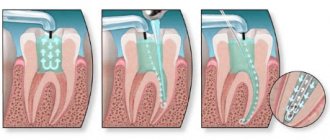
During endodontic treatment, a popular practice is to temporarily fill the root canal. As part of this procedure, a special paste is placed inside the canal, which has many healing properties. Such a filling can be applied for either a couple of days or several months, depending on the chosen treatment method. At the end of treatment, the temporary filling is replaced with a permanent one.
The specific period for which a temporary filling is installed is determined by the dentist. Most often, a material with a long duration of action is selected so that the treatment effect is maximum.
In some cases, medicinal pastes can be used in combination with disinfectants and antiseptics. This combination significantly increases the effectiveness of treatment. In addition, these drugs help reduce the risk of infection of soft and hard tissues.
Features of temporary filling with pastes
In the case of a specific degree of development of the disease, the techniques for temporary filling of root canals may differ. This is justified by the peculiarity of the technique used during treatment. In acute forms of the disease, potassium hydroxide is injected into the canal, often without compaction and for a period of 1 to 7 days based on the clinical picture.
The main goal of the procedure is to prevent the appearance of inflammatory processes and harmful microorganisms inside the canal. In case of chronic diseases, the drug is most often administered with compactions for a period of up to 2 months. If necessary, the material used can be periodically replaced until the desired result is achieved. Based on general practice, treatment can last from six months to 1 year, depending on the extent of the disease, as well as the characteristics of the individual patient’s body.
The application of a temporary filling is also aimed at stimulating the processes of regeneration of damaged cells. To do this, the following filling techniques are used:
- the canal is cleaned and prepared, after which paste is placed in it for a period of 7 to 10 days;
- at the end of the period, the old layer of paste is removed and replaced with a new one;
- After a certain time, the manipulations are repeated (the exact timing is announced by the dentist).
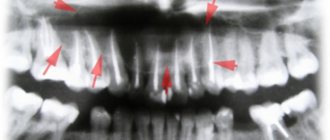
To provide a clear picture of the treatment, an x-ray is taken. It must be performed no earlier than 3 months from the date of the patient’s first visit. The fact is that in the first stages of treatment the result can be variable.
X-ray of teeth
At the end of all procedures, restoration of damaged tissue takes about 3-5 years. During this period, it is recommended to follow all the doctor’s recommendations so as not to repeat the next development of the disease.
Modern Moscow dentistry uses potassium hydroxide-based preparations with various antiseptic additives.
Granulomas on the roots, we treat the tooth canals
In the article “Available about root canal treatment,” I discussed in theory what proper endodontic treatment should look like, and what happens when it is not performed entirely in line with modern requirements. And today I propose to support the theory with practice and analyze one of the interesting clinical cases from my own practice.
So, a young man approached me with a referral from an orthodontist and a desire to save a tooth, or rather, what was left of it. This is how he looked at the time of our meeting on an x-ray.
This is the upper 6th tooth (designated by dentists as 16, there is a lot of detail about the numbering of teeth in dentistry). His background is as follows: a couple of years ago he was treated for pulpitis. Everything was as usual - they removed the nerve, somehow cleaned the canals, filled them and put in a big filling. As you can now see, very little time passed and a natural “accident” happened: the tooth and the filling broke. What’s bad is that one of the walls broke below the gum level. I will explain further why this is bad. As a result, we have 2 main problems that threaten the tooth with removal - a deep level of chipping of the palatal wall (indicated in the picture with a red line) and poorly treated canals (the unpassed part of the canal is indicated by a white dotted line), one of which has radiological signs of chronic inflammation - granulomas (its outlines are indicated by a black dotted line).
But despite these problems, the patient had a strong desire to preserve his own tooth by any means available. What was ultimately done for this?
In order to better understand and evaluate, we must say what shortcomings we had to correct... and what you can see for yourself in the picture of your teeth:
- barely noticeable white stripes on the x-ray - this is the filling material in the canals. Such thin, interrupted “threads” that do not reach the top of the root indicate that the canal was poorly expanded, and therefore not sufficiently treated with solutions to remove organic residues from it
- darkening around the tips of the roots (in this case around one root) indicates the presence of a chronic inflammatory process on this root. This is precisely caused, as a rule, by errors in the processing of the canals during previous treatment.
So, during the re-treatment, it was discovered that in addition to the 3 previously treated canals in this tooth, 2 (!!!) additional canals were missed at once. Those. they were not discovered by the doctor and were simply closed with all the remains of the pulp, which acted as a food storehouse for the microflora. It is on this root that the inflammatory focus is visible on x-ray. In addition, the so-called "step". In dentist jargon, this unpleasant thing means that the doctor has deviated from the natural course of the canal and lost it, resting on the hard tissues of the root. As a result, the apical part of one of the previously discovered canals also remained underprocessed.
The picture on the left shows 3 instruments inserted into 3 different canals in the same root. On the right picture, the black dotted line indicates the outline of the granuloma, the blue line outlines the outline of the root, the white dotted line indicates the untraversed part of one of the 3 canals, the red arrow shows the part of the canal in which a “step” was made during the previous treatment
Ultimately, these errors were corrected, two undetected channels were completely processed, and the step in the third was bypassed by finding the correct path. In total, after all the instrumental preparatory measures, it turned out that there were 5 separate canals in this tooth.
This control image taken before filling shows all 5 individual canals...
This is a photo of a tooth cavity, in which 5 separate orifices of all five canals are visible. Channels 1,2,5 are the main ones. It was they who were found and processed during the previous treatment, although not perfectly. Quite often, there are additional canals in the upper molars (3,4). Their mouths are initially very small, sometimes barely noticeable, and quite often these channels remain undetected. This is one of the common causes of complications after endodontic treatment...
This is quite a rare case. Still, usually in the upper molars there are 3-4 canals, very rarely less than 3. But no less rarely, more than 4. This is just that rare case, and therefore interesting.
The result of 2 visits (1 hour + 1.5 hours) was the filling of all canals.
Now all 5 canals are sealed exactly to the top of the root. All that remains is to wait for the inflammatory process to disappear.
The same thing, but the view from the tooth cavity. The canals are tightly sealed with gutta-percha*. Next comes tooth restoration.
Further, the remaining root due to serious damage will be restored with a stump insert* and a crown. True, before that, the surgeon will still have to tinker with him in order to solve the second problem of this sufferer after the canals (I talked about it at the beginning). We are talking about a deep chip of the palatine wall. The fact is that for high-quality restoration it is very important that the edges of the tooth rise at least 1-2 mm along the entire perimeter above the level of the gum (it is allowed that in some places the edge of the tooth coincides with the level of the gum). This will make the restoration airtight and preserve the remains of the tooth for many years to come. In this case, the wall was chipped on the palatal side below the gum, which means we will have to remove some part of it in order to transform the subgingival defect into a supragingival one. This manipulation is called “surgical lengthening of the clinical tooth crown.” I will also talk about this, though in other posts.
This completes the story of saving one single tooth.
Finally, I want to make a couple of small but important additions to this clinical case.
Firstly, very often in such situations the patient faces a dilemma: keep his tooth, fight for it until the last drop of... the sweat of your dentist, or remove it with subsequent prosthetics? In such cases, the last decision, dear friends, remains with you, the patients. Repeated canal treatment, correcting mistakes already made by the previous dentist (and, perhaps, your own) always remains a difficult task, and therefore no one can ever give a 100% guarantee on the final success of all rescue measures. What factors does the doctor take into account?
Objective:
— the condition of the tooth (and not only the canals)
- opportunities for its subsequent QUALITY restoration (you can perform a feat in the canals, but then, without properly assessing the degree of tooth destruction, make an inadequate restoration, and in the end still lose it)
— the importance of preserving a specific tooth (it seems that all teeth are important, you might say, but there are still situations in which the heroic saving of a tooth makes absolutely no sense, for example, this often happens with wisdom teeth)
Subjective:
- the equipment of your workplace (the presence of a rubber dam, an apex locator, a large number of various files *, x-rays, ultrasound, magnifying equipment - in general, everything that I have already written about earlier and without which “picking in the canals” is impossible). Why do I include completely objective things here? Yes, because, unfortunately, many doctors believe that it is possible to work “high quality” without something from this list, or even without everything at once. Sensitivity of fingers and experience, they say, you can’t drink away, as they say. This is self-deception.
- skills, knowledge, experience - well, everything is clear here... it’s very difficult to soberly evaluate your loved one. And in conditions of high competition, it is still somehow not customary for us to send patients somewhere to colleagues who are more equipped and “advanced” in some narrow issues. Proximity to the body of one's pocket may outweigh the patient's interests.
Based on this, the doctor should try to give an honest, objective prognosis for the success and feasibility of treatment. And remind you that only surgeons using forceps can achieve 100% results. If you are then ready to invest time and money in treatment without guarantees, go to battle. If you do not accept even 1% of possible failure after mutual efforts and your waste of money, you move to the surgeon’s office. In addition, it should be noted that from a financial point of view, canal retreatment followed by prosthetics usually costs the patient about the same as tooth extraction followed by implantation. At the same time, tooth extraction gives a more predictable result. The success of complex endodontic treatment over a 5-year period, even with the most remarkable specialist, does not exceed 70-80%. For implantation, the same figures are approximately 95%. So in the matter of “pulling” hopeless teeth, it is always worth soberly assessing the risks.
And the second addition... The modern protocol for the treatment of chronic inflammatory processes around the root (what is often called a granuloma or cyst ) involves opening and closing the canals as little as possible. What am I talking about? Some time ago it was “fashionable” in cases like the one I analyzed to put “medicine” (calcium preparations) into the channels and “marinate” it there for a long time. At the same time, change it several times with some frequency (and each dentist had his own favorite scheme - some once a week, some once a month, and some in accordance with the phases of the moon... just kidding). At the same time, it was believed that this should be done for 6-12 months and monitor whether the cyst “goes away.” So... This is already a very outdated approach, which has many disadvantages, the main one of which is the absolute pointlessness of keeping calcium preparations in the root canals for a long time. Therefore, such an approach, at a minimum, will not make you better (if you don’t consider wasting your money and your time a big loss), at most, it can do harm (for example, a temporary filling during a long wait by the sea for good weather will begin to “leak” or even fall out, leaving microbes the opportunity to again settle in the tooth canals and immediately making all previous treatment meaningless). Even in cases of exacerbation of inflammation, in the presence of swelling, pain, fistula, discharge from the canal... the modern treatment protocol remains the same - open the canals, thoroughly clean and wash (in case of exacerbation, this stage takes a longer time), immediately seal with permanent materials, make a good sealed restoration, and then sequential monitoring after 3.6 months. All this in 1-2-3 visits within a minimum time. No many months of walking with calcium, no numerous replacements, no walking with an open canal in the tooth, rinsing it and plugging it with cotton wool while eating, no leeches - all this is yesterday and the day before yesterday. If you are offered something like this, you can safely turn towards the exit, you can’t go wrong...
Indications for the procedure
Temporary filling of 1 root canal is a standard procedure during endodontic treatment. Among the general indications are the following:
- significant damage to the root canal is observed (most often due to the chronic form of pulpitis);
- the purulent stage of pulpitis was diagnosed (location does not matter);
- there are serious damage to intraradicular soft tissues.
First of all, the patient will have an x-ray to analyze the working length of the root canals, as well as the possibility of carrying out the procedure.
To begin treatment, it is necessary to carry out instrumental treatment, during which the canal acquires the desired shape. At the end of the mechanical manipulations, the funnel-shaped canal is directly treated.
During treatment, various types of pastes can be used. It all depends on the characteristics of the disease, the extent of infection, and the patient’s preferences.
Types of pastes
One of the most popular drugs is a paste based on antibiotics and corticosteroids. Most often, such a paste contains about 3 antibacterial agents with a wide spectrum of action. Such drugs have a complex effect and significantly accelerate the regeneration of damaged tissues. The paste also contains a radiopaque filler. It is necessary for a visual assessment of the quality of channel filling. This paste has an extremely strong effect with a minimal duration of action. The filling is applied for a period of 3 to 7 days.
An equally popular paste is a material based on metronidazole. The peculiarity of this paste is the effective suppression of pathogenic microflora in the root canals. In addition, the unique properties of the drugs used make it possible to stop the destruction of hard and soft tissues, as well as prevent the occurrence of inflammatory processes. Most often, metronidazole paste is used in case of excessive infection of the canals.
Another type of paste is a preparation based on an antiseptic mixture with a long-lasting effect. This material has an extremely strong effect due to a number of antiseptic components. The paste does not harden, but slowly dissolves, enriching the tissue with healing elements. Most often, this material is used to diagnose pulpitis or periodontitis, as well as in case of problems with baby teeth.
The fourth variety is potassium hydroxide paste. This drug ensures the beginning of a highly alkaline reaction, during which all existing bacteria and other harmful microorganisms are destroyed inside the root canal. For severe forms of periodontitis, non-hardening forms of the material are used, which are placed in a specific canal using a special filler. This paste must be changed every 6-8 weeks. The exact frequency is determined individually by the attending physician.
Note that, regardless of the specific category of pastes, it is extremely rare to completely cure damaged tissue in one session. The patient is assigned several sessions, during which the effectiveness of the current treatment process is diagnosed, as well as the need to apply another filling.
Long-term exposure to calcium hydroxide in maxillary anterior teeth (clinical case)
In our dental practice, calcium hydroxide has taken a leading place as medicinal pastes for intracanal therapy only in recent decades, although the use of calcium hydroxide in dentistry has been known since 1838 (Nygren), but this paste has been most widely used in the dental world since 30 years of the last century, with the aim of antimicrobial effects on the microflora of root canals (LRG Fava. WP Saunders. Calcium Hydroxyde pastes: classification and clinical indications. IEJ, 1999). To date, calcium-containing pastes are one of the main drugs in the treatment of infected canals (Ingle's Endodontics 6, Chpt 28, 1009-1010, 2008).
However, in the scientific community there is still no consensus on how long it is possible or necessary to put calcium hydroxide into the root canals. Typically the exposure period is recommended from 1 to 4 weeks. But, works are often published where the exposure period reaches up to 6 months. It seemed like something like that here? Who among us does not have patients who suddenly disappear for six months to a year with calcium hydroxide in the canal, and when we appear we do not find any noticeable exacerbation of the process in them. The inflammatory process either heals during this time, or the temporary restoration we created falls apart and the inflammation persists. In such cases, we blame the failure on failed coronal sealing.
However, among the studies examining prognostic factors affecting the periapical status of the tooth, calcium hydroxide exposure was not even included in the list of prognostic factors. Among such factors, greater importance is still given to the initial periapical status of the tooth and instrumentation with obturation along the entire length of the root canal (NChugal “Endodontics Prognosis”). The additional use of calcium hydroxide adds percentage to the success of treatment (“Reduction of Intracanal Bacteria Using Nickel-Titanium Rotary Instrumentation and Various Medications” G Shuping, D Orstavik 2000 JOE) but is still not able to completely remove the bacterial flora from the root canals (“One-versus Two-visit Endodontic Treatment of Teeth with Apical Periodontitis: A Histobacteriologic Study", Jorge Vera, DDS, Jose F. Siqueira, Jr, DDS, MSc, PhD, Domenico Ricucci, JOE 2014).
In the presented clinical case, a long time investment (more than 6 months) of calcium hydroxide was used in order to obtain sterility of the root canal of tooth No. 11. However, over time, after about six months, the inflammatory process not only did not decrease in size, but repeated exacerbations began to appear. Changes in the root canal treatment protocol, the use of additional irrigants, and an increase in the size of root canal treatment also did not bring any changes to the dynamics of the process. They began to “prepare the patient for resection of the root apex,” additionally “killing” tooth No. 12, since, according to the doctors, curettage of the periapical area could damage its neurovascular bundle.
This patient came to me with approximately the same input data. I decided that perhaps the reason for the failure of the treatment lay in insufficient instrumentation of the root canal of tooth No. 11, so I carried out my chemo-mechanical treatment, increasing the size of the finishing file to ISO 70. Additionally, instrumentation of tooth No. 12 was carried out to size No. 55 according to ISO. However, 10 days after the administration of calcium hydroxide, the tooth worsened the inflammatory process. This became an additional intraoperative factor that reduces the prognosis of treatment (Ng YL, K Gulabivala, T Mann “A prospective study of the factors affecting outcomes of NSRT”, IJE, 2011). Among other factors that negatively affected the prognosis, there was also the factor of the size of the lesion, in particular, according to the study by S Hoskinson (“A retrospective comparison of outcomes of root canal treatment” Oral Patogy Oral Medicine 2002), an increase in the size of the periapical process by 1 mm results in a decrease in success rate by 18%. Therefore, on my part, it was decided to perform apical microsurgery with resection of the apexes of the roots of teeth 11 and 12 after their obturation.
According to the preoperative CBCT analysis, the outer cortical plate of the upper jaw and the lower wall of the nasal cavity were missing, therefore, despite the routineness of the procedure, the curettage process was complicated by perforation into the nasal cavity. This defect was isolated by a biological membrane. The postoperative course was unremarkable. Observations were carried out at 6 and 12 months, after which it was possible to conclude the success of the treatment carried out according to the criteria of the European Society of Society.
Photo report of the work
Video report of the work
Preparation for the procedure
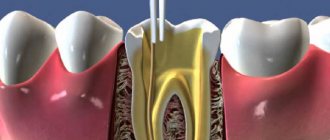
Proper preparation is the most important aspect of endodontic treatment. If you do not provide for all possible nuances, the effectiveness of the procedures may be reduced to zero. Before filling directly, it is necessary, first of all, to thoroughly clean the root canal of any plaque that has formed, and also remove all damaged tissue.
In general, all preparatory actions are quite standard. They are carried out in stages and have the following action plan:
- carious lesions are eliminated, as well as dead tissue (specialized drills are used for this);
- pulp is removed from open canals;
- An x-ray is taken to determine the specific shape and length of the canal;
- The root canal is expanded to the required size using various attachments and other tools.
Please note that strict adherence to all of the above points is the key to effective treatment. If you neglect at least one of these stages, with a high degree of probability the current situation will only worsen.
How is canal filling done with paste?
Proper filling of root canals promotes a speedy recovery without any complications. To do this, it is necessary to use proven and high-quality drugs, as well as sterilized dental instruments. Only a highly qualified doctor can perform the procedure correctly, so we recommend contacting only reputable dental clinics.
Filling is performed in stages with a clear sequence of actions:
- All affected tissue is removed. In some cases, the practice is used to remove healthy tissue in order to gain unhindered access to each section of the canal.
- Pulp extraction.
- Channel length analysis. Note that the length of the canals varies; the root and its bends play a special role in this matter.
- Mechanical processing of channels. The channels are carefully processed along their entire length to create the maximum possible space. If this is neglected, the material will not be able to spread throughout the entire volume of the channel.
- Canal filling with gutta-percha. The last stage of work. Its effectiveness will directly depend on the correct measurement of the channel length, as well as on the quality of the machining.
Pain in the tooth after canal treatment, if there is a focus of inflammation in the bone
If a patient comes in with pain that intensifies when food hits the tooth, with a feeling of internal pressure from inside the tooth, almost always in such cases there is inflammation in the bone or around the root. This situation occurs when the nerve is destroyed, rots and the entire infection comes out of the tooth into the bone, forming an inflammatory focus - a cyst or granuloma. Treatment in this case is quite complicated, and the tooth cannot always be saved. If the doctor believes that there is a chance to cure the inflammation, he treats the root canals and leaves turunda with an anti-inflammatory solution or medicinal paste in them under a temporary filling for 1–2 weeks, after which he fills the canals with permanent hardening materials. In some cases, the pain does not go away immediately. Therapeutic agents gradually take effect, so the first few days after treatment the tooth may hurt. As a rule, in such cases, additional treatment is prescribed in the form of anti-inflammatory tablets (Nise, Ibuprofen), antibiotics (Amoxiclav, Lincomycin) or antimicrobial agents (Trichopol). Rinsing with warm soda solution helps relieve pain.
There is no need to be afraid of root canal treatment and nerve removal. Modern pain relievers will effectively help you carry out the entire procedure without any pain. Mechanical preparation of hard tissues, cleaning of the tooth cavity, treatment and filling of root canals are necessary procedures, but they should be carried out in compliance with all the rules. High-quality root canal treatment is the key to tooth preservation.
What can pain after filling indicate?
In this case, the degree of pain plays a key role. Minor discomfort for several days after the procedure is a completely natural consequence. This happens due to irritation of the tissues and pulp, so there is nothing wrong with it. In addition, the patient may experience a feeling of some swelling inside the tooth, which is also normal.
Another thing is severe pain, which can be accompanied by hemorrhages in the oral cavity. This indicates the presence of a serious error during the filling. In this case, it is necessary to contact a dental clinic as soon as possible for an examination.
In general, to avoid unpleasant consequences, we recommend following the standard rules:
- do not expose your teeth to excessively cold temperatures, especially after drinking hot drinks;
- maintain oral hygiene;
- regularly brush your teeth both at home and in the clinic (professional ultrasonic cleaning, etc.);
- undergo routine dental checkups;
- do not neglect your doctor's advice.
Following these simple recommendations will help maintain healthy teeth for a long time.
Pain after nerve removal and root canal treatment
One of the most common misconceptions among patients is that a tooth without a nerve cannot hurt. In principle, there is truth in this. But it's not that simple. Nerve fibers exit the tooth through the apical foramen in the root and unite into common trunks, thicker and more powerful. Such a trunk may be responsible for the sensitivity of the entire half of the jaw or face. This explains the irradiation (passage) of pain along the entire nerve if the inflammation affects only one tooth. The impulse is transmitted through nerve fibers to neighboring areas - ear, temple, eye, eyelid, forehead, etc. When a nerve is removed (tooth depulpation), it is simply torn off from the main trunk, causing inevitable injury to the tissues. Canal cleaning takes place under anesthesia and the patient does not feel the moment the instrument exits through the tooth. Without proper control over this procedure, a hematoma (local hemorrhage) may form in the area of the apex of the tooth root, which will cause pain when pressing on the tooth or clenching the jaws. A feeling of mild pain in a pulpless tooth is acceptable for 1–2 days. As a rule, with high-quality cleaning of the contents of the tooth cavity, there is no painful reaction from temperature stimuli (cold or hot water), no severe throbbing or aching pain. If the doctor removed the nerve from the tooth, treated the canals and left a turunda with an antiseptic in them, the tooth should not hurt. If, some time after treatment, the patient notices severe pain, which intensifies in the evening or at night, it is necessary to re-clean and rinse the root canals. This needs to be done as quickly as possible; you should not endure the pain or relieve it with medications. Short-term help can be provided by painkillers: Pentalgin, Ketanov, Tempalgin and others.
The occurrence of throbbing pain from hot water after root canal filling
Treatment of tooth canals involves not only treating, cleaning and drying them, but also filling them with special filling materials. As a rule, pastes for these purposes are used with or without anti-inflammatory additives. Filling the canals is necessary in order to eliminate the possibility of creating conditions for the growth of bacteria. When the tooth cavity is densely filled with gutta-percha pins and paste, there are no such conditions. If some of the infected tissue gets behind the root apex during canal treatment, the inflammation spreads to the bone. Pain in the tooth appears almost immediately after root canal treatment or during the first days and has a certain character: pulsating, twitching, shooting, aggravated by heat. In order to eliminate such a complication, it is necessary to carefully treat the tooth canals using the correct technique. If such pain occurs, it is necessary to re-treat the canals; a short-term effect is achieved by taking painkillers with an anti-inflammatory effect: Nise, Ibuprofen. In some cases, rinsing the mouth with a warm soda solution (1 teaspoon of salt and soda per glass of water) has a positive effect.