobility, displacement of teeth - leads to displacement of the denture structure.
- Poor quality of oral hygiene after installation of a denture.
Solution
Errors in dental prosthetics usually occur due to improper work of the dentist. Any neglect of the necessary procedures preceding the actual prosthetics leads to irreversible complications. It will be impossible to correct/correct anything - you will have to remove the prosthesis (even permanent crowns and onlays), prescribe full treatment for the problem, and then repeat the prosthetic procedure again.
The dentist should never make concessions to patients - they often ask to install a prosthesis for carious teeth, not to pay attention to swelling of the gums (and this is a sign of inflammation), to choose the most expensive crowns. Such rashness has no place - the doctor must explain the situation to the patient in detail and inform the patient about the possible consequences. And patients themselves should be guided by the recommendations of professionals - this will be the key to obtaining the desired effect.
Oral hygiene after dentures
To maintain a healthy and beautiful smile, it is not enough to simply insert a tooth. You also need to take care of careful care of the oral cavity and the dentures themselves. Hygiene is the basis of dental health. After installing a denture, hygiene requirements increase, since food particles can get stuck in the elements of the orthopedic structure, plaque accumulates on the walls of the denture, and thus creates a favorable environment for bacteria - the main culprits of all diseases of the teeth and gums.
Care of fixed dentures:
- 1
regular brushing of teeth (recommended not only in the morning and evening, but also after each meal);
- 2
rinsing with special antiseptic preparations;
- 3
professional dental cleaning every 3 months.
Care will become much easier if you purchase an irrigator - a device that effectively washes away food debris in the most inaccessible areas of the oral cavity and is completely safe for dentures.
Rules for caring for removable dentures:
- after each full meal or snack, the denture should be removed and washed under running warm water;
- In the morning and evening, dentures, just like teeth, need to be cleaned (for this, use a toothbrush with soft bristles and a special paste for dentures);
- in order to prevent the accumulation of plaque, it is recommended to soak the denture in a special solution for 10-20 minutes after each cleaning;
- From time to time it is necessary to take your dentures to the dentist for cleaning;
- Removable orthopedic structures should be stored in clean water or a special solution for storing prostheses.
New generation removable dentures, made of high-quality polymers, are so comfortable that they can be left on at night.