Neuralgia of the glossopharyngeal nerve refers to pathological changes in its functioning due to concomitant diseases in nearby sections. The condition is accompanied by pain, impaired salivation, as well as decreased pharyngeal and palatal reflexes.
To relieve negative symptoms, medication and physiotherapeutic treatment are prescribed. The pathology is rare, mainly among men over 40 years of age.
Development factors
There are two forms of neuralgia:
- primary idiopathic glossopharyngeal;
- secondary (Sicart syndrome).
As a rule, neuralgia is a concomitant disease with various pathologies, for example:
- atherosclerosis with damage to the circulatory system;
- infectious lesions (for example, influenza or tonsillitis);
- intoxication with heavy metals and other harmful substances;
- tonsil injury;
- neoplasms in nearby areas;
- otolaryngological diseases;
- increased muscle pressure on the nerve;
- inflammatory processes in the brain, etc.
Taking into account the primary source, the patient is given conservative or surgical treatment.
Damage to the mandibular nerve
Installation of dental implants in the lower and upper jaw is performed under mandibular anesthesia, which suppresses the sensitivity of nerve endings for 3-5 hours. Numbness in the lower part of the face during this period is considered normal.
Persistent loss of sensation, pain, and uncontrollable salivation suggest injury to the branch of the trigeminal nerve, which runs along the nerve canal of the mandible.
Damage is considered to be injury to one of its bundles:
- Submental: n. mentalis.
- Lingual: n. Lingualis.
- Alveolar: n. alveolaris inferior.
Has a damaging effect:
- stretching;
- compression;
- crushing;
- rupture (partial, absolute).
Injury to nerve bundles when installing an artificial dental root of the lower row leads to a decrease in the sensitivity of the innervated organs. Manifests itself in pain and numbness:
- cheeks, 2/3 tongue;
- teeth, gums;
- lower lip, part of the chin.
Loss of sensitivity of these organs makes it difficult to care for the oral cavity and facial skin, complicates eating, and sometimes disrupts facial expressions.
Clinical picture
The pathology is accompanied by acute pain in the subradicular region of the tongue or one tonsil. The pain can spread to the soft tissues of the palate, ear, pharynx and other organs. Neuralgia has a one-sided short-term course (no more than 3 minutes).
Symptoms intensify while moving the tongue. Against the background of intense pain, the quality of life deteriorates and insomnia appears.
Other characteristic features:
- dryness of the mucous membranes of the oral cavity;
- increased salivation after an attack.
A neurological disorder can enter a stage of exacerbation and remission. Over time, the frequency of attacks increases, and the pain intensifies. Some patients report loss of taste perception.
Anatomy of the trigeminal nerve
The trigeminal nerve (5th pair) is a large mixed (sensory-motor) nerve, consisting of three branches :
- Orbital (n. ophthalmicus).
- Maxillary (n. maxillaris).
- Mandibular (n. mandibularis).
The mandibular ( MF ) is the third branch of the trigeminal, innervating the skin, mucous membranes of the organs of the lower jaw, and the muscles of the lower part of the face. Its location and parameters in the human body are individual and determined by anatomical features. The nerve trunk consists of 30-80 fibers, thickness is in the range of 3.5-7.5 mm, length - 0.5-2.0 cm.
The roots of the mandibular nerve transmit information from the lower part of the face and oral cavity: teeth, gums, tongue, outer part of the ear. Motor - innervate the masticatory and part of the facial muscles.
At the exit from the skull, the LF is divided into two branches:
1. Sensitive ( anterior ) - innervating the mucous membranes and skin:
- cheeks, chin;
- floor of the mouth;
- lower teeth, jaw;
- lower lip, back of tongue;
- salivary glands (sublingual and submandibular);
- parts of the outer ear.
2. Motor ( posterior ) - ensuring coordinated work of muscles:
- chewable;
- maxillohyoid;
- suprahyoid;
- palatal-curtain;
- eardrum.
Diagnostics
First of all, the doctor conducts a survey to determine the symptoms, nature and frequency of attacks. At this stage, it is important to differentiate the pathology from trigeminal neuralgia, which has similar symptoms. When the trigeminal nerve is damaged, the spasm is localized in the periolabial region, and damage to the glossopharyngeal nerve is accompanied by discomfort in the area of the root of the tongue.
To make a diagnosis, a number of clinical studies are carried out:
- orthopantomogram (to detect elongation of the styloid process);
- computed tomography of the brain;
- magnetic resonance imaging of the vascular system.
The patient needs to consult an oncologist to rule out cancer.
Probability of occurrence
The mandibular nerve fascicle is a fragment of the trigeminal nerve. It provides sensitivity to intraoral and facial tissues, and is responsible for contraction of the facial muscles and dentofacial apparatus. The bundle consists of motor and sensory fibers and nuclei.
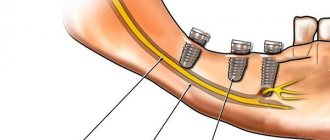
The inferior alveolar nerve (IAN) is located in the lower jaw and is one of the three endings of the trigeminal nerve. The NAN borders the root system of the mandibular arch. In this regard, there is a high risk of damage during dental treatment.
The statistics of nerve damage are especially high during the period when dental operations were performed without the use of modern technologies.
According to the latest data, the incidence of nerve damage during dental implantation does not exceed 3%. Of this number, only 1.7% end up with permanent neuropathy.
According to some dentists, these data are underestimated, and the percentage of damage to NAS reaches 30%. In any case, this issue should be given sufficient attention.
Treatment methods
It is important to consult a doctor immediately after the first characteristic symptoms appear. Timely treatment increases the chances of a full recovery. Neuralgia requires long-term therapy, the tactics of which are determined depending on the clinical condition of the patient and the course of the disease.
Conservative therapy
The patient is prescribed:
- taking non-steroidal anti-inflammatory analgesics;
- antiepileptic drugs;
- neuroleptics;
- muscle relaxants;
- a complex of vitamins and microelements to strengthen the immune system.
If oral administration is ineffective, the patient is prescribed injections of blockades under the tongue. Anesthetics are used for local treatment of the oral cavity. To increase efficiency, physiotherapeutic procedures (for example, exposure to diadynamic and sinusoidal currents, galvanization) are prescribed in combination with drug treatment.
Surgery
The operation is performed to release the compressed nerve. For this purpose, the method of microvascular decompression is used in the area where the nerve process exits the brain. If indicated, it may be necessary to dissect the hypoglossal ligament and shorten the styloid process.
The manipulation is carried out using endoscopic microsurgical equipment, which minimizes the impact on healthy tissue and prevents negative consequences.
Negative consequences may occur after an incorrectly performed intervention (for example, re-infection or injury to the affected area). Timely treatment and compliance with the recommendations of the attending physician increases the chances of a favorable outcome.
Classification
In accordance with Seddon's classification, the following types of NAS injuries are distinguished:
- Neuropraxia. This injury is reversible; the sheath of the nerve fibers does not suffer, that is, there is no development of degeneration. After treatment, the problem goes away, which usually takes a couple of weeks.
- Axonotmesis. A reversible type of lesion, for which long-term, intensive treatment is prescribed - from three to six months. The development of degeneration and fiber damage are observed.
- Neurotmesis. A serious disorder affecting all structures, including fibers and connective membranes. Scar tissue develops, and surgery is indicated to correct the problem.
In accordance with the generally accepted WHO classification, there are five categories of NAS injuries:
- compression, nerves are not damaged;
- swelling of tissues;
- partial rupture of fibers;
- complete ruptures of the NAS are observed;
- post-traumatic fibrosis develops.
Assessment methods
To determine the cause and extent of the disorder, diagnostics are required. For this purpose they prescribe:
- mechanoceptive methods, in which the response to mechanical irritation and stimulation is recorded;
- nociceptive, allowing to determine sensitivity to painful stimulation.
The first type of research includes tests of the following types:
- tests with a brush, during which the Patient’s lip is passed with a brush and asked to determine the direction of movement;
- two-point irritation using a probe.
The second diagnostic method includes:
- pin tests;
- Temperature tests for sensations of cold or heat.
Tests are also carried out for the presence of deficits in the sense of taste, and data from the right and left sides of the maxillofacial apparatus are compared. The accuracy of the research should be no more than 1 mm.
Treatment
The following regimens are used for therapy:
- observation of the Patient at intervals of 2, 3, 4, 6 months;
- drug therapy;
- unscrewing, removing the implant;
- microsurgical intervention.
There is no strict protocol; tactics are determined individually in each case. But there are limitations to surgical intervention - it will be effective only in the first year, after which this method is considered ineffective.
Drug therapy includes:
- taking painkillers;
- use of hydrogen pump blockers;
- prescription of anti-inflammatory drugs (glucocorticosteroids are prescribed);
- therapy for sensory impairment.
If symptoms appear in the first 1.-1.5 days after installation of the implant, its removal may be indicated. During this period, the prognosis is favorable, but over a longer period of time, removing the artificial root will no longer bring a noticeable improvement. The reason is irreversible changes in nerve fibers.
Surgery is indicated in cases where all previous measures have not brought the expected effect. To do this, the doctor must determine the location of the NAS and evaluate sensitivity disorders. The effectiveness of the operation is influenced by the following factors:
- time between injury and surgery;
- severity, type of lesion;
- blood supply;
- Preparation;
- tension zone;
- Patient's age, health status.
Predictions and prevention
Treatment has an uncertain prognosis; with microsurgical intervention, the positive result is in the range of 55-82%. If the damage is severe, complete recovery does not occur with any treatment method. According to some experts, complications such as pain persist even after the intervention. It is also worth noting that the success of treatment depends entirely on the extent of the lesion. It is impossible to guarantee a high result in any situation, that is, the forecasts are uncertain.
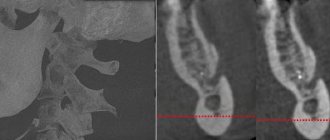
To avoid complications, prophylaxis is recommended. This is a mandatory full examination before the implantation procedure. The specialist will determine the exact location of the nerve, the topography of the nerve trunks and the maxillofacial system. This allows you to exclude the development of pathology and conduct conduction anesthesia correctly, without the risk of complications.
The main preventive measures include:
- competent selection of implantation system;
- diagnostics, including CT, production of a surgical template, computer modeling;
- planning the procedure for introducing an artificial root;
- determining the paths of nerve trunks, ensuring the distance between them and implants is not less than 2 mm;
- when drilling, it is necessary to avoid excessive force;
- When immersing a drill or implant, stoppers are used to limit the depth and ensure safety.
Treatment of damage to the mandibular nerve during implantation requires the doctor to have high qualifications and experience. But even under such conditions, the success rate does not exceed 82%. Some complications may remain, such as numbness or soreness.
Algorithm for patient management in the acute phase (first 30 hours)
There is a limited time window of up to 30-48 hours to make the most correct decision - to recognize the fact of damage to the alveolar and/or lingual nerve after implantation, endodontic treatment or removal of mandibular third molars.
Report by reference Khawaja N, Renton T Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 2009 Apr 11;206(7):365–370 suggests that early removal of the causative implant (within the first 30 hours) results in maximum recovery, but the evidence remains weak.
Suggested protocol based on available evidence:
- Homecheck - The attending physician should contact the patient between 6 and 24 hours after surgery to determine the presence/absence of persistent partial neuropathy after local anesthesia has worn off. This contact is based on the relationship between doctor and patient, which is achieved through signed informed consent.
- Confirm the presence of neuropathy . If the neuropathy affects +/- most of the dermatome, severe nerve injury should be considered, which will be accompanied by neuropathic severe pain if not treated immediately.
- Admit the damage and apologize. An apology is NOT an admission of guilt.
- Additional CT scans or radiography are not necessary or valuable for decision-making in cases of implantation, but are absolutely necessary in cases of third molar extraction.
- Initiate treatment for implant-related nerve damage: - Consider removal of the implant within 30 hours of implantation or sooner; - early therapeutic treatment.
- Acute phase - nerve damage during surgery - Implant removal, immediate nerve restoration +/-.
Neuropathy of the superior alveolar nerve.
The causes of the disease may be chronic pulpitis and periodontitis, nerve damage in case of complex tooth extraction, sinusitis, and surgical intervention for sinusitis.
It manifests itself as pain and a feeling of numbness in the teeth of the upper jaw. Objectively, there is a decrease or absence of sensitivity in the gum area of the upper jaw, as well as the adjacent area of the buccal mucosa. The electrical excitability of the pulp in the corresponding teeth of the upper jaw is reduced or absent.
If the cause of the disease is stenosis of the infraorbital canal, then patients will complain of pain and numbness of the skin in the area of innervation of the infraorbital nerve (wing of the nose, area above the canine fossa, upper lip).
Types of jaw nerve injuries
- Neuropraxia is a minor injury: benign course, favorable prognosis. In the absence of damage to the integrity of the nerve bundle, independent regeneration occurs within a month and a half.
- Axonotmesis is partial degeneration of the myelin sheath: restoration of nervous tissue is incomplete, possibly 1.5 months after damage. Medical attention is required.
- Neurotmesis - complete damage: degenerative changes in biophysical, biochemical parameters of nervous tissue. The prognosis is poor: high risk of irreversible loss of sensitivity .