The most common dental disease in the world, according to statistics, is dental caries. Depending on the part of the tooth that is affected by the carious process, it is divided into different types. Most patients visit the dentist for dentin caries. What are the features of this form of the disease and how it is treated, we will tell you in the article.
In this article
- Tooth structure and types of carious lesions
- Dental caries and its features
- How does a tooth hurt with dentin caries?
- Isolated dentin caries: what are its features
- Basic diagnostic methods
- How is dentin caries treated?
- Prevention of dentine caries in permanent and baby teeth
Tooth structure and types of carious lesions
A tooth consists of several parts. On top it is covered with hard mineralized enamel, underneath there is dentin, and even deeper - the root of the tooth and pulp. Caries is a pathological process that is accompanied by demineralization and softening of hard dental tissues with the subsequent formation of a carious cavity. The process can affect any part of the tooth; depending on this, caries of enamel, dentin or cement is distinguished.
Carious lesions of the enamel are characterized by symptoms such as softening, the appearance of a white or brown spot, roughness, and sometimes the carious cavity is located in the enamel. If the lesion affects the bone tissue of the tooth, which makes up its bulk, in this case we speak of dentin caries. This form of lesion is characterized by the formation of a carious cavity directly in the dentin.
Cement caries affects the root of the tooth and contributes to its exposure. It often occurs with gum disease, when there is no close contact between the tooth and the gum.
Text of the book “Fundamentals of clinical dental morphology: a textbook”
Chapter 5 Histology of teeth and surrounding tissues
5.1. Hard tooth tissues
5.1.1. Dentin Dentin (dentinum) is
the tissue that forms the bulk of the tooth and determines its shape. In humans, dentin in the crown area is covered with enamel, and in the root area - with cement. Thus, in a healthy tooth, dentin does not come into contact anywhere with the external environment and tissues surrounding the tooth. Like enamel, mature dentin is another ossified tissue of the tooth. In terms of its formation, structure and physiological characteristics, dentin is most likely closer to compact coarse-fibrous bone tissue, but differs from it in greater hardness and the absence of cells. Dentin and bone share some similar properties:
– growth by accession (apposition);
– the presence of a canalicular system containing cell processes, as well as specialized extracellular fluid and mineralizing matrix vesicles;
– structure of an organic matrix of collagens. However, between these two tissues there are obvious differences
differences.
Main features of dentin:
– dentin comes from ectomesenchyme (cells of the cranial part of the neural crest);
– dentin is restored and modified throughout the life of the individual;
– dentin is an acellular tissue (contains only processes of odontoblasts) that does not have blood vessels;
– odontoblasts participate in both the formation and mineralization of the organic basis of dentin.
Physical properties and chemical composition.
Dentin has a light yellow color, has some elasticity, it is stronger than bone and cement, but 4–5 times softer than enamel. The high hardness of dentin is explained by the presence in it of a large amount of mineral salts, the content of which reaches 70-80%, while the remaining 20-30% consists of organic substances (12-18%) and water (8-12%). In this regard, organic and inorganic components (matrices) are distinguished in mature dentin.
Organic matrix
Dentin is made up of collagen. Under an electron microscope, rather large fibers with an axial periodicity of 600–700 nm, characteristic of type 1 collagen, are visible. this is a genetically specific form of collagen found in the most ossified tissues (dentin, bone, cement).
In dentin, collagen fibers are oriented randomly, as in dense, unformed connective tissue. Only at the dentinoenamel border - in mantle dentin - are the fibers characterized by regularity, precise organization and orientation.
The collagen fibers of the dentin matrix are embedded in a basic amorphous substance consisting of glycosaminoglycans such as chondroitin sulfates. The latter can combine with non-collagen proteins, resulting in the formation of proteoglycans - the main components of the dentin matrix.
About 20% of the organic dentin matrix consists of non-collagen proteins, which play a role in the mineralization of dentin:
– proteins rich in gamma-carboxyglutamic acid;
– proteins that bind calcium;
– bone morphogenetic proteins;
– glycoproteins: fibronectin, osteonectin and, possibly, dentinonectin;
– proteins associated with membranes: calcium ATPase and alkaline phosphatase;
– collagenases, as well as collagen-digesting enzymes, necessary for the restructuring and change of the organic matrix.
In the organic basis of dentin, lipids (glycolipids and phospholipids) have also been identified, probably participating in the mineralization of the matrix.
Inorganic matrix
Dentin, like bone, cement and enamel, consists mainly of calcium phosphate in the form of hydroxyapatite crystals, which in dentin are small, thin, needle-shaped.
Transmission electron microscopy data made it possible to establish that these crystals are located both inside collagen fibers and between them. The inorganic dentin matrix contains small amounts of calcium fluoride (fluorapatite), calcium carbonate, magnesium and sodium.
5.1.1.1. Structure of dentin
Dentin consists of a ground substance and many thin dentinal tubules (canaliculi dentales) that penetrate the ground substance (Fig. 89).
Rice. 89. Scheme of the structure of dentin and periodontium (according to R. Krstic).
1 – Toms fibers; 2 – odontoblasts; 3 – predentin; 4 – dentin; 5 – cellular cement; 6 – acellular cement; 7 – fibers of the periodontal ligament; 8 – periodontal blood vessels; 9 – bone alveolus; 10—Thoms granular layer (interglobular dentin); 11 – alveologingival ligaments; 12 – gums; 13 – enamel; 14 – gingival epithelium.
Dentinal tubules provide trophism to dentin and are thin cone-shaped tubes with a diameter of 1 to 3–4 μm, running in the radial direction from the dental pulp to the enamel or cement. They are wider in the inner parts of the dentin and gradually narrow outward.
The number of dentinal tubules varies in different parts of dentin. Due to the radial direction in relation to the tooth cavity, the tubules in the internal parts of the dentin (near the pulp) lie more closely: there are 50,000-75,000 dentinal tubules per 1 mm2 of dentin, and from 15,000 to 30,000 tubules closer to the periphery. There are more of them in the crown of the tooth than in the root. In molars there are 1.5 times less of them per 1 mm2 of dentin surface than in incisors.
The dentinal tubules in the crown are S-shaped curved, and in the area of the tooth root they are almost straight and run perpendicular to the axis of the tooth.
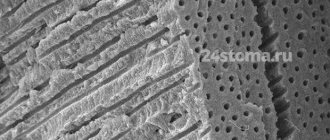
In the thickness of the dentin, the tubules branch and give off lateral processes that anastomose with each other (Fig. 90).
Rice. 90. Topography of dentinal tubules in peripulpar dentin (scanogram)
1 – dentinal tubules; 2 – Toms fibers; 3 – collagen fibers of the organic dentin matrix; 4 – boundary plate (Neumann’s shell).
The branching of the tubules is especially clearly visible at the dentinoenamel and dentinocement border, where each of them is divided into several terminal branches. In some cases, the tubules can cross the dentinoenamel border, penetrating into the thickness of the enamel and forming enamel spindles.
Due to the presence of a huge number of tubes penetrating dentin, the latter has high permeability. This circumstance is of clinical significance, causing a rapid response of the pulp to damage to dentin.
The ground substance surrounding the tubules is more compacted (hypermineralized) and homogeneous than the substance in the spaces between them. In this regard, peritubular (around the tubular) and intertubular (intertubular) dentin are distinguished.
Peritubular dentin is the layer of dentin that immediately surrounds each dentinal tubule, forming its wall (Fig. 91).
Rice. 91. Electronic scanogram of a dentin area.
1 – openings of dentinal tubules; 2 – peritubular dentin; 3 – intertubular dentin.
The thickness of the layer of peritubular dentin at the pulp end of the tube is about 40–50 nm, and at the dentinoenamel border – 500–700 nm. This dentin has a higher (35–40%) mineral content than intertubular dentin. The amount of organic matter in peritubular dentin is minimal, since it almost completely disappears during decalcification. Therefore, during caries during dentin demineralization, peritubular dentin undergoes intense destruction, which leads to the expansion of the tubes and an increase in its permeability.
During tooth development, intertubular dentin is formed first in both mantle and peripulpal dentin. It consists mainly of calcified collagen fibrils with a diameter of 100–200 nm, with hydroxyapatite crystals located along the axis of the fibrils.
The contents of dentinal tubules are varied:
– processes of odontoblasts (Toms fibers);
– unmyelinated nerve fibers;
– tissue dentinal fluid;
– non-calcified collagen fibrils (intertubular fibrils);
– hydroxyapatite crystals.
Some of these substances are involved in the sensory function of dentin, others are involved in the restructuring of its organic matrix. From the inside, the wall of the dentinal tubule is lined with a thin film of organic matter - the boundary plate (Neumann's membrane, or membrane), running along the entire length of the dentinal tubule and containing high concentrations of glycosaminoglycans. The tubes can serve as conductors for various substances necessary for dentin restoration, cellular debris from degenerated odontoblasts, microorganisms and their metabolic products. The latter can reach the pulp, causing some damage to it.
The processes of odontoblasts, being a direct continuation of the apical sections of their cell bodies, as a rule, stretch along the entire length of the dentinal tubules, ending at the dentinoenamel border. They contain few organelles, but a significant number of cytoskeletal elements, as well as vesicles, lysosomes and polymorphic vacuoles. The lateral branches of the processes are numerous in the predentin and internal parts of the dentin (100–200 µm from the border with the pulp), there are few of them in its middle parts and again many at the periphery. The branches form contacts with branches of neighboring odontoblasts, which can play a significant role in the transfer of nutrients and ions, as well as contribute to the spread of microorganisms and acids during caries.
Nerve fibers directed into dentin from the peripheral parts of the pulp usually penetrate into it to a depth of several micrometers, individual fibers - to 100–200 microns. Some of the fibers already in the predentin are divided into numerous branches; others pass inside the dentinal tubules along the process of the odontoblast or have a spiral course, entwining it and occasionally forming branches running at right angles to the tubules. Nerve fibers are usually thinner than the processes of odontoblasts and in some places form connections with them such as tight junctions and gap junctions. Most researchers believe that nerve fibers in the dentinal tubules influence the efficiency of odontoblast activity, that is, they are efferent, and do not perceive changes in their environment.
The main substance of dentin, located between the dentinal tubules, has a fibrillar structure and consists of collagen fibers and a homogeneous cementing substance (Fig. 9 2).
Rice. 92. Electronic scanogram of a demineralized area of peripulpar dentin.
1 – collagen fibers of the organic matrix; 2 – openings of dentinal tubules.
The location of collagen fibers and their structure change in different parts of dentin. In this regard, two layers of dentin are distinguished: outer, or mantle (mantle) dentin and inner, or peripulpal dentin. In mantle dentin, the predominant fibers are those running in the radial direction (Korff fibers), parallel to the course of the tubules. this arrangement remains closer to the occlusal surface of the tooth crown, and on the lateral surfaces of the crown and in the root area the radial fibers acquire an increasingly oblique direction.
Mantle dentin smoothly transitions into peripulpal dentin, in which, along with radial fibers, there are a large number of fibers located parallel to the surface of the pulp. The mantle dentin matrix is less mineralized than the peripulpal dentin matrix and contains relatively fewer collagen fibers.
In peripulpar dentin, the fibers are located tangentially (Ebner fibers) and almost at right angles to the dentinal tubules.
The location of Ebner fibers in the peripulpal dentin coincides with the location of the dentinal plates - layers of dentin deposited from the inside, from the pulp side, during the development of the tooth. The expression of rhythmic growth and layered dentin deposition are Owen's contour lines and Ebner's growth lines.
Owen's lines usually run at right angles to the dentinal tubules and correspond to periods of rest in the activity of odontoblasts. During this period, less intense calcification of the dentin substance and the formation of very small interglobular spaces occurs (Fig. 93).
In baby teeth and first permanent molars, a contour (neonatal) line is often visible, separating the layer of dentin that formed during the prenatal period of life from the dentin that formed after birth. According to B. Orban [72, 73], this line corresponds to incompletely calcified dentin that arose in the first 2 weeks after birth due to metabolic disorders during the period of adaptation of the newborn to sudden changes in environment and nutrition.
The number of Owen lines can increase in pathological conditions of the body (long-term illnesses accompanied by increased body temperature, unstable nutrition, etc.).
Rice. 93. Microphotograph of a longitudinal section of a tooth (from L.I. Falin).
1 – Owen lines; 2 – dentinal tubules.
The thinner Ebner lines, directed almost perpendicular to the dentinal tubules, are located closer together than the Owen lines, with a periodicity in the crown of about 18–20 μm. Between Ebner's lines there are lines, the distance between which is usually constant (about 4–5 µm) depending on the location - at the apex or at the root of the tooth. It is assumed that the latter reflect the daily rhythm in the formation of dentin, and the Ebner lines correspond to the 5-day cycle of the formation of the organic dentin matrix, i.e., periods of less mineralization of the main substance of dentin.
Secondary and tertiary dentin.
Dentin deposited in the teeth of an adult during his life is called secondary (regular, or physiological) reparative dentin (Fig. 94).
In addition to the slower rate of formation, it differs from primary dentin (which arose during the embryonic development of the tooth) in having a less regular structure. This is expressed in a change in the course and number of dentinal tubules and collagen fibers with a lower degree of mineralization. The most active deposition of secondary dentin occurs in the side walls and in the roof of the pulp chamber, and in multi-rooted teeth - in its bottom. In this regard, with age, the shape of the pulp chamber changes: the pulp horns become less protruding, and its volume decreases. The intensity of secondary dentin deposition in men is higher than in women; it decreases with age. The thickness of the secondary dentin layer can be used as one of the indicators to estimate the dental age of an individual.
Rice. 94. Microphotograph of a vertical section of a mandibular molar.
1 – secondary (reparative) dentin; 2 – vestibular horn of the pulp; 3 – lingual horn of the pulp; 4 – dentin; 5 – enamel; 6 – tooth cavity.
The production of secondary dentin sharply increases with the destruction or abrasion of enamel and exposure of dentin (caries, increased tooth abrasion, exposure to chemicals, etc.). At the same time, in areas of the pulp corresponding to the area of tooth damage, there is a deposition of more or less significant masses of replacement dentin, which can protrude into the tooth cavity and change its configuration. Such dentin is called tertiary (irregular). Unlike secondary dentin, which completely lines the surface of the pulp facing the dentin, the formation of tertiary dentin occurs more or less locally, that is, only in places of the strongest influence of an unfavorable factor (Fig. 95).
The main function of tertiary dentin is to protect the dental pulp from the spread of bacteria, toxins, etc. It can form in any part of the wall of the tooth cavity, but most often appears in the area of the pulp horns. According to its structure (presence of osteoblasts, irregular course of dentinal tubules or even their absence, weak mineralization), it is closer to the bone and is therefore called osteodentin by some authors. In the dental cavity of elderly people, foci of osteodentin are also normally found, which can significantly change the configuration of the cavity, up to its complete obliteration.
Rice. 95. Topographical features of tertiary dentin (scheme).
1 – enamel; 2 – dentin; 3 – tooth cavity; 4 – defect in the area of the tooth neck; 5 – tertiary dentin; 6 – enamel defect (caries).
Denticles.
In the dental pulp, round or irregularly shaped bodies are sometimes observed, consisting of dentin or dentin-like tissue, which are called denticles, or pulp stones. According to their position in the pulp, they are divided into free, that is, lying directly in the pulp; parietal, maintaining connection with the tooth wall; interstitial, which arise when free or parietal denticles are overgrown with new layers of secondary dentin (Fig. 96).
As a result, the denticle becomes immured in the wall of the tooth (this process is more often observed at the root of the tooth, closer to its apex). Depending on the structure, it is customary to distinguish between highly organized (canalized) and low-organized (devoid of canaliculi) denticles. The sources of their formation are odontoblasts. As noted, denticles have the structure of dentin or dentin-like tissue, therefore they are called true denticles, in contrast to false denticles, which are foci of limited calcification in the pulp tissue.
The sizes of denticles are very variable - from barely noticeable grains to 2–3 mm in diameter. As a result of their growth, denticles can merge with each other, filling the entire tooth cavity or root canals, preventing endodontic manipulation. By squeezing the nerve fibers of the pulp, denticles can cause pain of a pulpitic nature. The reasons for their formation are not clear enough. Denticles are found both in the teeth of elderly people and in the teeth of young people, and even in tooth germs before their eruption [42, 61].
Rice. 96. Topography of denticles in the dental pulp (diagram).
1 – enamel; 2 – dentin; 3 – interstitial denticles; 4 – free denticles; 5 – parietal denticles; 6 – dental pulp.
5.1.1.2. Age-related changes in dentin
Dentin is a living tissue that is produced continuously throughout life. The formation of secondary and then tertiary dentin leads with age to a decrease in the size and volume of the tooth cavity - a process called pulp recession by clinicians. In addition, in the teeth of elderly people there are areas of dentin in which lime salts are deposited not only in the main substance, but also in the dentinal tubules and processes of degenerating odontoblasts. As a result, obliteration (“physiological” sclerosis) occurs, i.e., complete closure of the lumen of some groups of dentinal tubules, while the refractive indices of the tubules and the main substance are aligned and such areas look transparent. These areas are called sclerotic (transparent) dentin. Such dentin is also formed during caries or increased wear of teeth (“pathological” sclerosis), which can be considered as a protective reaction of the tooth to the action of destabilizing factors, which protects the pulp from irritation and infection (Fig. 97).
Rice. 97. Microphotograph of a vertical section of a mandibular incisor.
1 – enamel; 2 – dentin; 3 – dead paths in dentin; 4 – sclerotic dentin; 5 – reparative dentin; 6 – tooth cavity.
The formation of transparent dentin most often begins in the apical part of the root and progresses slowly towards the crown.
Typically, mineralization occurs first in the periodontoblastic space, and then captures the odontoblast process, less often vice versa.
Due to the fact that dentin sclerosis reduces its permeability, it can prolong the period of pulp viability. Obliteration of the dentinal tubules also leads to a decrease in tooth sensitivity.
With age, especially with increased tooth abrasion, the death of part of the odontoblasts and their processes and blockage of the inner ends of the corresponding dentinal tubules with tertiary dentin are also often observed. The contents of such tubules disintegrate, and the cavities of the tubules are filled with air or other gaseous substances. As a result, on thin sections of a tooth, groups of such tubules appear black in transmitted light (Fig. 98).
E. Fish [51] called groups of such tubules “dead paths”. The sensitivity of dentin in these areas is reduced.
In most cases, the dead spaces on the pulp side are, as noted, closed by the formation of irregular tertiary dentin.
Rice. 98. Microphotograph of a section of dentin.
1 – peripulpar dentin; 2 – pulp; 3 – tertiary dentin; 4 – “dead paths” of dentin.
5.1.1.3. Morphology of dentin in a clinical aspect
The “instant” reaction of the pulp to damage to dentin is due to the presence of a system of dentinal tubules, which can become pathways for the invasion of microorganisms, contributing to the rapid spread of the carious process. It has been shown that in cases where 1 mm2 of the dentin surface remains unprotected by enamel, about 30,000 odontoblasts are destroyed. Toxins, drugs and chemical reagents can penetrate through unprotected dentin, and the receptor apparatus of the pulp is also vulnerable to thermal influences. Dentin is most sensitive in the area of the dentinoenamel junction.
With demineralization of dentin, destruction of the dentinal processes of odontoblasts is observed. Under the action of enzymes secreted by microorganisms, the organic matter of demineralized dentin is dissolved. Along the periphery of the carious cavity towards the dental pulp, the dentinal tubules expand and become deformed. Closer to the tooth cavity there is a layer of compacted transparent dentin with significantly narrowed dentinal tubules.
The morphology of dentin must be taken into account when determining the treatment tactics for defects of hard dental tissues of both carious and non-carious origin.
One of the important clinical stages in the treatment of caries is the removal of softened and discolored (pigmented) dentin using various dental instruments (excavators, burs, etc.). An exception is the treatment of deep caries. In these cases, pigmented dentin is left at the bottom of the crown cavity and therapeutic pads containing calcium hydroxide (calmicin), zinc-eugenol paste and other materials are placed on it for several weeks or months. During this period, pulp cells become odontoblasts through cytodifferentiation, and the latter form reparative dentin, after which the dentist can remove pigmented dentin without fear of opening the tooth cavity.
Dental caries and its features
Dentin is a hard bone tissue that is located between the tooth enamel and the root and forms the basis of the tooth. Although dentin is a hard substance, it has a loose structure, contains many organic components and, without reliable protection of tooth enamel, is easily destroyed by the acid produced by bacteria. If the carious process has already affected the dentin, the disease will develop faster than with enamel caries.
The following signs are characteristic of dentin caries:
- the formation of a carious cavity (if there may be no cavity when the enamel is damaged, then with dentine caries there is always a hole in the tooth);
- toothache (as a rule, carious damage to the bone tissue of the tooth is accompanied by pain - first as a reaction to hot, cold, sour, sweet, and with deeper damage - as independent pain);
- bad breath (it occurs as a result of decay processes occurring in the carious cavity);
- discomfort when chewing (occurs if a carious cavity is located on the chewing or contact surface of the teeth);
- difficulties when using dental floss (when cleaning between teeth, the floss gets stuck, breaks or is damaged);
- change in tooth color (takes on a yellowish or brownish tint).
Any of these symptoms, and especially a combination of signs, most likely indicates damage to dentin by caries and requires contacting a dentist.
Features of dentin in temporary teeth
The thickness of dentin in a baby tooth is approximately half that of a molar. This is explained by its faster formation and shorter lifespan of a temporary tooth. The tissue in children is lighter, it contains fewer minerals, it is softer, it is better prepared, so the treatment of caries of milk teeth is faster. Peritubular dentin, in turn, is practically absent, the tubules are wider and are not subject to sclerosis. Intrauterine dentin is characterized by uniform mineralization.
How does a tooth hurt with dentin caries?
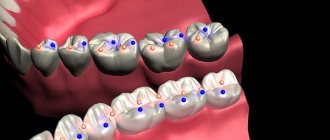
Different types of pain are characteristic of different stages of caries. When dentin is damaged, the stages of medium and deep caries are distinguished. In the first case, the carious cavity is located closer to the enamel; in the deep stage, it is as close as possible to the area of the dental nerves.
The middle stage of dentin caries is characterized by a painful reaction in response to temperature or taste stimuli, the pain quickly passes, and the intervals without pain are quite long.
If caries is in the stage of deep damage to dentin, it is characterized by intense long-term pain with short intervals without pain.
Deep caries is the most dangerous, because at any moment it can be complicated by pulpitis, periodontitis, purulent inflammation, and the spread of infection beyond the dental tissues. But even the moderate one can turn into the deep stage at any moment, so if you have a toothache of any nature, you should consult a dentist as soon as possible.
Isolated dentin caries: what are its features
Sometimes lesions and extensive carious cavities form in the dentin of a permanent tooth while maintaining the integrity of the enamel. This is how isolated, atypical caries develops. Its difference from the classical form is that the carious lesion does not affect the enamel, but immediately passes to the dentin.
This happens, for example, in cases where a person uses fluoride preparations for a long time for preventive purposes. This leads to strengthening of the enamel located on top of the affected dentin, and, as it were, “seals” the pathological process inside the tooth.
What are dentinal tubules
They look like thin tubes that taper in the outer direction and penetrate the tissue from the pulp to the periphery. In the depths they branch, and inside they are filled with Toms fibers, which nourish dentin and saturate it with mineral salts. It is the dentinal tubules that ensure the high permeability of dentin, despite its dense structure. This allows the pulp to quickly respond to damage.
The dentinal tubules also contain dentinal fluid. Its movements cause pain and sensitivity in the teeth. It is believed that due to temperature, mechanical or other effects, the liquid begins to move, irritating the nerve endings in the pulp.
Basic diagnostic methods
Independent determination of dentin caries is possible based on pain and other unpleasant symptoms. However, only a doctor can make an accurate diagnosis after conducting a full dental diagnosis. It includes basic and additional research methods.
The main diagnostic methods for dentin caries include the following:
- Probing - using a sharp probe, the doctor determines the presence and depth of carious cavities. If the bottom of the cavity has a soft structure and a light brown color, this may indicate an acute course of caries. Dense pigmented dentin in the bottom area indicates a chronic form of the disease. Also, with the help of probing, you can detect hanging edges of tooth enamel, chips on it, and by the localization of pain during probing, determine the depth of the carious lesion.
- Percussion is tapping on the teeth with tweezers or the back of a dental probe.
- Palpation - feeling.
These methods are used to determine the viability of the pulp, which is especially important in differential diagnosis.
Additional research methods include:
- Thermometry - measuring the temperature of dental tissues.
- Electroodontometry is the study of pulp using electric current.
And the following methods are used to assess the condition of the pulp:
- X-ray - an X-ray of the tooth helps determine the exact location of the carious cavity and its depth.
- Transillumination - the transillumination method is widely used in the diagnosis of hidden dentin caries, for example, with an isolated, atypical form of progression. When transilluminated, healthy tissues appear transparent, while those affected by caries create a shadow effect.
When the doctor has made a preliminary diagnosis based on the above methods, differential diagnosis of dentin caries with other types of dental diseases - enamel caries, pulpitis, periodontitis may be required.
Self-detection of caries
The disease cannot always be detected on its own. To diagnose dentin caries, the following methods are used:
- visual inspection;
- percussion and palpation;
- probing the carious cavity;
- radiography (single tooth or panoramic);
- fluorescent stomatoscopy.
Experts can also recommend other modern techniques, performed manually or using dental equipment. It should be borne in mind that many dental diseases have similar symptoms with completely different treatment methods.
How is dentin caries treated?
Treatment of moderate dentin caries and deep-stage carious lesions is carried out only surgically through preparation of the carious cavity. At any stage of such caries, pain will occur during treatment, so in most cases local anesthesia is used.
Dental treatment of dentin caries takes place in several stages:
- Cleaning the tooth surface from plaque and tartar.
- Selection of the optimal color of the filling, which will closely match the natural shade of the teeth.
- An anesthetic injection with an anesthetic drug into the area of the tooth that requires treatment. To reduce pain, the injection area is lubricated with anesthetic gel.
- Isolation of the tooth from saliva and neighboring teeth using a latex lining - rubber dam.
- Preparing a cavity using a drill. The dentist removes the lesion with caries: aligns the edges of the enamel that hang over the cavity, removes the softened and pigmented layer of dentin, and forms the correct cavity for convenient and high-quality filling.
- Washing, treating with antiseptics and drying the cavity after preparation.
- Acid etching and adhesive application are an important step in the treatment of caries in permanent teeth. These procedures provide better adhesion of the filling to the walls of the cavity.
- Installation of an insulating or therapeutic pad. The first prevents the negative impact of the filling on the dental pulp, the second has a therapeutic effect if it is necessary to relieve inflammation.
- After preparing the cavity and thoroughly preparing it for filling, a filling is installed. Today, fillings are mostly made from photocomposite materials. They dry quickly under the influence of light, have good strength and do not shrink.
- Alignment according to the bite, polishing and grinding help to adjust the filling to the anatomical features of the jaw and give it the necessary aesthetic characteristics.
- Dentist's recommendations for the prevention of recurrent caries, dental care, selection of optimal hygiene products.
At this point, the process of treating medium dentin caries can be considered complete. Therapy for deep caries has its own characteristics. After preparing the cavity, the dentist places a therapeutic pad with calcium on its bottom in the area of the most painful point. Some experts do not recommend completely preparing softened dentin in case of deep caries. After treatment with an antiseptic, they first recommend installing a temporary lining with a therapeutic effect, and after a certain period, removing the temporary filling and performing the final restoration of the tooth.
Prevention of dentine caries in permanent and baby teeth
Measures to prevent dentin caries are similar to the prevention of caries in other parts of the tooth.
These include:
- Proper nutrition with a minimum amount of sugars and fast carbohydrates, rich in fluoride, calcium, phosphorus. Avoiding frequent snacking.
- Thorough daily brushing of teeth twice a day using a toothbrush, paste, and floss. The additional use of an irrigator to clean hard-to-reach places and interdental spaces, as well as mouth rinses, helps reduce the risk of caries.
- Schedule a visit to the dentist twice a year, as well as immediately contact a doctor at the first sign of caries.
- Professional teeth cleaning using special equipment twice a year.
- If necessary and as prescribed by a doctor, use vitamin-mineral complexes, which contain components beneficial for dental health.
- Drinking fluoridated drinking water, which is enriched with minerals.
Compliance with these preventive measures allows you to maintain the health and beauty of your teeth and reduces the risk of developing caries and other dental diseases.
Fact one: color component
One of the most common misconceptions is that the color of a tooth is the color of its enamel. In fact, the color characteristic directly depends on the dentin, which determines the shade of the smile. Although the enamel is the strongest part of the tooth, it is still transparent, and the color of soft dentin is visible through it. The palette ranges from white to gray and yellowish.
Don't be upset if your smile is not snow-white. Today you can whiten your teeth in many ways - from going to the dentist and using pastes with a dispersed phase to using specialized preparations and devices. But the main thing is the health of the teeth, their strength and beauty. Those with yellow teeth, as it turns out, are incredibly lucky, because their bodies are saturated with minerals, which means no bacteria are scary. As you know, yellow teeth are not necessarily a lack of proper care; often the color is transmitted genetically.
Interesting! In the old days in Rus', teeth were whitened with birch charcoal, but doing this with gunpowder or salt was strictly prohibited.