Chronic sialadenitis is an inflammation of the salivary glands, in which periods of exacerbation alternate with periods of remission. This type of disease manifests itself differently in men, women and children. During reduced activity of the pathological process, symptoms of the inflammatory process are practically absent. During an exacerbation, there is a painful swelling in the cervical spine, an unpleasant taste in the mouth, and difficult salivation. Treatment is aimed at containing changes in the structure of the salivary gland tissue and eliminating painful symptoms.
Classification of forms of chronic sialadenitis
Depending on the area of localization and similarity of symptoms, three main forms of sialadenitis are distinguished:
- Parenchymal sialadenitis . Parenchyma is the collection of functional cells that make up the salivary gland. The inflammatory process is based on changes in cells of this type. Women are more often susceptible to this form of the disease. Parenchymal sialadenitis affects the parotid salivary glands.
- Interstitial sialadenitis. This type of inflammation occurs in the interlobular space of the gland. Most often it affects men. Interstitial sialadenitis affects the submandibular salivary glands.
- Ductal sialadenitis Occurs due to congenital pathology of the salivary ducts or as a result of their injury. Most often it occurs in older people.
General information
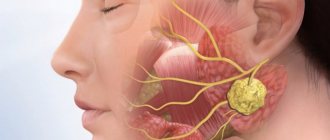
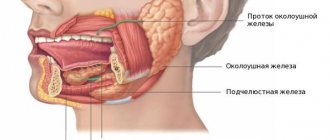
Sialadenitis is an inflammatory process in the salivary glands. In humans, there are three pairs of salivary glands in the oral cavity, which secrete saliva and discharge them into the oral cavity through special ducts, thereby ensuring a normal digestive process. These are the parotid , submandibular and sublingual glands.
The main functions of saliva are to soften food and also facilitate the process of swallowing it. During the inflammatory process, the production of saliva becomes difficult, and during the process of eating a person feels significant inconvenience. During the development of the disease, pain, swelling of the face, etc. are noted. If the process progresses, a purulent cavity or tumor may form. The disease develops in both young children and adults. Damage to the salivary glands requires consulting a doctor and carrying out the prescribed treatment. The ICD-10 code for sialadenitis is K11.2. How inflammatory diseases of the salivary glands manifest themselves, what treatment is most effective in such cases - this will be discussed in the article.
Diagnosis and treatment of salivary gland diseases
Saliva is a complex mixture of fluid, electrolytes, enzymes, and macromolecules that together perform several important functions: moistening the mouth to aid swallowing and digestion, digesting starch via salivary amylase, modulating taste, and protecting against tooth decay and pathogens. The major salivary glands include the paired parotid, submandibular and sublingual glands, and the minor ones are contained in the mucous membrane of the lips, tongue, oral cavity and pharynx.
Diseases of the major salivary glands sometimes occur in the practice of a family doctor. Approximately half of the cases of benign diseases of the salivary glands are due to obstructive sialadenitis (caused by the presence of stones or stricture). Salivary gland tumors are relatively rare: they account for only 6% of all head and neck tumors, with an incidence of 2-8 cases per 100,000 people in the United States. Clinical manifestations of infection and inflammatory processes of the salivary glands are varied.
Acute purulent sialadenitis ICD K11.2.
Acute sialadenitis is a bacterial inflammation of the salivary gland, usually affecting one large gland (most often the parotid) and often occurs in disabled, hospitalized or post-operative patients. Inflammation occurs due to retrograde bacterial infection by oral contents. Stasis of salivary outflow as a result of dehydration or decreased fluid intake by the patient promotes the migration of bacteria into the parenchyma of the gland.
Causes
The following factors contribute to the development of acute sialadenitis: diabetes mellitus, hypothyroidism, renal failure and Schöngren's syndrome. Some drugs, especially anticholinergics, impair the flow of saliva. Sialolithiasis and ductal strictures can also impair salivary flow and contribute to acute infections, but are more likely to cause chronic or recurrent infections. A common bacterial causative agent of acute sialadenitis is Staphylococcus aureus (50-90% of cases), less often - streptococci and Haemophilus influenzae.
Clinical signs
Patients with acute sialadenitis usually complain of acute pain and swelling of the affected gland. During a physical examination, compaction, swelling and severe tenderness on palpation can be detected, and during a massage of the gland, pus may be discharged from the opening of the duct in the oral cavity, which can be taken for culture.
Discharge of pus from the opening of the parotid gland duct in a patient with acute purulent parotitis
Treatment
Treatment includes antibiotic therapy and measures to correct the primary pathology and risk factors. Stimulate saliva flow through warm compresses, salivary aids, adequate hydration, salivary gland massage, and oral hygiene. Empirical antibiotic therapy is directed against gram-positive microorganisms and anaerobes, which are often resistant to penicillin, so it is recommended to prescribe penicillins protected by β-lactamase inhibitors (for example, amoxicillin-clavunate [Augmentin]). If possible, antibiotics should be prescribed according to culture results. Rarely, acute purulent sialadenitis can lead to abscess formation; in this case, surgical drainage is necessary.
Recurrent mumps ICD B26
An inflammatory process of the parotid gland, which is characterized by recurrent episodes of swelling and tenderness. Etiology unknown. Children experience recurrent episodes of acute or subacute parotid swelling with fever, malaise, and tenderness. Usually the pathology is unilateral, although it can be bilateral, episodes last from several days to several weeks and can recur every few months. Treatment includes supportive care with adequate hydration, massage of the gland, warm compresses, medications that promote salivation, and antibiotic therapy. Sialendoscopy has been shown to reduce the frequency and severity of relapses. With the onset of puberty, the disease resolves spontaneously; surgical interventions are rarely performed.
Child with swelling of the parotid gland
Chronic sialadenitis
It manifests itself as recurrent episodes of pain and inflammation caused by impaired flow of saliva and salivary stasis. The parotid gland is most often affected. The primary etiological factor is obstruction of the salivary duct by stones, stricture, scar, foreign bodies, or external tumor compression. Recurrent inflammatory processes cause progressive destruction of the acini with replacement of the gland by fibrous tissue.
In a patient with chronic sialadenitis, it is necessary to collect an anamnesis, conduct a physical examination and, possibly, imaging tests, and begin treatment of the primary etiology. Patients typically present with recurrent or mild swelling and tenderness of the affected gland, especially while eating.
During a physical examination, enlargement of the gland can be detected in the initial stages, which may subside in the later stages of the disease. Using massage in the direction of the opening of the duct, it is not always possible to obtain a significant amount of saliva. During the examination, attention should be paid to the etiological factor - stone or stricture. If the etiological factor cannot be established, treatment is conservative and includes drugs that promote salivary secretion, massage of the gland, adequate hydration and anti-inflammatory drugs. In severe cases, the gland is removed.
Sialolithiasis ICD K11.5
Caused by the formation of stones in the ducts of the salivary gland. The submandibular gland is most often affected (80-90% of all cases), and almost all other cases occur in the parotid gland. The stones are composed of salts and proteins, mainly calcium carbonate.
Patients usually complain of pain and swelling of the salivary gland after eating. The history contains evidence of relapses of acute purulent sialadenitis. During bimanual palpation along the duct, a stone can be detected. To visualize the stone, ultrasound or CT without contrast is necessary.
Initial therapy includes treatment of acute infection followed by surgical removal of the stone. Access to the duct depends on the location of the stone. Submandibular stones, which are palpable and located at the front of the floor of the mouth, can be removed from the side of the mouth, usually under local anesthesia. If the submandibular stone is located at the hilum of the gland, the entire gland may need to be removed. Stones from the parotid gland are technically more difficult to remove, so a parotidectomy is often necessary. An alternative to open surgery is sialendoscopy, during which a thin (0.8-1.6 mm) endoscope is inserted into the strait of the salivary gland; it can be used to remove the stone. The results of several studies have shown the advantage of endoscopy over open surgery for getting rid of stones and the disappearance of symptoms.
Salivary duct stone removed by endoscopic surgery.
Parotitis
The most common cause of non-purulent acute sialadenitis; 85% of cases occur in children under 15 years of age. The infection is highly contagious and spreads through airborne droplets with secretions from the salivary glands, nasal cavity and urinary tract. Mumps is manifested by local pain and swelling, ear pain and trismus are possible. In most cases, both glands are affected, although the infection usually begins on one side. The diagnosis can be confirmed serologically.
Treatment is supportive care including adequate hydration, oral hygiene, and pain management. The swelling usually goes away within a few weeks. Vaccinations completed before 4 to 6 years of age are 88% effective in preventing infection and reduce disease incidence by 99%.
Human immunodeficiency virus ICD B20
Salivary gland disease associated with HIV manifests itself as diffuse, gradual, painless cystic enlargement of the large glands (the parotid gland is most often affected). These lymphoepithelial cysts may be the initial manifestation of infection or appear in later stages. The patient may experience decreased saliva production, leading to xerostomia, which may resemble Schoengren's syndrome. Using imaging techniques, multiple cysts of reduced echogenicity and diffuse lymphadenopathy can be detected.
Treatment includes antiviral medications, oral hygiene, and medications that increase saliva production.
Benign tumors
Benign salivary gland tumors usually appear as painless, asymptomatic masses in the neck or parotid area and grow slowly. Common salivary gland tumors in children include hemangiomas, malformations of the lymphatic system, and pleomorphic adenoma. However, more than 50% of salivary gland tumors in children are malignant. A common tumor of the salivary gland in adults is pleomorphic adenoma.
To verify the diagnosis, a fine needle biopsy, ultrasound, CT or MRI is required. Some tumors, especially pleomorphic adenomas, may develop malignancy over time, so these radiation-resistant tumors are usually removed surgically. To confirm the diagnosis and reduce morbidity and mortality, salivary gland tumors should be completely removed.
Malignant tumors
Malignant tumors of the salivary gland are relatively rare; Thus, according to a population study, only 16% of tumors were malignant. Most tumors of the parotid gland are benign, but tumors of the submandibular and sublingual glands are more often malignant. During the initial examination, it is difficult to differentiate a benign tumor from a malignant one until a biopsy is performed. Both types of tumors look like painless mass formations in the gland.
The following symptoms are more typical for malignant tumors: pain, paresis of the facial nerve, fixation of the tumor to the skin or surrounding tissues, palpable cervical lymphadenopathy. In patients who seek medical attention for painless facial muscle weakness, physical and imaging examinations of the parotid gland should be performed. If a tumor is diagnosed, the patient should be referred to an ENT specialist.
Malignant tumor of the parotid gland with fixation and inflammation of the surrounding skin
Initial examination includes contrast-enhanced CT and/or MRI and fine needle aspiration biopsy. Often malignant tumors of the salivary glands are mucoepidermoid and adenoid cystic carcinoma. Less commonly, squamous cell carcinoma of the face or scalp may begin to metastasize to the parotid gland. In most cases, malignant tumors of the salivary glands are treated surgically, therefore, if suspected, the patient should be referred to a specialist as soon as possible.
Indications for referral to a specialist for patients with suspected malignant tumor of the salivary gland
- Complications from infection (eg, abscess, fistula, neurological cranial nerve deficit)
- Recurrent or chronic symptoms
- A tumor is suspected for biopsy and removal
- Suspicion of salivary gland duct stone
- Swelling or infection that is resistant to treatment
Literature
- Bozzato A, Hertel V, Bumm K, Iro H, Zenk J. Salivary simulation with ascorbic acid enhances sonographic diagnosis of obstructive sialadenitis. J Clin Ultrasound
. 2009;37(6):329–332. - Flint PW, Haughey BH, Lund VJ, et al., eds. Cummings Otolaryngology Head and Neck Surgery. 5th ed. Philadelphia, Pa.: Mosby Elsevier; 2010: 1151–1161.
- Luers JC, Grosheva M, Reifferscheid V, Stenner M, Beutner D. Sialendoscopy for sialolithiasis: early treatment, better outcome. Head Neck
. 2012;34(4):499–504. - Myers EN, Suen JY, Myers JN, Hanna EY, eds. Cancer of the Head and Neck. 4th ed. Philadelphia, Pa.: Saunders; 2003:475–510.
- Pinkston JA, Cole P. Incidence rates of salivary gland tumors: results from a population-based study. Otolaryngol Head Neck Surg
. 1999;120(6):834–840. - Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg
. 1986;8(3):177–184. - Sun EC, Curtis R, Melbye M, Goedert JJ. Salivary gland cancer in the United States. Cancer Epidemiol Biomarkers Prev
. 1999;8(12):1095–1100. - Author: Bogdan Boris
0 0 votes
Article rating
Pathogenesis
There are three pairs of major salivary glands in the human mouth. The parotids are located under the auricle in front and are the largest. The submandibular muscles are located under the lower jaw. Accordingly, sublingual - under the mucous membrane of the floor of the oral cavity on both sides of the tongue. These glands produce saliva, which is produced through ducts located in the oral cavity. Saliva ensures normal digestion by softening solid foods.
Reactive-dystrophic pathological processes occur in stages. At the initial stage , there are no symptoms of the inflammatory process, but the lymph stagnates near the blood vessels and ducts. The vessels become overfilled with blood, the lymph around the gland ducts stagnates, and the connective tissue loosens. The acini (terminal sections of the salivary gland) are completely preserved, and mucopolysaccharides and mucin accumulate in them.
The second stage of the disease is characterized by the presence of signs of an obvious chronic inflammatory process. There are signs of atrophic changes in the end parts of the gland, infiltrates are detected in the sclerotic stroma. Fibrous tissue appears near the excretory ducts of the gland. Lymphocytes and epithelial cells accumulate in the lumen of the ducts.
At the third stage, almost complete atrophy of the gland parenchyma occurs, and it is replaced by connective tissue. Blood vessels dilate, the ducts of the gland dilate or narrow if they are compressed by connective tissue.
Classification
Taking into account the peculiarities of the process, acute and chronic sialadenitis are distinguished.
According to nosological independence, two forms of the disease are distinguished:
- Primary is an independent disease.
- Secondary – a complication in the development of other diseases ( flu , sore throat , etc.).
Taking into account the causes of the development of the disease, the following are distinguished:
- Traumatic – a consequence of injuries and the influence of external factors.
- Radiation – a consequence of irradiation.
- Toxic – a consequence of chemical influence.
- Infectious – develops after infection.
- Allergic.
- Autoimmune.
- Obstructive - a consequence of blockage of the excretory duct by a foreign body or cicatricial narrowing of the duct.
According to the location of the lesion there are:
- Inflammation of the sublingual salivary gland - the inflammatory process of the sublingual gland is also called sublingual gland.
- Inflammation of the parotid salivary gland - in this case, the cheeks swell and there are signs of general intoxication. Sialadenitis of the parotid gland is also called mumps .
- Sialadenitis of the submandibular salivary gland is an inflammatory process of the submandibular salivary gland. When this gland is damaged, calculous sialadenitis , which is characterized by the development of stones in the ducts of the salivary glands or in their parenchyma.
Taking into account the condition of the parenchyma, the following forms of the disease are distinguished:
- interstitial sialadenitis - only stromal damage occurs.
- parenchymal sialadenitis - in addition to the stroma, the parenchyma is also affected.
Depending on the nature of the inflammatory process, the following forms of sialadenitis are distinguished:
- Purulent.
- Serous.
- Hemorrhagic.
- Connective tissue.
- Destructive.
- Granulomatous.
- Fibroplastic.
- Sialadenitis without deformation of the gland.
- Sialadenitis with scarring of the gland.
There are also epidemic and non-epidemic sialadenitis.
- The epidemic form of the disease develops against the background of viral diseases and infections.
- Non-epidemic form - diagnosed if there is a blockage of the salivary gland. Such blockage can develop as a result of injuries, salivary stones, or foreign bodies entering the ducts.
Causes
There are a number of factors that provoke the development of sialadenitis:
- Wrong approach to oral hygiene.
- Diseases in which the composition and viscosity of saliva changes.
- Postponed surgeries.
- Infectious diseases - influenza, encephalitis , herpes , ARVI , etc.
- Oral diseases – caries , pulpitis , periodontitis , etc.
- Dry mouth.
- Treatment with chemotherapy , radiation therapy .
- Diabetes.
- Disorders of mineral metabolism leading to stone formation.
The epidemic type of the disease develops as a result of infectious processes. Most often, this condition develops with mumps (mumps) . This virus is transmitted from infected people through airborne droplets.
The non-epidemic form of the disease is usually associated with blockage of the glands. This happens with injuries or exposure to foreign bodies. Also the cause of the development of this form of the disease is the so-called salivary stone disease ( sialolithiasis ). If a person develops sialolithiasis of the submandibular salivary gland, the resulting stones may block the ducts.
Symptoms of salivary gland inflammation
The signs that inflammation manifests largely depend on where exactly the pathological process is localized.
submandibular sialadenitis develops , symptoms may be as follows:
- Pain in the submandibular area, which becomes worse when chewing.
- Swelling in the area of the salivary gland, which may increase.
- Temperature increase.
- Taste of salt or pus.
- Swelling of the face.
- Redness and swelling in the mouth.
If sialadenitis of the sublingual salivary gland , similar symptoms develop. The mouth of the exit ducts of the gland turns red and swelling develops. The pain may be more severe than with submandibular sialadenitis .
With parotid sialadenitis, more pronounced symptoms appear. There is marked swelling and asymmetry of the face, redness of the skin. The patient is bothered by dry mouth. The pain intensifies when palpating the affected area. The temperature rises and the general condition worsens. Shortness of breath may bother you . Palpation of the parotid salivary gland leads to the appearance of cloudy saliva mixed with pus.
Symptoms of salivary stone disease can manifest themselves in a similar way. I am concerned about soreness and dry mouth. At the same time, it is difficult for a person to open and close his mouth.
Parotid salivary gland cancer (ICD 10) - classification of tumors
All salivary gland tumors are divided into three main groups:
- malignant - sarcoma, adenocarcinoma of the salivary gland, carcinoma of the salivary gland, adenoid cystic carcinoma of the parotid gland, as well as metastatic and malignant tumors;
- benign – non-epithelial tumors (hemangiomas, chondromas, fibromas, lipomas, salivary gland lymphoma, neuromas) and epithelial (adenomas, adenolymphomas, mixed tumors);
- locally destructive - mucoepidermoid tumor of the parotid salivary gland, cylindroma, acinar cell neoplasms.
Doctors classify the stages of salivary gland cancer according to the TNM system:
- T0 – absence of neoplasm in the salivary gland;
- T1 – the tumor is present, its diameter is less than 2 cm and is not localized only within the gland;
- T2 – tumor diameter up to 4 cm, localization – within the salivary gland;
- T3 – neoplasm with a diameter within 6 cm, does not spread or spreads without affecting the facial nerve;
- T4 – the tumor reaches a diameter of more than 6-7 cm and spreads to the facial nerve and base of the skull;
- N0 – tumor without metastases to local lymph nodes;
- N1 – metastasis occurs in one adjacent lymph node;
- N2 – metastases are present in several lymph nodes, diameter – up to 6 cm;
- N3 – metastases affect several lymph nodes with a diameter of more than 6-7 cm;
- M0 – no distant metastases;
- M1 – distant metastases are present.
The stages of cancer are determined through a series of diagnostic measures that allow a comprehensive study of the tumor process and selection of the most appropriate treatment.
Tests and diagnosis of sialadenitis
Diagnosis of sialadenitis is carried out using clinical, instrumental and laboratory methods.
The essence of clinical methods is the collection of complaints and anamnesis. The doctor also examines the patient.
Laboratory methods - a general blood and urine test, a biochemical blood test are performed. A study of saliva is also carried out, in which, during the inflammatory process, leukocytes and an admixture of pus are found.
Hardware methods - diagnosis of diseases of the salivary glands involves, first of all, sialography with contrast, that is, x-rays of the gland. With the help of such a study, stones, narrowing of the lumen of the excretory duct, as well as other obstacles to the normal secretion of saliva are determined.
CT, MRI - it is advisable to carry out if the presence of stones is suspected.
Ultrasound - allows you to determine the structure of the gland and the characteristics of the inflammatory process.
Thermosialography – the temperature of the gland is measured.
Salivary gland biopsy - performed under ultrasound guidance.
Sialendoscopy.
Diagnosis of sialadenitis
Diagnosis involves a thorough analysis of the patient’s complaints, as well as palpation of the salivary gland. To clarify the diagnosis, cytological studies of salivary secretions are possible. , radiography with a contrast agent may be prescribed . The purpose of the study is to evaluate the gland tissue and the patency of the salivary ducts. X-rays are performed only after acute inflammation has been eliminated. The goal of diagnosis is to differentiate chronic sialadenitis from other diseases with similar symptoms:
- acute bacterial or viral sialadenitis;
- benign neoplasms;
- Herzenberg's pseudomumps;
- sialadenosis.
Treatment with folk remedies
Traditional methods in the treatment process can only be used as auxiliary ones. It is advisable to use the following methods of traditional treatment:
- Rinsing the mouth - for this purpose, a solution of soda and salt can be used (1 teaspoon of salt and soda for 1 glass of water). It is also recommended to rinse the mouth with infusions of herbs - sage, oak bark, calendula, chamomile. To prepare the infusion for rinsing, 2 tbsp. l. raw materials should be poured into 3 liters. boiling water Leave for an hour and rinse your mouth several times a day. In case of purulent processes, rinsing is contraindicated.
- To stimulate salivation, it is recommended to consume lemon juice, cranberry juice, and chewing candies.
- 5 tbsp. l. pine needles pour 1 liter of water, bring to a boil, leave and take 50 ml 2 times a day.
Tumor of the parotid salivary gland: treatment without surgery at the Yusupov Hospital
The prognosis for a salivary gland tumor entirely depends on the individual clinical picture of the patient. As a rule, it is more favorable for women.
Benign neoplasms are subject to surgical removal. Surgery for tumors of the parotid glands is associated with the risk of trauma to the facial nerve, therefore, both the surgical process and the rehabilitation period require careful monitoring by an oncologist. Possible postoperative complications are paralysis or paresis of facial muscles, as well as the occurrence of postoperative fistulas.
Salivary gland cancer most often involves combined treatment - surgery together with radiation therapy. Chemotherapy for tumors of the salivary glands is used extremely rarely due to the fact that in this case it is ineffective.
The treatment of salivary gland cancer at the Yusupov Hospital is carried out by experienced oncologists, whose professionalism has been repeatedly confirmed by international certificates and diplomas. Our doctors annually undergo advanced training courses, which allows them to use only the most modern and effective techniques in medical practice. The drugs used in the hospital or prescribed during treatment are safe and most effective.
To make an appointment with an oncologist at the Yusupov Hospital, you should call or write to the coordinating doctor on our website.
Diet
Diet to boost immunity
- Efficacy: therapeutic effect after 3 weeks
- Terms: 1-3 months or more
- Cost of products: 1600-1800 rubles. in Week
During the treatment period, it is recommended to eat properly to strengthen the immune system. Sometimes doctors advise sticking to the so-called salivary diet. However, if a patient is diagnosed with calculous sialadenitis, then in this case it is necessary to carry out mechanical removal of stones, since nutritional correction will not help cure the calculous type of disease.
The salivary diet involves introducing the following products into the menu:
- Sauerkraut, sour berry fruit drinks, lemon juice, pickles.
- Citrus.
- Sour lollipops.
- Fresh vegetables.
- Juices from cabbage, carrots.
- Rose hip decoction.
You need to exclude from your diet foods that contribute to the formation of stones:
- Cheeses, cottage cheese.
- Tofu.
- Almonds, sesame.
- Fish.
- Milk.