Botulinum toxin type A preparations are better known in our country as Botox and are firmly associated with getting rid of early wrinkles. But there are a number of inaccuracies here. Firstly, Botox is not a group of drugs or an active substance, but a trade name for a very specific drug, which, nevertheless, has become a household name, that is, it is used to refer to all similar drugs in general. And secondly, the range of tasks for such tools is much wider!
What are the advantages of botulinum therapy with Botulax in the treatment of bruxism?
- Myorelaxation Complete relaxation of tight masticatory muscles and elimination of painful spasm.
- Long-lasting effect After one procedure, the relaxing effect lasts for several months.
- Quick relief from pain The drug begins to act immediately and gently relieves stress and discomfort.
- Point effect The medicine is administered to strictly defined points and does not affect the functioning of other facial structures.
- Getting rid of a bad habit You will quietly get out of the habit of clenching your jaw and aggravating the consequences of bruxism.
- Maximum safety The drug does not cause addiction and is completely eliminated from the body.
There is a solution for each case!
1 procedure
1 Botulax procedure Gentle and safe effect For mild cases of hypertonicity of the masticatory muscles RUB 15,000. 15,000 rub.
3 procedures
A course of 3 Botulax procedures Gentle and safe effects For moderate and severe stages of hypertonicity RUB 35,000. 35,000 rub.
Botulinum therapy can help if you have a habit of clenching your jaw tightly and grinding your teeth, you suffer from increased abrasion of enamel and destruction of crowns.
About trismus
Trismus can occur at any time, immediately after or even years after treatment. This condition may occur in the following cases:
- if you have a tumor affecting the bones, muscles and nerves that control the opening of your mouth;
- after surgery on the head and neck organs;
- after radiation therapy in the head and neck area.
Trismus can occur when fibrosis (scarring) develops during the healing process of tissue after surgery. In addition, fibrosis may worsen years after radiotherapy.
If you cannot open your mouth wide enough, it will be difficult for the health care provider to examine your mouth. In this regard, problems may also arise with:
- oral hygiene (keeping the mouth clean and brushing teeth), which can lead to bad breath, tooth decay and oral infections;
- chewing and swallowing, which may make it difficult for you to eat and drink;
- speech;
- kisses;
- insertion of a breathing tube, for example if you ever need general anesthesia (a drug given to keep you asleep during an operation or procedure);
- carrying out routine dental treatment.
When trismus occurs, its treatment is very difficult. This is why it is important to prevent trismus and treat the condition as early as possible.
to come back to the beginning
Symptoms of hypertonicity of the masticatory muscles and bruxism
- the chewing surfaces of the teeth become worn and flat (the cutting edges disappear),
- tooth enamel chips, wedge-shaped defects appear, fillings fly out, teeth quickly decay, become loose, gums hurt,
- you experience discomfort when opening your mouth, while eating or yawning - there are clicks, crunching sounds,
- you or your loved ones notice that you are grinding your teeth - the characteristic grinding appears mainly at night (the so-called “night bruxism”), when it is difficult for a person to control himself during sleep,
- cramps the jaw - you cannot fully open or close your mouth, the jaw seems to be blocked,
- it is difficult for you to keep your mouth open for a long time, overexertion and pain appear during bruxism,
- when talking or chewing, you feel that your facial muscles are “clogged”, tired,
- when you are angry, tense or just working in concentration - your mouth is tightly closed, your lips are pursed, your teeth are closed, you are literally clenching your jaw,
- there are problems with your bite – your teeth don’t fit together correctly, your jaws are misaligned relative to each other, causing you to bite your cheeks or tongue,
- after concentrated work or under stress, you often have a pressing sensation in your temples, pain and dizziness,
- you notice ringing and noise in your ears,
- Over time, the lower half of your face has become visually square, heavy,
- there are problems with posture - you are slouched, your lower back hurts, your neck is stiff, one shoulder is higher than the other.
If you find one or more signs in yourself, then this is a reason to consult a specialist for medical help. And the first step is a comprehensive diagnosis and search for the causes of hypertension.
We approach the treatment of bruxism comprehensively! We carry out in-depth diagnostics, find the exact cause of facial muscle spasm and eliminate it using advanced methods - safely and with high results.
Free consultation
Clinical picture
The first sign of trismus of the jaw muscles is compression of the upper and lower jaws, during which the person cannot make any movements.
Other characteristic symptoms:
- pain when trying to make a movement;
- swelling, compaction;
- limited mobility;
- facial asymmetry (with unilateral spasm).
The pain intensifies when palpated. In some cases, there is an increase in temperature and fever. Unilateral spasm most often occurs as a result of injuries and inflammation of the facial region, bilateral spasm occurs in pathological conditions of the body systems.
Trismus has three forms, which is determined by the degree of limitation of motor functions:
- with a mild form, the mouth may open up to 4 cm;
- with average – up to 2 cm;
- in severe cases - up to 1 cm.
The pathology is often confused with a dislocated jaw or arthritis of the joints, which is associated with similar symptoms, so professional diagnosis is necessary to determine the exact cause of the problem.
The main causes of bruxism in adults and jaw strain
- psycho-emotional reasons: nervous overstrain, prolonged stress, difficult experiences of situations,
- dental reasons: prolonged absence of teeth, malocclusion, diseases of the temporomandibular joint, complete or almost complete absence of teeth, inconvenient and poorly made crowns and dentures, fillings that are too high, injuries to the dental system,
- disorders of the musculoskeletal system: injuries and curvature of the spine, poor posture, asymmetry in the work of the core muscles,
- neurological causes: epilepsy, birth trauma, brain and central nervous system damage,
- other reasons: taking certain medications, smoking, abuse of caffeine-containing drinks.
“We always take a comprehensive approach to solving problems of hypertonicity of facial muscles. First of all, we look for causes from the maxillofacial apparatus - we carry out a full diagnosis and examination, evaluate the functioning of the masticatory muscles, identify the patient’s characteristic habits and collect a medical history. If necessary, we refer the patient to specialized specialists - a neurologist, psychotherapist, etc. It is very important to cure hypertonicity - at least so that the patient in the future can safely begin high-quality dental restoration: implantation, prosthetics or treatment.”
Aida Vladimirovna Jutova, implant surgeon, periodontist, work experience of more than 9 years make an appointment
Diagnostics
Early cases of hemifacial spasm are sometimes difficult to distinguish from facial myokymia, tics or myoclonus, which may be caused by pathological processes in the cerebral cortex or brainstem. In such cases, neurophysiological testing is the most valuable diagnostic method.
Wide and variable synkinesis on eyeblink tests and high-frequency discharges on electromyography (EMG) with associated clinical manifestations are diagnostic criteria for hemifacial spasm. Stimulation of one branch of the facial nerve can spread and cause a response in the muscle innervated by another branch. Synkinesia is absent in essential blepharospasm, dystonia or epilepsy. Needle myography shows irregular, short, high-frequency burst potentials (150-400 Hz) of motor units that correlate with clinically observed facial movements.
Visualization methods
Magnetic resonance imaging is the diagnostic method of choice when there is a need to exclude compression effects. Angiography of the cerebral vessels is generally of little value in the diagnosis of hemifacial spasm. Ecstatic blood vessels are rarely identified, and these vessel findings may be difficult to correlate with nerve effects. Performing angiography and/or magnetic resonance angiography is typically used to perform surgical vascular decompression.
Botulinum therapy as one of the methods for treating hypertension and bruxism
Botulinum toxin type A, which is used in medicine and cosmetology, is able to relieve spasms and relax overstrained muscles, specifically reducing their activity or immobilizing them completely. But not forever, but only for a certain period of time - during this time the body adapts to new circumstances and stops overstraining a certain area. That is, the therapeutic effect for a diagnosis such as “bruxism” lasts for a long time, which is confirmed by numerous reviews from patients.
How it works?
Botulinum toxin type A is a neurotoxin produced by the bacteria Clostridium botulinum. It blocks nerve impulses from the central nervous system to muscle fibers. That is, in fact, the drug paralyzes a certain muscle without transmitting motor commands from the brain to it.
In medicine and cosmetology, it is used in ultra-small and highly purified forms - that is, it is not poisonous or toxic to the body!
The drug is injected into clearly defined points in order to affect only a specific muscle and not affect the work of others. The dosages are harmless, and the blocking is reversible. Over time, the drug is completely eliminated from the body - usually this takes from 5 to 7 months. Gradually, neuromuscular conduction in the area is restored, and mobility returns to the muscle - but since it has “rested,” the spasmodic fibers are smoothed out, and the body adapts and normalizes the load.
Botulinum toxin only relieves hypertonicity and allows the muscle to relax. This is the basis of its well-known cosmetic effect - smoothing out wrinkles by blocking the work of facial muscles. That is, it is wrong to think that you can “pump yourself up” with botulinum toxin preparations - they do not in any way increase the volume of soft tissues.
To relieve excess tension in the masticatory muscles, we use the drug Botulax for intramuscular injection with 99% active substance content, thereby increasing the speed of onset and duration of the therapeutic effect. And thanks to the high degree of purification of the drug, the risk of adverse reactions is minimized. The dosage and course are selected by the doctor strictly individually!
Indications and contraindications for botulinum therapy of masticatory muscles
Indications
- pain in the temporomandibular joint area,
- limited mouth opening,
- clicking, crunching, discomfort when moving the lower jaw,
- pathological abrasion of enamel,
- overstrain of the masticatory muscles, their soreness and heaviness,
- preparation for implantation, classical prosthetics (especially veneers), orthodontic treatment.
Contraindications
- pustular skin lesions, ulcers, acute infection in the area of the masticatory muscles,
- viral and infectious diseases in the acute stage,
- neuromuscular diseases (myasthenia gravis),
- constant use of certain medications and antibiotics,
- pregnancy and lactation period,
- bleeding disorders,
- diabetes,
- allergic reactions to the components of the drug,
- oncology and severe mental disorders.
Symptoms of bruxism and the main causes of hypertonicity:
- the surface of the teeth grinds down, they become flatter;
- the enamel is damaged, fillings fall out, teeth begin to loosen, their integrity is violated, the gums become raw and bleed;
- crunching and clicking appears in the jaw when opening and chewing;
- teeth grinding occurs when a person sleeps;
- it is difficult to open and close your mouth, you feel tired and overstrained masticatory muscles;
- you often unconsciously clench your jaw, most of the time they are tense;
- malocclusions appear;
- the lower part of the face takes on a square shape;
- posture worsens.
Main stages of treatment
Step 1. Preparation for the procedure
A doctor, for example, an implant surgeon or an orthopedist, may refer you to the botulinum therapy procedure for comprehensive preparation before installing implants or dentures. But you can also contact your dentist yourself with complaints about the symptoms of dental bruxism. On the recommendation of a doctor, after consultation and diagnosis, you can begin the injection course.
No complicated preparation is required. 2-3 days before the procedure, it is advisable to eliminate alcohol and reduce the consumption of tea, coffee and energy drinks, as well as stop taking blood thinning medications and antibiotics.
Experienced doctors who follow safety precautions! Our specialists have undergone appropriate training, are certified and accurately calculate the dosage of the drug. We carry out treatment carefully, safely and with results!
Sign up
Step 2. Administration of the drug
The procedure itself takes on average 20 minutes. The doctor conducts a follow-up examination and marks points for drug administration.
The doctor takes the ampoule out of the refrigerator and opens the disposable syringe with the medicine in front of you - this way you will make sure that the storage conditions and sterility of the drug are observed. How many units of Botox are needed for bruxism? The specialist will calculate the dose individually, based on the severity of the symptoms, and divide it into 3-4 parts - that is, you will be given several small injections in different areas of the muscle. For injections, disposable sterile syringes with thin needles are used, so the procedure is almost painless. But for greater comfort, the injection site can be numbed.
Step 3. Rehabilitation period
The drug begins to act immediately, but gains maximum strength gradually - over about 10-14 days, during which the spasmodic area completely relaxes. At this time, it is undesirable to overheat and overcool the problem area: that is, you will have to limit physical activity, trips to the bathhouse and sauna, as well as to the pool.
It is also important in the first days to touch your face as little as possible and not to steam or massage the injection sites.
The effect of the drug lasts up to 7 months, but may weaken faster depending on individual characteristics. Your doctor will tell you at your follow-up appointment whether you need a repeat course.
Symptoms and manifestations
Trismus of the masticatory muscles is accompanied by limited mobility of the joints responsible for closing the jaw. The inability to unclench them can be of a different nature - from partial to complete immobilization. The mouth may open 40, 20, or 10 mm or less, depending on the severity of the condition. Spasmodic contractions can worsen your overall health, cause headaches and other consequences.
One of the manifestations is inflammatory processes due to jamming of the jaws, in this case there is an alternating reduction of the sides of the face. Less commonly, trismus is associated with tumor processes, accompanied by a noticeable increase in formation and increased symptoms. With viral infections, elevated body temperature is often observed.
Disadvantages of treating bruxism with Botulax
It is important to choose an experienced, certified doctor who has trained and has official approval for botulinum toxin injection therapy - this is a rather complex procedure with its own subtleties. If the rules of storage, selection of dosage and administration technique are not followed, complications may occur. And if hematomas, bruises or slight swelling basically go away on their own, then difficulties with swallowing and chewing should be eliminated together with a doctor.
Our doctors have been trained and certified - treating hypertonicity with botulinum therapy in our clinic is completely safe
Why is botulinum therapy not enough to eliminate hypertension?
You need to understand that Botox treatment in dentistry, like orthopedic treatment of bruxism (that is, the manufacture of special protective mouth guards for teeth during bruxism), is only an additional, and not an independent method. Botulinum therapy protects against the consequences of muscle strain - that is, visible relief will actually occur after administration of the drug. The spasm will go away, the muscles will relax, you will stop involuntarily clenching your jaw and thereby injuring your teeth. But as soon as the effect of botulinum toxin wears off, the problem may return, albeit to a lesser extent.
Of course, if it was just a formed habit based on nervousness, and the causes of bruxism are psychosomatic or neurological, then during treatment you have a good chance to completely get rid of it. But if the source lies in other pathologies and disorders, then you also need to address them: take care of your posture, solve bite problems, restore damaged teeth, replace low-quality dentures, etc. And botulinum therapy will become an effective comprehensive measure.
Why are mouthguards needed for bruxism?
Another additional way to treat hypertonicity of the masticatory muscles in adults is to wear a special protective mouth guard (they are also called a “mouth guard” or “bruxism trainer”). These are plastic and dense overlays for teeth, which are worn mainly at night, and in case of severe symptoms, worn during the day. They are made from hypoallergenic materials in a dental laboratory individually for the patient or at the factory, if we are talking about mass production.
But this is also an auxiliary measure - a mouth guard helps muscles relax, protects against tooth wear and the consequences of bruxism, but does not remove the cause of hypertonicity.
- protection of enamel from cracks, chips, increased abrasion due to involuntary clenching of teeth,
- protection of artificial crowns, dentures (including those on implants) or brace systems from damage,
- relieving tension and pain in masticatory muscles and joints,
- protection against movement and displacement of teeth due to constant pressure on them,
- gradual return of the jaws and joints to the correct position in the event of their displacement (of course, only individual mouthguards for bruxism made by a doctor work this way).
How to prevent trismus
There are 4 main ways to prevent trismus:
- massage your jaw muscles;
- train your jaw muscles;
- maintain good posture;
- Maintain proper oral hygiene.
This should be done even if there are no symptoms of trismus to prevent it. Follow the directions in the section below. If you have had surgery, ask your healthcare provider if it is safe before you have surgery.
You may need a timer or watch to help you hold the stretching position for the required amount of time. Breathe normally and do not hold your breath. If you feel pain, numbness, or tingling, stop immediately and call your healthcare provider.
Massage your jaw muscles
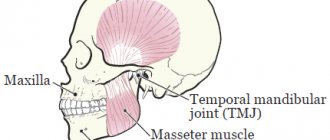
Press your index and middle fingers against your cheekbone. Use your fingers to massage the masseter muscle, which is attached to the lower jaw (see Figure 3). As you move your fingers, look for areas that are tender or tight. Massage these areas with circular movements of your fingers for 30 seconds. Do this 2-3 times a day.
Try not to clench your jaw when you are stressed or out of habit. This will help relax your jaw muscles.
Figure 3. Massage the jaw muscles
Train your jaw muscles
Perform these exercises 3 times every day. You can do them standing or sitting. Use a mirror to help you do the exercises correctly.
These exercises will help stretch the muscles well, but should not cause pain. If an exercise causes pain or discomfort, try doing it with less effort. If pain or discomfort persists, contact your healthcare provider.
Range of motion and stretching exercises
Your head should remain in one position while performing these exercises. Repeat these steps 5 times.
- Open your mouth as wide as possible until you feel a good stretch but no pain (see Figure 4).
Hold this position for 10 seconds. Figure 4. Opening your mouth as wide as possible - Move your lower jaw to the left (see Figure 5). Hold this position for 3 seconds.
- Move your lower jaw to the right (see Figure 6). Hold this position for 3 seconds.
Figure 5. Jaw shift to the leftFigure 6. Jaw shift to the right
- Make circular movements with your lower jaw to the left.
- Make circular movements with your lower jaw to the right.
Passive stretching exercise
Figure 7. Press your thumb and index finger against your teeth.
Repeat these steps 5 times.
- Press your thumb against your upper teeth in the middle of your jaw.
- Press the index finger of your other hand against your lower teeth in the middle of your jaw (see Figure 7).
- Open your mouth as wide as possible. Place additional emphasis with your fingers so that your mouth does not close. You should feel a slight stretch, but not pain. Hold this position for ______ seconds.
Maintain proper posture
Correct posture means sitting and standing with your ears, shoulders, hips, knees and ankles aligned horizontally (see Figure 8). To have correct posture, it is necessary to maintain good tone and stretch in the muscles of the neck and shoulders. The following exercises will help you with this.
Figure 8. Correct posture
Do them 2 times every day. You can do them standing or sitting with your arms at your side.
Neck stretch
Repeat these steps 5 times. Hold each stretch for 30 seconds.
- Tilt your head forward (see Figure 9).
- Tilt your head back (see Figure 10).
Figure 9. Head tilt forwardFigure 10. Head tilt back
- Turn your head to the right (see Figure 11).
- Turn your head to the left (see Figure 12).
Figure 11. Turning the head to the rightFigure 12. Turning the head to the left
- Tilt your head, trying to bring your left ear closer to your left shoulder (see Figure 13).
- Tilt your head, trying to bring your right ear closer to your right shoulder (see Figure 14).
Figure 13. Head tilt to the leftFigure 14. Head tilt to the right
Chin retraction
Figure 15. Retraction of the chin when pulling the head back.
Repeat these steps 5 times.
- Looking forward, tuck your chin.
- Pull your head back so that your ears are level with your shoulders (see Figure 15). Stay in this position for 3 seconds.
Scapula compression
Repeat these steps 5 times.
- Tuck your chin in as described in the exercise above.
- Squeeze and squeeze your shoulder blades together as hard as possible (see Figure 16).
- Stay in this position for 3 seconds.
Figure 16. Squeezing the shoulder blades together
Maintain proper oral hygiene
- Brush your teeth and tongue in the morning after sleep, after every meal and before bed.
- If you have removable dentures, remove and clean them every time you brush your teeth. Don't go to bed with dentures in your mouth.
- Floss your teeth once a day before bed.
to come back to the beginning
Choosing a sleep guard for bruxism: types and price
Firstly, there are universal and individual options: finished products are produced in factories using standard templates, and custom-made mouth guards are made exactly to your measurements.
Also, as we mentioned, mouthguards are not only night guards. The vast majority of patients suffer from teeth grinding during sleep, but a number of people cannot control jaw clenching during the day - for such cases, there are options for daytime overlays that are more invisible and do not affect pronunciation.
A mouthguard for teeth against bruxism, especially a night guard, can be bought at a pharmacy (either in Moscow or in any other city). It costs about two to three times less than a custom-made one. The quality depends on the manufacturer, and universal options have limitations in size and shape, so they simply may not fit the dentition. But the most important limitation, which patients often forget about, is that a ready-made onlay should be purchased on the recommendation of a dentist, and not self-medicated. Alas, without diagnosing and searching for the causes of spasm of the masticatory muscles, a ready-made mouth guard will do more harm than good.
Therefore, it is better if the mouth guard is made individually - based on a cast of your jaws. Individual mouthguards for bruxism, made for sleep, take into account anatomical features to the smallest detail and do not overload the teeth. And if you need to wear the veneer during the day, then it should match the shape of the teeth so that it is truly invisible when communicating. You can order such a mouthguard for bruxism in dentistry by contacting your doctor about this problem.
The doctor will also give recommendations on how long a day it is best to wear a mouth guard, how to care for it, and when the product should be replaced.
What happens if hypertonicity of the masticatory muscles is not treated?
The masseter muscle, which moves the lower jaw, is the most powerful in the group of facial muscles. By contracting, it is capable of creating a force of up to 80-100 kg (compare - in order to chew food efficiently, we use barely 10% of this force).
Chronic spasm and overstrain of such strong masticatory muscles creates excess pressure on the teeth, periodontal tissues and temporomandibular joints. From here, many unpleasant consequences for the jaw system and health in general develop along the chain:
- abrasion of enamel and reduction in tooth height,
- chips and cracks, various enamel defects,
- frequent caries,
- overload of periodontal tissues and the development of gum diseases - in particular, dangerous periodontitis,
- failure of fillings, crowns and dentures,
- threat to implants, the possibility of their overload and loosening,
- swelling and inflammation of the masticatory muscles,
- dysfunction of the temporomandibular joint, pain and discomfort when chewing,
- deterioration of blood circulation and tissue nutrition in the area of muscle spasm,
- increased headaches, dizziness, noise and pain in the ears,
- overstrain of the neck and back muscles, development of posture problems,
- violation of facial aesthetics: angular jaw, deep wrinkles around the nose and lips, haggard face and reduction of the lower third.
Correction of bite by treatment of dysfunction of the temporomandibular joint
We usually don't think about how our jaw moves. When most people talk about bite, they mean teeth. But, as mentioned above, the bite is an entire system that controls the position of the jaw. Here are its components and their role:
The role of muscles
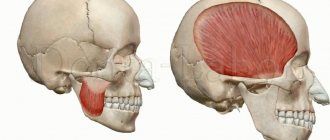
Figure No. 4 Opening, closing the mouth, chewing and swallowing occurs due to the work of a large number of muscles.
The opening of the mouth is ensured by the muscles located in the neck. The muscles that support the mandible are located behind the jaw and run under the cheeks to the frontal and postauricular areas.
The most powerful muscles responsible for chewing are located in the cheek area.
Figure No. 5 Our body strives to carry out all functions with the greatest rationality and the least amount of energy. Therefore, normally, the chewing muscles hold the jaw in a position in which the teeth are separated by 1-2 mm.
Figure No. 6 From this rational position, the lower jaw moves hundreds of times a day until the teeth close to swallow.
All this happens subconsciously. Our brains are hardwired for a process called proprioception.
With proper bite and jaw position at rest, most muscles are in a relaxed state.
If your teeth don't close quite correctly, your muscles can adjust, causing your jaw to close in a pattern that causes excessive tension, spasm, and muscle fatigue over time.
In this case, the position of physiological rest of the lower jaw (when the teeth are not closed) is not accompanied by muscle relaxation, as it should be with normal occlusion, but, on the contrary, leads to their constant tension.
The role of joints
Figure No. 7 The lower jaw moves thanks to the joints. called the temporomandibular joints, or TMJs.
Think of the joint as a ball in a basket - the articular head (ball) moves in the recess of the skull (basket). Between them there is a soft tissue layer (articular disc).
The position of the articular head (condyle) in the corresponding depression of the skull (fossa) is largely determined by the bite (occlusion) - the position where the muscles hold the jaw.
Figure No. 8 If the system is balanced, the condyles are located in the center of the glenoid fossa and the disc, located between the articular head and the glenoid fossa, moves freely in the joint when opening and closing the mouth.
Figure No. 9 If the masticatory muscles adapt to the incorrect position of the jaw, they can hold the head of the joint in a displaced position, negatively affecting its function. This often causes the articular disc to become dislodged, preventing it from moving normally in the joint until it moves completely into its normal position when the mouth opens. When this happens, a clicking sound occurs.
The intensity of the click can vary from a barely perceptible vibration to a very loud sound.
This sound is often a sign of abnormal joint function, which in turn may be associated with a malocclusion.
The role of posture
Posture also plays a significant role in occlusion. The mandible and lower limbs can be considered interdependent parts of the human skeletal system. If any of these parts are negatively affected, other parts of the skeleton may be affected.
Let's check this by slightly closing our teeth. Pay attention to which teeth closed first. Then tilt your head back as much as possible and clench your teeth again. Don't be surprised if the first contact is on other teeth this time. By changing the position of your head, you thereby influence the balance of the entire skeletal system (and your bite in particular).
The same thing happens when you get a filling. Lying in the dental chair under anesthesia, it seems that the filling is not in the way. But after the anesthesia wears off and you get up from the chair, you notice that the filling is higher than the rest of your teeth. This is why in neuromuscular dentistry, the bite is assessed in the sitting position - the position in which your jaw is normally located. If you evaluate the bite in a sitting position, leaning back, the jaw also moves posteriorly. This situation is different from the usual one.
Photo No. 10,11 In an experiment on rats, an oversized filling was made on one lateral tooth on the right side. A week later, an x-ray examination revealed deformation of the entire spine. After leveling the occlusion by making a filling on the lateral tooth on the left, the shape of the spine was restored.
Figure 12 Since there is a direct connection between all parts of the musculoskeletal system, head position undoubtedly affects occlusion, and can cause tension in the neck and back muscles. Figure No. 13 When the lower jaw moves back as a result of malocclusion in childhood or wear of teeth over time, the neck moves forward and the head is thrown back. This, in turn, significantly increases the load on the muscles of the neck and shoulder girdle. Therefore, most people with an anterior head position experience neck pain or neck muscle tension. Figure No. 14, 15 Often, displacement of the lower jaw due to malocclusion is accompanied by rotation of the first and second cervical vertebrae, which leads to severe deformation of the entire cervical spine.
Just as changes in jaw position can cause changes in posture and lead to pathology in the cervical spine, changes in the spine can affect jaw position and occlusion.
The role of breathing and sleep apnea
Figure No. 16 Displacement of the lower jaw back often leads to a narrowing of the airway due to deformation of the cervical spine and posterior displacement of the tongue, which follows the lower jaw. In order to increase the clearance of the airways, the muscles move the neck further forward and tilt the head back.
In this case, the artery that carries blood to the brain along the spine can sharply bend in the area of the first and second cervical vertebrae, causing disturbances in the blood supply to the brain.
Narrowing of the airways and impaired blood supply can cause sleep apnea - a short-term cessation of breathing during sleep.
Repeated stops in breathing lead to a significant change in the metabolism of the entire body and, as a result, can become one of the triggers for diseases such as hypertension, diabetes, myocardial infarction, stroke, etc. Therefore, the untreated condition of sleep apnea is responsible for reducing life expectancy by 20%.
Now you understand that occlusion is much more complex than just the way the teeth are closed! And malocclusion can cause not only early tooth loss, but also cause serious pathologies such as diabetes and myocardial infarction and even reduce life expectancy.
Is it possible to undergo implantation for bruxism?
Only on condition that an integrated approach is applied to implantation and subsequent installation of the prosthesis. In order for your new teeth to serve you for a long time, we carefully plan the entire course of treatment from start to finish: we conduct in-depth diagnostics, identify related problems that may affect the result, take measures to eliminate them, and step by step work through the entire course of the operation and prosthetics.
For example, our patients often experience bruxism and problems with the temporomandibular joints due to the fact that the dental system has not been working properly for a very long time - the teeth were destroyed, the load was distributed unevenly. In itself, the return of all teeth through complex implantation is already a treatment for such conditions, since we think over dentures taking into account the correct functioning of muscles and joints, normal closure of the dentition, etc. But the body will need time to adjust to normal functioning. And that is why in cases of bruxism we are taking additional measures - increasing the number of implants installed for the entire jaw, making prostheses reinforced with a frame and made from more durable materials, and making protective soft mouth guards.
But if bruxism in adults cannot be cured only by dental methods, since the problem is not with the jaw system, but with the same psychosomatics, then we refer the patient for treatment to a specialized specialist - and return to dental restoration afterwards. We care about your health and do everything to ensure that the achieved treatment results last not just for a couple of years, but throughout your entire life.
Primary treatment of pain in temporomandibular joint disorders
An important part of dental treatment is monitoring, diagnosing and treating pain, as well as relieving the underlying causes of pain. However, most dental patients with symptoms of unexplained pain often succumb to inappropriate diagnosis, resulting in misdiagnosis and ineffective treatment. As a result, the patient not only continues to suffer from chronic pain, but also becomes disillusioned with the dental treatment provided.
Pain in the maxillofacial area
By definition, pain in the maxillofacial area (orofacial pain) is associated with localization in the soft and hard tissues of the head, face and neck. With painful stimulation of these zones, through the structure of the trigeminal nerve, impulses reach the corresponding centers of the brain. In the brain, such signals are interpreted “as unpleasant sensory or emotional sensations that arise as a result of actual or potential tissue damage.” The density of tissue in the affected area greatly complicates the procedure for making a correct diagnosis. Quite often, patients describe the location of the toothache away from the actual site of the lesion. The phenomenon of referred pain is based on the interweaving of many sensitive nerve endings that are directed to the nucleus of the trigeminal nerve from the skin and deep tissues of the head and neck.
Toothache is one of the most common forms of pain in the maxillofacial area. The next most frequently reported pain is pain due to dysfunction of the temporomandibular joint (TMJ) and headaches. Often the patient may experience pain of several etiologies at once. The difficulty of diagnosing the main source of pain is also associated with the possible concomitant development of fibromyalgia, chronic fatigue syndrome, or other pathological conditions. In such cases, the best way to make a diagnosis is to use the principle of “peeling the onion” - verifying changes in symptoms one by one.
Temporomandibular joint
The temporomandibular joint (TMJ) is a complex joint that allows for both rotational and gliding movements of the mandible. Structurally, it consists of the condyle of the lower jaw, which in shape corresponds to the articular fossa of the temporal bone. The articular disc is made of dense fibrous cartilage and prevents direct contact between bone surfaces. The anterior part of the disc lacks blood vessels and nerve endings, while the posterior part, on the contrary, is characterized by an abundance of these structures. The joint is lubricated by a special synovial fluid contained in its composition. The movements of the TMJ are ensured by the masticatory muscles. Another main type of muscle that is not involved in the development of TMJ movements, but is responsible for demonstrating emotions, is the facial muscles. The complex of masticatory muscles includes the masticatory muscles themselves, the temporal muscles, the medial pterygoid muscles and the lateral pterygoid muscles.
Temporomandibular joint disorders
Temporomandibular joint disorders are a group of musculoskeletal and neuromuscular diseases that primarily negatively affect the function of the joint itself, the masticatory muscles, or the articular disc. The possibility of TMJ disorders should be taken into account when carrying out the differential diagnosis of facial pain, since TMJ dysfunctions are the most common cause of pain in the area of the dentofacial apparatus of non-odontogenic etiology. To make a correct diagnosis, you should carefully study the patient's medical history, taking into account the onset and duration of pain, as well as the effects of factors associated with relief or worsening of pain. Along with constant pain in the jaw projection, patients often complain of ear pain, headache and diffuse facial pain. In addition, they may complain of radiating pain or a feeling of stiffness in the face, jaw or neck, associated with restrictions in jaw movement, painful clicking or cracking sounds when closing or opening the mouth. Patients may also indicate changes in the nature of the relationship of teeth with each other. The above symptoms may be especially severe early in the morning, or worsen throughout the day. The threshold, localization, pain sensitivity and the nature of the description of pain sensations differ in different patients, and if we also take into account the complex mechanism of formation of the pain impulse, then one thing becomes obvious - diagnosis is an extremely important stage for the objectification of painful changes. History remains one of the key aspects of a comprehensive diagnosis, helping to detail aspects associated with the development of pain. In addition, during the collection of anamnesis while talking with the patient, the doctor can visually assess the nature of the movements of the lips and jaw, his facial expressions and posture, as well as his emotional status. Historically, occlusal disorders have been considered the primary cause of TMJ dysfunction. However, according to recent studies, these constitute only a small proportion of cases associated with painful joint dysfunction.
There are many classifications of TMJ dysfunctions. In other words, pain due to TMJ dysfunction can be arthrogenic and myogenic. Arthrogenic (joint and disc) dysfunction of the TMJ is usually caused by disc displacement or develops secondary to degenerative changes in the disc, ankylosis, dislocation, infection or neoplasia. Myogenic dysfunctions occur due to muscle hyperactivity or due to bruxism, hypermobility, or external stimuli. Myogenic joint dysfunctions can cause ischemia of the skeletal muscles of the face. Irreversible damage to myocytes develops after 3 hours of the ischemic state and in parallel with progressive microvascular disorders. All this only complements the pathological cycle of the mechanism of development of facial pain. Patients with myogenic dysfunction of the TMJ are characterized by the development of more complex pathological disorders and more severe pain compared to patients with arthrogenic dysfunctions. That is why the main principle of treating joint dysfunction is focused on treating and stopping the hyperactivity of the masticatory muscles.
Myofacial pain syndrome
According to the National Institute of Dental Research, the most common form of TMJ dysfunction is myofacial pain syndrome (MPS). With this chronic inflammatory disease, damage occurs not only to the muscles, but also to the fascia. The root causes of this disorder are repetitive movements, damage to muscle fibers and excessive tension in the ligaments and tendons. Patients themselves often complain of depression and fatigue, and even during a clinical examination, the doctor may notice some changes in their behavior. A differential sign of MPS is the presence of so-called trigger points, the activation of which provokes the development and irradiation of pain to different parts of the head and neck area. Trigger points (photos 1 - 4) are formed in the projection of excessive muscle contraction and dysfunction of one of the components of the biomechanical complex of the head and neck. This type of muscle spasm differs from physiological tension of the entire muscle: due to local excessive contraction, blood flow directly to the area of contraction is stopped, which consequently leads to the development of ischemia. The buildup of waste products and toxins sensitizes the trigger point, essentially causing it to send pain signals to the brain, causing even more contraction. Thus, the mechanism of trigger point formation includes a vicious circle of metabolic crisis. Clinically, trigger points can be identified by analyzing existing signs of the lesion, reproducing symptoms and performing palpation. Deep palpation almost always allows you to identify the main trigger zones. Often, when pressing on the trigger area, the patient may experience muscle twitching.
Photo 1. Trigger points of the masticatory muscle in the projection of the upper musculotendinous junction of the superficial layer and central trigger points of the superficial layer with corresponding patterns of pain spreading to the area of the lower jaw, teeth and gums.
Photo 2. Trigger points of the masseter muscle in the lower part of the superficial layer of tissue with corresponding patterns of pain spreading to the lower jaw and superciliary region.
Photo 3. Trigger points of the masseter muscle in the upper part of the deep tissue layer below the TMJ with corresponding patterns of pain spreading to the ear area.
Photo 4. Trigger points of the temporal muscle and projection of the spread of referred pain.
Masseter muscle
The masticatory muscle is the main muscle of the complex of the entire masticatory musculature. The lower jaw is the only movable part of the skull, the movements of which are ensured precisely by the masticatory muscle. It is located in the parotid region along the posterior edge of the jaw, easily visualized and palpated when the jaws are clenched.
The average person can bite with 150 pounds of force, but a bite force of more than 250 pounds is considered normal. This strength of the masticatory muscle is achieved due to specific biomechanical conditions: its lever arm is much shorter than in other muscles. Given the high activity of the masticatory muscle, its tension is visualized even when a person’s emotional state changes. When tension in the muscle continues for too long a period of time, this provokes the formation of those same trigger zones associated with myofacial pain. When trigger points are located in the projection of the masticatory muscle, the patient may experience pain in the eyes, on the surface of the face, in the structure of the jaw and teeth. According to Simons and colleagues, the trigger mechanism of the masseter muscle may even be responsible for the development of pain and itching in the structure of the ear, as well as the development of tinnitus - an unexplained ringing in the ears. Photos 1-3 show trigger points in the masseter muscle and general pain patterns (shown in red). It must be remembered that the facial nerve is motor and is responsible for the innervation of facial muscles. Therefore, when treating trigger points in the deep layers of the masticatory muscle, it is necessary to take into account the specific anatomy of the facial nerve in the projection of the zygomatic arch.
Temporalis muscle
The temporalis muscle is a large, thin, fan-shaped muscle located on the side of the skull above and in front of the ear. Although the masseter muscle is considered the most powerful, the temporalis muscle also plays an important role in the chewing process. It originates from the temporal bone of the skull and passes completely under the zygomatic arch (cheekbone), attaching to the lower jaw, thus assisting the masseter muscle in closing the jaw and retracting it. By placing your fingers just above your ear, squeezing and unclenching your jaw, you can feel the biomechanics of the temporal muscle. Photo 4 shows how strongly trigger points in the temporalis muscle are associated with the possibility of developing pain in the projection of the upper teeth, head, cheeks, eyes and ears. Often, when the nature of pain is incorrectly diagnosed, doctors resort to endodontic treatment, although such treatment may be completely non-odontogenic in nature.
Treatment with botulinum neurotoxin type A
Considering the basic principle of “do no harm,” the treatment of myofacial pain should be carried out through the implementation of non-invasive and reversible intervention methods. To relieve TMJ dysfunction, various palliative approaches and combinations thereof can be used, which include, but are not limited to, splint therapy, massage, physiotherapy, biofeedback, acupuncture, chiropractic, the use of ethyl chloride sprays and stretches, the use of antidepressants, narcotic and non-steroidal anti-inflammatory drugs. In addition, botulinum neurotoxin type A (BoNT-A), which is widely used in cosmetics (Botox, Dysport, Xeomin), and which has been previously approved by the US Food and Drug Administration (FDA) for the treatment of painful conditions potentially associated with disorders in the TMJ area (dystonia of the neck muscles, migraine, etc.). BoNT-A is an injectable pharmaceutical agent that is derived from the bacterium Clostridium botulinum. In small doses, this purified protein can be used to achieve selective skeletal muscle relaxation as it inhibits the release of acetylcholine at the neuromuscular junction. Consequently, due to this, the muscle will not be able to contract with the same intensity, since the amount of available neurotransmitter is markedly reduced. Constant, sometimes dysfunctional contraction of the masticatory muscles may be the main cause of the formation of trigger points in TMJ-associated disorders associated with myofacial pain syndrome. Treatment of TMJ dysfunctions with BoNT-A lasts for a month, allowing the effect to be achieved for 3-4 months. In this case, the physiological functions of chewing, speech, and swallowing remain unimpaired, but the intensity of pain noticeably decreases. Unlike systemic medications, botulinum toxin acts only locally, allowing relief of both active and latent trigger points. Immediately after the injection, the patient may report immediate pain relief as a “dry needling” effect develops. Although this approach cannot cure the cause of pain dysfunction, the effect of BoNT-A injections becomes more and more durable over time. On the other hand, in cases of resistance to other treatment methods, this approach may represent a successful alternative aimed at relieving existing pain. Dentists who are considering using BoNT-A in their practice as an approach for the management of pain associated with TMJ dysfunction may benefit from specialized training. During the latter, the doctor will be able to become familiar with the anatomy, physiology, pharmacological characteristics, as well as adverse reactions and potential complications associated with the use of botulinum toxin. The average price of a bottle with 100 units of active substance for a doctor is about $600. Before using BoNT-A, it is also necessary to take into account the specifics of local legislation regarding the performance of such manipulations.
Bruxism and Dental Sleep Medicine
Dental parafunction is a habit due to which certain organs of the oral cavity or the dentition do not function correctly. Moreover, it is not associated with the processes of drinking water or food, or with the function of speech. The most common parafunction remains bruxism, clenching and pathological abrasion. All of them can potentially be associated with TMJ dysfunctions. Physiological pressure applied to a tooth ranges from 20–80 psi (0.14 to 0.55 MPa), while with bruxism it can reach 300–3000 psi (2.07–0.55 MPa). 20.7 MPa). It is logical that under such conditions the load on the masticatory muscles increases significantly, and their overload, in turn, leads to the development of myofacial pain syndrome.
Masseter muscle hypertrophy
When examining patients with facial pain syndrome associated with TMJ dysfunction, the dentist often identifies the presence of trigger points in the projection of the masticatory muscle. In addition, such patients may experience such strong hypertrophy of this muscle that it provokes a distortion in the appearance of the face. Hypertrophy of this kind can be treated with the same BoNT-A used according to the injection protocol in cases of TMJ dysfunction. Botulinum toxin injections reduce the intensity of muscle contractions and allow the muscle to relax, eliminating the possibility of clenching the teeth with excessive force. But it should be remembered that the goal of such treatment is not only to relieve pain, but also to normalize the visual shape of the face, the distortion of which was caused by hypertrophy (photo 5-6).
Photo 5. View of a patient with hypertrophy of the masseter muscle before treatment.
Photo 6. View of the patient after treatment of masseter muscle hypertrophy using botulinum toxin.
Obstructive sleep apnea
Obstructive sleep apnea (OAE) occurs when repeated episodes of complete or partial blockage of the upper airway occur during sleep. During an episode of OAE, the diaphragm and chest muscles begin to work harder to open blocked airways and allow air into the lungs. Patients with OAE often experience TMJ dysfunction and signs of nocturnal bruxism. The American Academy of Dental Sleep Medicine classifies sleep bruxism as a movement disorder. To record data on bruxism and OAE, it is advisable to use a home monitoring device. Important indicators are the level of oxygenation, pulse, airway patency, the presence of snoring, the specifics of chest movements and body position during sleep. Once an apnea-hypopnea index score has been recorded in a patient with signs of bruxism, which could potentially indicate the presence of OAE, the dentist should contact the patient's physician for a more detailed diagnosis. If UAE is mild or moderate in severity, a customized intraoral device can be made for the patient, which will prevent tongue retraction and dislocation of the lower jaw, thus ensuring patency of the upper respiratory tract.
Headache
The connection between sleep bruxism, TMJ dysfunction and headaches is well established. Headaches provoke the development of significant discomfort, disruption of normal daily activities and possible further chronification of painful sensations. About 30% of patients with headache suffer from associated functional impairment and do not seek medical help. Patients may describe signs of headache during a history taking during a dental examination.
Tension headaches and migraines
Tension headache (TTH) is the most common form of primary headache, affecting most of the population at least once in their lives. Pain that develops from trigger points in the projection of the masticatory muscle can be either episodic or chronic, and clinically it is quite difficult to differentiate them from migraine pain. Therefore, it is necessary to remember that tension-type headache, as well as TMJ dysfunction, can be characterized by the presence of pain, which is a variant of migraine, although they themselves consist of a migraine-like component. Sometimes there is an overlap of symptoms of several pathologies, which can be interpreted both as diagnostic criteria for TMJ dysfunction and as diagnostic criteria of the International Headache Society. The relationship between TMJ dysfunction and headaches has been described in detail in the literature. Patients with an established diagnosis of tension-type headache or migraine, which can be triggered by temporalis muscle myalgia, may also present with symptoms characteristic of TMJ dysfunction.
On the other hand, patients who have undergone treatment for TMJ dysfunctions also experience a decrease in headache intensity levels. Recent evidence suggests that among patients with signs of vascular pain and migraines, there is an increased prevalence of TMJ dysfunction, since the latter can be interpreted as components of a complex of pain sensations with a specific localization. We should also not forget about the potential role of disorders of the facial nerve and facial muscles, which can also provoke the development of pain.
On October 15, 2010, the FDA approved BoNT-A injections for the prevention of headaches in adults with chronic migraine. The treatment protocol includes selective relaxation of hyperfunctional muscles of mastication or facial expression. The treatment approach is to use the lowest effective dose needed to relieve pain; The dosage of the drug depends on the individual response of each individual patient to the therapy. Again, dentists considering the use of BoNT-A injections are strongly advised to undertake appropriate practical training and follow the principles of existing legislation. However, the mechanism by which BoNT-A relieves migraine pain is not entirely clear. It is believed that botulinum toxin, by turning off muscle tension, reduces the load placed on them, and thus relieves pain associated with bruxism or clenching. However, the release of neuropeptides, especially calcitonin gene-related peptide (CGRP), is considered an integral component of the pathophysiological mechanism of migraine. It was found that BoNT-A not only affects the autonomic nervous system, but also directly reduces the amount of CGRP released by trigeminal neurons. Based on this, it can be assumed that BoNT-A relieves headaches through a direct effect on the central nervous system.
Cervicogenic headaches
Neck pain and neck muscle soreness are common symptoms of primary headaches. The diagnosis of cervicogenic headaches (CHH) refers to cases where the headache develops due to bony structures or soft tissues localized in the neck. The pathophysiology of this condition most likely involves disturbances in one or more muscular, neurogenic, osseous, articular, or vascular structures of the neck. Such lesions are often the result of head or neck trauma, but can develop in the absence of a history of trauma. Clinical signs of CDH may mimic those of primary headache, tension-type headache, and migraine. The diagnosis of CDH can only be made after a thorough history and physical examination. Diagnostic criteria include one or more of the following symptoms: moderate or severe pain in the occipital, frontal, temporal, orbital region of the head, neck and back; intermittent or chronic pain, usually deep and not throbbing; headache triggered by neck movements; or restriction of neck movements. Patients with CDH are usually characterized by a slight forward head tilt. Muscle trigger points are localized in the projection of the suboccipital, cervical and brachial muscles, and with physical or manual stimulation they can provoke the development of headaches in the head area. Studies show that 44.1% of patients with CDH have myofacial pain syndrome associated with TMJ dysfunctions. Moreover, when treating TMJ dysfunctions in patients with CDH, a more effective outcome of pain relief is noted, which allows patients to increase the range of motion of the neck as a whole. Like other pain symptoms associated with myofacial pain syndrome, they also respond well to BoNT-A injections.
conclusions
TMJ dysfunctions are characterized by a set of clinical manifestations that are often painful and lead to limitations in physical activity. However, they are self-limiting and usually respond to conservative treatment, such as BoNT-A injections. The basic principles of treatment are aimed at reducing pain and restoring the range of muscle motion, which helps reduce existing physical limitations and relieve pain of associated etiology. Treatment of TMJ dysfunctions also helps prevent the development of tooth damage and chipped restorations, pathological tooth mobility and periodontal tissue pathologies, which can be associated or caused by bruxism. During the treatment of dysfunctions, some patients manage to simultaneously get rid of night bruxism and relieve chronic pain in the neck and shoulders. If a patient is suspected of having signs of nocturnal bruxism, they should undergo home monitoring for potential obstructive sleep apnea. Despite the generalized nature of pain in the head and neck area, patients with chronic orofacial pain often initially seek help from a dentist. Therefore, the clinician must be theoretically and practically prepared to treat TMJ dysfunctions and relieve associated pain during their daily dental practice.
Authors: Lisa Germain, DDS, MScD Louis Malcmacher, DDS, MAGD
Prevention of bruxism: how to help yourself
By prevention we mean measures that prevent dental hypertonicity and bruxism in adults, because without finding the cause and monitoring a specialist, treating them at home is an unsafe activity, as with any disease. So if you notice alarming symptoms, your first step is to get diagnosed and get a plan to comprehensively eliminate this problem.
You may need the help of several specialists (neurologist, dentist, gastroenterologist, ENT doctor, psychotherapist), because bruxism occurs in different people for very different reasons. You may be prescribed courses of physiotherapy, taking certain medications (for example, magnesium supplements), but all this, of course, is very individual.
Self-help measures are helpful if you discuss them with your doctor. For example, you can do a light relaxing massage against bruxism in the area of the chin and temples. There are also a number of exercises that can help relieve muscle spasms; it is useful to repeat them regularly before bed. Relieve general stress: sleep enough hours, walk more in the fresh air, reduce the amount of coffee and strong tea, take relaxing baths with herbs, avoid anxious situations.
All this will help consolidate the results of complex professional treatment and forget about unpleasant symptoms.