Tonsillectomy for most patients with chronic decompensated tonsillitis is the method of choice and often the only treatment. In this regard, tonsillectomy is one of the most common planned operations in ENT surgical practice. This method of surgical treatment, according to various authors, reaches up to 40% of all surgical interventions on the ENT organs [1-3]. Indications for surgical intervention are frequent tonsillitis, as well as local complications of tonsillitis, such as peritonsillar abscess, retropharyngeal abscess, neck phlegmon, suppurating cervical lymphadenitis, febrile convulsions, severe tonsillogenic intoxication, diseases of distant organs and systems associated with pharyngeal pathology [4]. In the postoperative period after tonsillectomy, pain remains extremely relevant and in most cases the only symptom. The causes of pain immediately after tonsillectomy and in the next few days are the extensive open postoperative surface in the tonsillar niches, swelling and infiltration of the palatal arches [5]. The mechanism of post-traumatic pain is associated with an increase in the excitability of nociceptors resulting from the action of algogens - substances released from cells damaged as a result of surgical exposure (histamine, serotonin, ATP, leukotrienes, interleukin-1, tumor necrosis factor, endothelins, prostaglandins, nitric oxide, neurokinin , A, etc.) and formed in the blood plasma (bradykinin). Most often after surgery, patients are bothered by severe sore throat, which often radiates to the ears and also intensifies when swallowing [6]. In these cases, it is necessary to resort to painkillers, as well as follow a special diet that excludes coarse, salty, and spicy foods. Postoperative pain negatively affects the patient's eating and return to active daily life.
In addition, there is a danger of microbial contamination of the wound surface against the background of a decrease in local immunity and anti-infective resistance of inflamed tissues. In this regard, an important problem after tonsillectomy is to reduce the phenomena of reactive inflammation of tissues and reduce the pain syndrome that occurs in response to surgical trauma.
To achieve optimal analgesic effect after tonsillectomy, the use of a large number of different analgesic drugs is required.
According to the literature, over the years of tonsillectomy, multiple attempts have been made to improve pain relief in the postoperative period, both with systemic and local drugs. However, many of them have side effects and are poorly applicable in modern practice.
Opioid use has side effects such as nausea, vomiting, constipation, respiratory depression and severe sedation.
Nonsteroidal anti-inflammatory drugs (NSAIDs) increase the risks of bleeding and gastrointestinal disorders. According to experts, ibuprofen has some advantages in terms of tolerability over other non-steroidal anti-inflammatory drugs [7]. Cyclooxygenase-2 inhibitors (celecoxib) have similar analgesic properties to nonselective NSAIDs and have minimal side effects such as platelet dysfunction and gastrointestinal bleeding. However, one study showed that celecoxib does not provide sufficient analgesic effect after tonsillectomy and also often causes vomiting [8].
H. Tolska et al. [9] conducted a meta-analysis of 29 studies representing a double-blind, placebo-controlled, randomized trial of systemic analgesics used in the postoperative period after tonsillectomy. This study confirmed the beneficial analgesic effects of paracetamol, NSAIDs, dexamethasone, gabapentinoids and dextromethorphan after tonsillectomy on the day of surgery. Dexamethasone in multiple doses had an analgesic effect exceeding 24 hours. However, the use of steroids with high total doses and/or long-term use after surgery should be carried out with caution, taking into account the possible risks. Well-known side effects of systemic corticosteroid therapy (eg, moon face, Cushing's syndrome, diabetes mellitus) develop with long-term treatment. The risk of side effects from short-term, 1-2 weeks, systemic glucocorticosteroid therapy is minimal if treatment is not given to patients with diabetes, glaucoma, cataracts and osteoporosis. However, an increase in blood glucose levels and a rise in blood pressure can be observed during treatment with systemic glucocorticosteroids and in patients without diabetes mellitus or hypertension. A single dose of analgesics or the use of dexamethasone alone does not provide a clinically significant long-term analgesic effect after tonsillectomy.
A. Khan et al. found that gabapentin, pregabalin, and dextromethorphan may be useful in moderate doses as adjuvants to other analgesics. However, gabapentin and pregabalin are antiepileptic drugs, and dextromethorphan is an antitussive drug, and therefore their analgesic effect itself is not justified. Ketamine, an NMDA antagonist used as an anesthetic, can be used for pain relief after surgery. Its use in subanesthetic doses is effective in various types of surgeries to reduce opioid requirements and pain sensitivity. However, a patient receiving ketamine should be under constant medical supervision [10].
Thus, systemic analgesic drugs do not always have a good analgesic effect and in most cases have side effects. In this regard, in order to avoid the systemic effect of NSAIDs and at the same time ensure direct contact of the drug with the mucous membrane of the oral cavity and pharynx, it was necessary to develop local anesthetic drugs.
Topical drugs used in the complex treatment of pathological conditions of the oral cavity and pharynx can be divided into analgesics, anti-inflammatory drugs, antiseptics, drugs with a decongestant effect on the mucous membrane, etc. [11]. Local preparations in the form of lozenges, sprays, and rinses have also begun to be used in patients after tonsillectomy.
Many studies conducted in adult patients after tonsillectomy have shown the therapeutic effectiveness of benzydamine, especially when using a 0.15% mouthwash or spray - rapid relief of sore throat, reflex otalgia, and the absence of secondary bacterial complications were noted. However, in these studies there is mention of such an unpleasant sensation in some patients as a burning sensation in the throat associated with the ethyl alcohol contained in these drugs. This may indicate the irritating effect of these drugs, as well as the risk of bleeding from the tonsil niches [12, 13]. Topical therapy for the oropharynx may include rinsing, spraying, and lozenges. Rinsing with medicinal preparations is effective in treating the oral cavity and the base of the tongue. The use of a spray allows you to irrigate the back wall of the pharynx, however, the use of sprays is not recommended for children under 6 years of age and for patients with bronchial asthma. When assessing the effectiveness of medications in the form of resorption, it was noted that the concentration of active ingredients in the pharyngeal mucosa is higher than when using a spray and rinse. There is also a slower cleansing of the pharyngeal mucosa from drugs when using drugs in a resorption form, which ensures the maintenance of a high concentration of the drug at the site of inflammation [14].
In the search for non-pharmacological analgesia, various types of non-traditional approaches to pain management are being used. One such approach is transcranial electrical stimulation. It has been established that under the influence of this method the sensitivity of peripheral pain receptors decreases. This effect is caused by an increased concentration of β-endorphin circulating in the blood. However, this method has a number of contraindications and reduces the severity of pain for a limited period of time, and it is also economically unprofitable [15].
The use of a visual analogue scale (VAS) to assess pain allows us to assess the level of acute postoperative pain syndrome in patients who have undergone tonsillectomy [16].
In connection with the problem of pain relief for patients in the postoperative period after tonsillectomy, attempts have been made in recent years to produce new, safe, modern drugs. One of these drugs is Arnica Montana C9 (BOIRON) - a homeopathic monocomponent drug of plant origin.
The purpose of the study was to identify the effect of the homeopathic monocomponent herbal preparation Arnica Montana C9 (BOIRON) on the condition of patients who underwent tonsillectomy.
What causes inflammation of the tonsils (tonsillitis)
The tonsils (tonsils) become inflamed when their lymphoid tissue, which is involved in the formation of immunity, is unable to cope with the infectious agent. In this case, adults and children develop acute tonsillitis (tonsillitis), which can develop into chronic.
Other causes of chronic tonsillitis include [2]:
- frequent and untreated pharyngitis;
- prolonged difficulty in nasal breathing due to curvature of the nasal septum, infectious diseases of the nasal mucosa and paranasal sinuses (rhinitis, sinusitis, the occurrence of polyps, etc.);
- diseases of teeth and gums;
- allergic reactions.
As a result of tonsillitis, inflamed tonsils turn into a source of infection, which leads to decreased immunity and frequent respiratory diseases and can cause complications of existing chronic diseases, the development of allergies and serious diseases of the cardiovascular system, liver, kidneys, and joints [2].
Symptoms of chronic tonsillitis
The main symptoms of the disease include [2]:
- elevated temperature for a long time, especially in the evening;
- headache, sore throat and joint pain;
- loss of appetite;
- bad breath;
- inflammation of the cervical and submandibular lymph nodes;
- frequent relapses of sore throat.
When examining the throat, the ENT will find [2]:
- enlargement, looseness, swelling of the tonsils;
- accumulation of plugs (white cheesy mass) in the lacunae of the tonsils.
Indications for tonsillectomy
After collecting anamnesis and a complete examination, the doctor will prescribe a tonsillectomy if there is [1, 2]:
- frequent relapses of tonsillitis (if we talk about children - from seven exacerbations per year to five or three exacerbations over two and three years, respectively), convincing of the ineffectiveness of conservative treatment;
- decompensated form of chronic tonsillitis, when the tonsils are unable to perform their protective functions and inflammation leads to diseases of other organs;
- chronic tonsillitis with toxic-allergic phenomena, when the risk of complications and other infectious-allergic diseases increases;
- sleep apnea syndrome, when inflamed tonsils cause dysfunction of breathing and swallowing;
- purulent complications in the tonsils themselves and peritonsil tissue;
- Marshall syndrome (PFAFA syndrome) is a regularly recurring fever with complications that occurs mainly in children.
Diagnostics
The need for tonsillectomy is determined by an ENT doctor after a conversation with the patient, a visual and instrumental examination, and obtaining the results of diagnostic studies. Laboratory tests and instrumental examinations not only indicate the presence of chronic tonsillitis, but also reflect the degree of influence of the inflammatory process on the body. Some of the tests and examinations are necessary to ensure that there are no contraindications to surgery.
Before removing tonsils, the following is prescribed:
- general blood test with leukocyte formula;
- blood chemistry;
- blood clotting test;
- blood for syphilis, HIV, hepatitis;
- rheumatic tests;
- general urine analysis;
- ECG;
- FLG;
- culture from tonsils.
Contraindications to tonsil removal
The operation is impossible if the patient [1, 2, 3]:
- diseases of the blood system that occur with increased bleeding (hemophilia, agranulocytosis, leukemia, leukemia, hemorrhagic diathesis and others);
- vascular anomalies of the pharynx (angiodysplasia, aneurysms, submucosal pulsation of the vessel);
- active form of tuberculosis;
- decompensated form of diabetes mellitus;
- severe progressive diseases of the cardiovascular system, kidneys, liver, lungs;
- severe forms of mental disorders.
There are also relative contraindications that can negatively affect the outcome of the operation - therefore, tonsillectomy should be postponed until they are eliminated or completed [1, 2, 3]:
- acute infectious diseases;
- menstruation;
- caries;
- inflammation of the gums;
- pyoderma (pustular skin diseases);
- exacerbation of chronic diseases;
- exacerbation of dermatitis;
- pregnancy starting from the 7th month.
Anesthesia
Tonsillectomy surgery is performed under both local anesthesia and general anesthesia (anesthesia). Both methods of pain relief have their advantages and disadvantages, so the decision is made by the attending doctor, taking into account the health condition and wishes of the patient.
Local anesthesia
The classic surgical technique (under local anesthesia) has been carried out for many decades and has not lost its relevance today. An anesthetic solution in an amount of about 20 ml is injected into several points around the tonsil - usually 1% lidocaine with the addition of adrenaline (to reduce bleeding). The effect is that the tissues are deeply impregnated with the drug, so the pain is almost not felt, and the tonsil appears to be raised above the palatine arches and is easy to isolate. This technique is called infiltration anesthesia.
If the patient has had allergic reactions to these drugs, they are replaced with ultracaine. Next, the operating doctor proceeds directly to removing the tonsils. The patient is only required to strictly follow his instructions. A tonsillectomy lasts about half an hour; before sending the patient into the room, the surgeon carefully checks whether the bleeding has stopped. This is a very important moment of the operation.
General anesthesia (anesthesia)
Nowadays, tonsillectomy is performed more and more often under general anesthesia. This is due to the fact that anesthetic equipment and drugs for anesthesia have changed a lot recently. Modern anesthetics are considered to be of a high safety class; they are non-toxic and do not carry the same complications as before. Anesthesia is easily tolerated by the patient and feels similar to normal sleep.
The photo shows an anesthesia device from the German company Drager used in the clinic.
To carry out general anesthesia, the patient is carefully examined, before the operation he is examined by an anesthesiologist, because, despite the safety of anesthesia, if there are deviations in the tests, the operation may be postponed. The operation is performed strictly on an empty stomach; the patient cannot even drink water. After the examination, the patient is escorted to the operating room, where he is placed on the operating table and put on a breathing mask. A mixture of oxygen and anesthesia medication is supplied to it, sleep occurs within a few minutes, and the operation ends for the patient - awakening occurs in the ward.
Doctors anesthesiologists
The clinic employs highly qualified anesthesiologists with many years of experience, including specialists from the Children's Clinical Hospital named after. N.F. Filatov, who have academic degrees of candidates and doctors of medical sciences, many years of unique work experience. Our specialists use a modern anesthesia device from the German company Drager and the latest generation of medications. All this allows operations to be performed under general anesthesia (anesthesia), which is safe for the patient’s health, with further rapid recovery in the postoperative period.
Drugs used
In their work, anesthesiologists use modern drugs such as sevoran, diprivan, esmeron, enfluron, isoflurane, dormicum and others. The use of a specific drug is at the discretion of the anesthesiologist and depends on each individual case, test results and other factors.
Preparing for surgery
The decision to remove the palatine tonsils, as well as the choice of treatment tactics and anesthesia, is made by the otolaryngologist after collecting anamnestic data and conducting a thorough clinical examination [2]:
- taking tests (general blood and urine analysis, biochemical blood test, determination of blood group and Rh, coagulogram (assessment of blood clotting), etc.);
- other examinations (electrocardiography, fluorography, etc.);
- in the presence of pathologies, consultation with specialized specialists and additional examinations;
- prescribing medications that reduce the risk of bleeding, and, if necessary, other drug therapy and taking sedatives.
This treatment method has been used for more than 2000 years and remains one of the most common surgical interventions to this day.
During the time that has passed since the first tonsillectomy in children, surgical tactics, pre- and postoperative preparation of the patient, as well as the possibilities of pain relief have changed significantly. Polunina T. A, Ph.D., ENT, employee of the Scientific Center for Children's Health of the Russian Academy of Medical Sciences, Moscow [1]
A few days before surgery, you must give up alcohol, smoking, and eating heavy, spicy, and fatty foods. You should not eat or drink directly on the day of surgery.
Conclusion
Based on the statistical analysis of the comparison of two groups of patients who underwent bilateral tonsillectomy, in patients who received, in addition to the anesthetic drug ketorolac, Arnica Montana C9 (BUARON) for resorption, 5 granules 3 times a day from the 2nd day, the recovery time was significantly reduced . This is indicated, in particular, by a faster time for normalization of body temperature, disappearance of pain and a decrease in the inflammatory reaction in the pharynx after tonsillectomy. This may have a positive effect on the quality of life in the early postoperative period of patients taking the drug Arnica Montana C9 (BOIRON).
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Surgical options
Today there are many methods for removing tonsils, but the most common include [1, 3]:
- Classic (standard) tonsillectomy. Enucleation of tonsils using surgical instruments.
- Extracapsular tonsillectomy. The doctor, using scissors and a loop, cuts off the palatine tonsil along with the capsule, then applies sutures. The main disadvantage of this method is the high risk of bleeding both during and after surgery.
- Using an ultrasonic scalpel. Thanks to high-frequency sound vibrations, the temperature of surrounding tissues remains low enough to avoid serious damage.
- Coblation (bipolar radiofrequency ablation). This method has become widespread in otorhinolaryngology due to the minimization of pain and postoperative risks, as well as the reduction of the recovery period. This is due to the absence of thermal effects: the radiofrequency energy used separates the molecular bonds between tissues, allowing them to be cut almost painlessly and bloodlessly.
Possible complications after tonsil removal
Thorough preoperative examination and preparation, modern equipment and adherence to doctor's recommendations during rehabilitation after tonsil removal can minimize the risk of complications after tonsillectomy. However, the following cannot be excluded [2]:
- bleeding, which can occur both directly during surgery (primary) and several hours and days after tonsillectomy (secondary);
- sore throat, difficulty swallowing;
- taste disturbance;
- inflammation of the wound;
- increased body temperature;
- swelling of the soft tissues of the neck and larynx.
Therefore, the first few days after removal of the tonsils, the patient most often remains in a hospital under the supervision of specialists, where if his health worsens, he will be provided with qualified assistance.
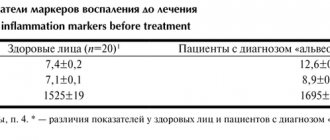
Material and methods
The study was carried out in patients with chronic decompensated tonsillitis who were admitted to the Department of Otorhinolaryngology of the St. Petersburg State Medical University named after. acad. I.P. Pavlova for planned surgical treatment. Group 1 included 23 patients aged from 20 to 43 years, who in the postoperative period received NSAIDs (Ketorolac) on demand for pain, as well as a homeopathic monocomponent herbal preparation Arnica Montana C9 (BOIRON) 5 granules 3 times a day for resorption from the 2nd day. The second (control) group of patients included 20 patients aged 19 to 42 years who received only on-demand NSAID therapy (Fig. 1).
Rice. 1. Distribution of patients in groups by age. The two study groups of patients were balanced by gender and age, thus, the studied differences between them reflect the effect of the drug Arnica Montana C9 (BOIRON). All patients underwent classical bilateral tonsillectomy under general anesthesia by the same operating team. In the early postoperative period, a number of criteria were assessed in all patients: body temperature in the morning after waking up and in the evening, the need to use NSAIDs, the amount of their use per day, pain assessment according to VAS, as well as changes in the pharyngoscopic picture and neck lymphadenopathy within 10 days after surgery.
The results of the study were entered into the developed computer database on a personal computer using Microsoft Excel tables. Using the application package Statistica for Windows v.10.0, analysis and statistical processing of the obtained data were carried out, and the parameters of descriptive statistics were determined.
Quantitative indicators were checked for compliance with normal distribution using the Kolmogorov-Smirnov test. For quantitative data having a normal distribution, the arithmetic mean ( M
) and standard deviation (
SD
), which are presented in the format
M
(
SD
); when describing indicators that differ from the normal distribution, medians (Me) were used in the Me format (Q1; Q3) and the lower Q1 (25%) and upper Q3 (75%) quartiles were used as an interval estimate. Qualitative indicators of the study are presented in absolute and relative values (%).
To find differences between normally distributed indicators, t
-Student's t-test.
Formula t
-Student's test:
where M
1 - arithmetic mean of the 1st compared group,
M
2 - arithmetic mean of the 2nd compared group,
m
1 - mean error of the first arithmetic mean,
m2
- mean error of the second arithmetic mean.
Statistical processing of the study results in groups was carried out with determination of significance using the nonparametric Mann-Whitney U test.
Mann-Whitney U test formula:
where n
1 - the number of elements in the 1st sample,
n
2 - the number of elements in the 2nd sample, T
x
- the larger of the 2 rank sums,
nx
- the corresponding sample.
Indicators changing over time were analyzed using paired Student's t test (in the case of normal distribution) or using t
-Wilcoxon test.
To analyze qualitative indicators, the χ2 test with Yates' correction was used (in cases of absolute numbers less than 10); if it was impossible to use it, the Z-test was used for proportions with correction for end points.
The difference between groups was considered statistically significant at p
<0,05.
Postoperative period after tonsillectomy
The duration of the recovery period after tonsillectomy directly depends on the chosen method of operation; the wound itself heals on average in 3–4 weeks. For rehabilitation to be successful, it is necessary [2]:
- follow all doctor's recommendations;
- stick to bed rest for the first few days;
- limit physical activity, visiting the sauna, hot bath, swimming pool;
- take prescribed medications;
- for the first 5–7 days, avoid eating irritating foods (hot, cold, sour, spicy), carbonated drinks;
- Carefully monitor your condition and, if any deviations or complications appear, seek the help of specialists.
After surgery to remove the tonsils as a source of infection, the frequency of colds and the risk of developing serious complications are reduced. Therefore, if conservative methods of treating tonsillitis do not produce results, it is necessary to contact a specialist and discuss the possibility of surgery.
Advantages of the laser method
The laser method is one of the most modern methods of treating tonsils.
- Coagulation of the tonsils that occurs during laser exposure accelerates healing, thereby reducing the possibility of bleeding.
- The duration of the laser operation is up to 30-40 minutes.
- Laser treatment does not leave open wound surfaces.
- Laser tonsillectomy surgery is performed on an outpatient basis and does not require a long recovery period. The patient remains able to work after the operation.
- The operation is performed using local anesthesia
- To minimize trauma and facilitate the recovery period, laser tonsillectomy is usually performed in several stages.
Laser exposure is sterile in nature, it allows you to reduce the risks of negative consequences of the operation and minimize interference in the body using the partial excision method.