20.07.2018
The author of the article is Dakhno L.A. Candidate of Medical Sciences, dental surgeon, radiologist.
Post-traumatic neuropathy of the trigeminal system is a sensory disturbance with or without neuropathic pain, often leading to functional and psychological consequences.
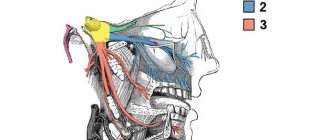
The trigeminal nerve is the largest sensory nerve in the body and is responsible for the orofacial region. Iatrogenic injuries of the trigeminal nerve (trigeminal nerve injuries -TNI) lead to pain in 70% of patients, which in turn leads to functional impairments in speech, eating, kissing, shaving, applying makeup, brushing teeth, etc., which means there is a negative impact on self-esteem, quality of life and patient psychology.
It must be understood that after injury to the trigeminal nerve, complete recovery is rare, except in cases of minor injury, so it is very important to maintain a trusting relationship between the dentist and the patient and not give false assurances of a complete recovery.
Nerve damage can occur during any dental procedure: injections of local anesthesia, wisdom tooth extraction, endodontic treatment, as well as at all stages of implantation - from the administration of anesthetic and preparation of the implant bed to implantation, bone augmentation and/or soft tissue swelling after surgery .
Rice. 1 Clinical case. CBCT computed tomography images show fragments of sealer that are directly adjacent to the lumen of the mandibular canal in the area of the mental foramen. The patient complained of paresthesia and pain from touch and wind in the area of the chin and lower lip on the left, which appeared after endodontic treatment of the 34th tooth. After 6 months - paresis (motor disorder) of the left half of the lower lip, which led to the inability to fully drink and eat (the patient holds the lip with her fingers while eating to prevent food and liquid from falling out of the mouth) and, as a result, a stress disorder accompanied by anxiety, fear and fits of anger.
Fig. 2. Removal of the sealer into the mandibular canal due to the absence of an apical stop
Regarding implantation, pain during bone preparation with a pilot drill can be an indicator of the proximity of the nerve and, if this is not addressed immediately (deciding to place a shorter implant), permanent nerve damage can occur.
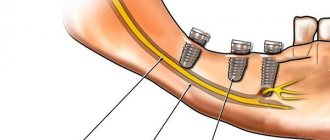
Nerve injury during implantation is associated primarily with preoperative factors, including poor preoperative planning, which leads to inaccurate measurements and incorrect selection of implantation site and implant type (diameter and length).
Figure 3a. Planning error.
Figure 3b. Incorrect choice of implant length.
Figure 3-a, b. CBCT images from two clinical cases demonstrate implantation-related nerve damage. The implants are inserted directly into the canal of the inferior alveolar nerve, which is associated with errors in preoperative planning.
The habit of carefully planning implantation based on computed tomography data, performing implantation under infiltration anesthesia using surgical guides, performing intraoperative X-ray control and using drill stops (drill stops) can minimize possible nerve injury during implantation.
Any injury (penetration or compression) as well as hemorrhage into the mandibular canal results in acute and often severe intraoperative pain of the neuralgic type and it is imperative that the physician use an appropriate protocol of infiltration local anesthesia so that the patient can indicate the proximity of surgical instruments to the mandibular canal .
Since implantation is the surgery of choice, nerve injury, which leads to potentially irreversible consequences even after repeated surgery (implant removal), can always be avoided.
The physiological consequences of sensory nerve damage are immediate and often irreversible. The inferior alveolar nerve passes through the bony canal, which may be subject to compression and ischemic damage. Compression of peripheral sensory nerves for 6 hours can cause nerve fiber atrophy.
Ischemia itself, even without direct nerve damage, will cause sufficient inflammation and nerve damage that may result in permanent nerve damage.
Figure 4. Sagittal CBCT sections demonstrate an acceptable relationship between the implant and the lumen of the inferior alveolar nerve canal, but the clinical picture is consistent with ischemia, which caused pain and paresthesia. During the first 24 hours, a clinical decision was made to remove the implant and prescribe medication.
Three months after injury to the inferior alveolar nerve, permanent changes in the nervous system, both central and peripheral, will occur, which are unlikely to respond to surgical treatment or respond to drug treatment and peripheral interventions.
When nerve injury occurs, the clinician must be able to recognize the type and extent of injury, provide the most appropriate postoperative care, and be able to make recommendations.
Types of nerve damage:
- complete or partial resection of the nerve (cutting),
- compression, crushing, stretching, pinching, thermal and ischemic damage.
Total sensory deficits can range from minor sensory loss to persistent, severe, and debilitating pain dysfunction, but the most common combinations include anesthesia, paresthesia (painless altered sensation), dysesthesia (uncomfortable altered sensation), and neuropathic pain.
Currently, there is no standardized protocol for the dentist to diagnose and treat post-implant nerve injuries.
We will try to fill this gap.
What is mandibular nerve injury?
By this concept, dentists mean injury to one of the nerves:
- chin;
- lingual;
- alveolar.
Types of injuries include sprain, compression, crushing and rupture - partial or complete. The cause of the stretching is the long-term retraction of the mucoperiosteal flap, which is created by an implant of greater length than necessary. Crush injuries and compression are caused by needle injuries during the administration of anesthesia. Rupture occurs in two cases: when cutting the mucosa or during preparation of the hole for the implant.
Contraindications
The dentist will refuse to perform depulpation if:
- history of acute respiratory viral infection, sore throat, influenza;
- Stomatitis, acute leukemia, and hepatitis of infectious origin were diagnosed.
Contraindications to manipulation are heart disease in the acute stage and inflammatory pathologies of the oral cavity.
Remember: women in the 1st and 3rd trimester of pregnancy cannot have the nerve removed! This is due to possible psycho-emotional outbursts and (in the absence of pain relief) the painfulness of the procedure. Anesthesia during these periods is undesirable.
Causes and prevention of mandibular nerve injuries
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.
Classification and diagnosis of pathology
Facial nerve injuries are divided into the following types:
- neuropraxia (cured in 3-5 weeks);
- axonotmesis (moderate nerve damage, requiring up to six months of therapeutic treatment);
- neurotmesis (irreversible changes in the structure of nerve fibers. Cannot be treated with medication. Surgical intervention is required).
This neurological pathology is diagnosed using two methods:
- mechanoceptive (brush test - the patient is carried out on the lip, and the patient says the direction of movement and irritation with two points - a device resembling a mathematical compass is applied to the lower part of the face. In this case, the distance between the legs of the device is constantly increasing. As soon as the patient stops feeling each injection separately, the result is recorded and the degree of nerve damage is determined);
- nociceptive (pin prick, temperature test).
Taste buds are tested by dipping a cotton swab in salty or sweet water.
Treatment
Pain in the area of the inferior branch of the trigeminal nerve requires the use of 3 treatment methods.
Drug therapy. The doctor prescribes blockers and painkillers to reduce symptoms. The dentist will also recommend anti-inflammatory therapy. This treatment usually lasts 5-7 days.
Removing the artificial root. 1-1.5 days after implantation of the rod (if symptoms occur), dentists recommend immediately removing the implant, since such a decision increases the chances of a favorable outcome of therapy. Further treatment is carried out with medication.
Surgical intervention. Indications for a radical method are considered to be the failure of removal of the implant and treatment with medications.
Important! Removing the implant is not always the key to successful treatment of the nerve, but this action increases the chances of a quick recovery and reduces the risk of tumor formation in the area of the nerve bundle.
Treatment tactics are agreed upon with the patient, who signs consent for the operation.
Predictions and prevention
| Click to sign up for a FREE consultation |
Neuropraxia and axonotmesis are quite treatable. Statistics show that more than half of patients completely cure the disease. With neurotmesis, complete recovery does not occur.
Dentists call the main preventive measure a comprehensive study of the performance of the dental system before implantation. At the diagnostic stage, the doctor finds out the exact location of the nerve. This helps to avoid injury to the “twig”.
An experienced dentist will definitely analyze CT and X-ray data, compare the results and draw up an implantation plan based on the individual structural features of the patient’s lower jaw.
The implant is screwed in carefully; its final position should be no closer than 2 mm to the nerve process.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Removal steps
Depulpation is a dental operation that is carried out in stages:
- Examination and diagnosis. Radiography is often used. This research method helps determine the viability of nerve endings, the length and direction of canal branches.
- Anesthesia. Local anesthesia is preferably used, but sometimes general anesthesia is administered for medical reasons or patient preference.
- Isolation of the tooth using a rubber dam (special latex film). This will help prevent infection from entering the open cavity of the canal.
- Depulpation. After removing the destroyed layer of enamel and dentin, the pulp chamber is opened. The contents are removed using a pulp extractor.
- Filling root canals with gutta-percha.
- Installation of temporary or permanent filling.
- Repeated radiography to detect voids in the canal and double-check the accuracy of installation of the filling material.
This depulpation process is applied to premolars and molars, except for the number eight. Removing the nerve in a wisdom tooth is a more complex procedure. The location of the tooth does not always allow for high-quality filling of the canals.
Complications after surgery
The main causes of complications are fatigue, lack of professionalism of the dentist, and poor-quality equipment.
A complication from the aesthetic side is a change in the shade of the tooth crown. Its color depends on the material used to prepare the filling.
Care after removal
It is important to strictly follow the dentist’s recommendations and follow all his instructions:
- absence of stress for 2-3 hours after depulpation;
- It is forbidden to eat food and drink drinks for 4-5 hours;
- It is not recommended to chew on the side where the filled tooth is located for about a few days;
- Be sure to rinse and take medications prescribed by your doctor.
Symptoms and stages of damage
The symptoms by which this complication can be recognized are as follows:
- numbness of parts of the head - tongue, lips, chin, cheeks, etc.;
- biting lips and tongue;
- choking while eating or drinking;
- profuse salivation.
All this creates a number of inconveniences for the patient: it makes it difficult to eat and talk, disrupts facial expressions, and also prevents men from shaving and women from applying makeup. The severity of this injury is determined by its degree: a minor one goes away on its own or with the help of drug treatment, a severe one leads to irreversible processes of nerve degeneration and is not curable. Damage to the mandibular nerve, the symptoms of which the patient observes, requires immediate consultation with a doctor - only a specialist will be able to determine its extent and provide timely assistance.
Dentists distinguish the following stages of this implantation complication:
- minor - neuropraxia;
- more severe, but partial damage - axonotmesis;
- a serious injury that leads to complete loss of sensitivity - neurotmesis.
When performing dental implantation in the lower jaw, there is a potential risk of damage to the inferior alveolar nerve (IAN) and, as a result, disruption of its function [6, 8]. According to a number of authors [1, 3, 5], the incidence of this kind of complications during dental implantation ranges from 8.5 to 33% of the total number.
Perforation of the mandibular canal and nerve injury during the formation of the implantation bed, as well as compression of the nerve directly by the dental implant or due to postoperative swelling lead to peripheral neuropathy. This complication manifests itself in the form of absence and/or long-term changes in the sensitivity of tissues in the innervation zone, the development of pain of varying intensity, and is also accompanied by emotional and stress disorders and significantly worsens the patient’s quality of life [6, 8, 10].
After injury, complete regeneration of the nerve is possible provided there is no prolonged influence of the traumatic agent, as well as obstacles to axon growth and restoration of blood flow in the damaged area. Otherwise, already 2 months after the injury, atrophy and sclerosis of the nerve distal to the damaged area begin [4]. This can cause long-term sensory disturbances in the innervation zone. Consequently, there is a need for the earliest possible diagnosis of complications and treatment, which is aimed at restoring the anatomical integrity and functional viability of the NAS.
The purpose of the study is a clinical and physiological study of dysfunction of the NAS as a complication of dental implantation, determination of tactics and treatment strategies.
Material and methods
The main criterion for including patients in this study was the presence of signs of dysfunction of the NAS after dental implantation performed in the lateral areas of the lower jaw. In the specialized department of the Department of Faculty Surgical Dentistry and Implantology of the Moscow State Medical and Dental University, 32 patients (24 women and 8 men) aged from 26 to 60 years with installed screw implants of various systems in the amount of 1 to 4 on the side of the nerve injury were observed . After a thorough interview and history taking, all patients underwent general examination methods, as well as an assessment of local neurological status. Pain intensity was assessed using a 10-point visual analogue scale (VAS). The sensitivity of the tissues of the chin area, lower lip on the side of the injury and the symmetrical side was studied using sensory tests. The response to tactile (touching the skin with a cotton ball), pain (tingling with a needle) and temperature (metal surface, test tube with hot water) stimuli was assessed. The area of sensitivity impairment was calculated in centimeters using the formula for calculating the area of a trapezoid or rectangle and was necessarily photographed for comparison in dynamics (Fig. 1).
Figure 1. Area of sensory impairment based on sensory tests.
The degree of sensory impairment after dental implantation was assessed by measuring sensitivity thresholds in the zone of innervation of the inferior alveolar nerve. Single pulses of electric current with a duration of 0.1 ms and a frequency of 0.5 pulses/s with a gradually increasing amplitude from 0.5 to 99 mA were used as a stimulus. The electrode was installed on the skin in the projection of the lower lip and chin area both on the side of the nerve damage and on the symmetrical side, comparing the results with the average values [2]. When conducting research, the following criteria were used: sensation threshold, pain threshold, pain tolerance level. The selected criteria correspond to the definition of these concepts, which was adopted by the International Association for the Study of Pain [9].
Many scientific studies have established a high data error in orthopantomography, therefore, to determine the anatomical features of the mandibular canal and clarify the localization of the dental implant, all patients underwent computed tomography of the mandible [7, 10]. Based on the results of computed tomography, the patients were divided into two groups. Group 1 included 10 (31%) patients in whom the dental implant was adjacent to the mandibular canal without violating the integrity of its cortical plate (Fig. 2, a).
Figure 2. Fragments of a computed tomogram in transverse (left) and panoramic (right) sections. a — patient S. from group 1.
Group 2 included 22 (69%) patients with a dental implant located directly in the lumen of the mandibular canal (Fig. 2, b).
Figure 2. Fragments of a computed tomogram in transverse (left) and panoramic (right) sections. b — patient M. from group 2.
results
When analyzing the results of the study, a tendency was revealed to increase the number of complications depending on age and gender: 26 (81%) people were between the ages of 40 and 60 years. This fact is probably associated with the phenomena of atrophy of the alveolar part of the lower jaw, as well as the peculiarity of the ratio of spongy and compact substance at this age, which increases the risk of damage to the NAS. The work demonstrated the predominance of this complication in females with a female/male ratio of 3:1, which is consistent with literature data [5]. These features, of course, can be an additional risk factor in the formation of an implantation bed in women after 50 years of age.
The key differential diagnostic feature was the absence of spontaneous and evoked pain in 100% of patients in group 1. All patients complained of decreased sensitivity of tissues (hypoesthesia) innervated by the NAS, and 70% additionally experienced various types of paresthesia in the form of a feeling of “crawling” in this area. A slight decrease in tactile and temperature sensitivity of tissues was determined, and the perception of a painful stimulus was practically no different from the symmetrical zone. The area of sensory impairment in the zone of innervation of the NAS averaged 11.4±2.96 cm2.
A characteristic feature of patients in group 2 was the absence in 82% of patients or a significant and persistent decrease in 18% of patients in tissue sensitivity to tactile, temperature and pain influences in the area of innervation of the NAS.
In group 2, 18% of patients had the main complaint of pain in the lower lip on the side of the nerve injury. The pain was spontaneous and of moderate intensity according to VAS (3-5 points). Also characteristic complaints were unusual sensations of a constant nature in the form of “crawling goosebumps”, “tingling” and unpleasant sensations (dysesthesia) when touching the lower lip, chin area, when talking, or eating. When conducting sensory tests, a pronounced decrease in tactile, pain and temperature sensitivity of tissues innervated by the NAS was revealed. The area of sensory impairment in the zone of innervation of the NAS averaged 13.6±0.86 cm2.
In patients of both groups, the threshold of sensation (TS) in the zone innervated by the NAS on the side of the injury statistically significantly exceeded the normal limit values. During clinical examination, this is expressed by a decrease in tactile sensitivity. A clear intergroup difference was the pain threshold (PT), which statistically significantly exceeded normal limits in all patients of group 2, of which in 8 patients with pain syndrome PT was not determined even at the highest possible intensity of testing stimulation, which indicates a significant degree of nerve damage on the implantation side. This kind of dysfunction of the NAS corresponded to the localization of the dental implant directly in the lumen of the mandibular canal and was diagnosed in 69% of the total number of patients examined. In group 1, no changes in PA indicators and pain tolerance level (PET) were detected in all patients (Fig. 3).
Figure 3. Results of assessing sensitivity thresholds (ST) in the zone of innervation of the NAS on the side of the injury.
All patients of group 1 received conservative treatment aimed at reducing swelling and stimulating the function of the NAS, as well as dynamic observation by a neurologist. Within 1-2 months, complete restoration of sensitivity in the zone of innervation of the NAS was determined.
Patients of the 2nd group underwent removal of the dental implant from the lumen of the mandibular canal according to the timing of their visit, followed by treatment by a neurologist. A favorable outcome of treatment, when carried out in a timely manner as early as possible, was obtained in patients of group 2 without pain, despite the localization of the dental implant in the lumen of the canal. In 10 patients of group 2, in whom the implant was removed from 14 days to 2 months after damage to the NAS, restoration of nerve function began in the immediate postoperative period and ended by 6-8 months. With later removal of the dental implant (in 2 patients 6 months after injury), full restoration of NAS function was observed only after 1 year.
Two patients without pain refused treatment and further observation. In 4 patients with pain syndrome, dysesthesia with an unpleasant tint in the lower lip area persisted after 1 year. By this time, there was a restoration of pain and temperature sensitivity, but not in full, with a decrease in the area of hypoesthesia of the lower lip to 5 cm.
The study made it possible to determine the doctor’s tactics in case of dysfunction of the NAS after dental implantation (see diagram).
Scheme 1. Scheme. Doctor's tactics for dysfunction of the inferior alveolar nerve (IAN) after dental implantation (DI).
conclusions
1. The appearance of pain after dental implantation and the absence of all types of tissue sensitivity in the zone of innervation of the NAS is an indication for removal of the dental implant.
2. A mandatory research method for all patients with dysfunction of the NAS is computed tomography or dental volumetric tomography of the mandible to determine the localization of the dental implant relative to the mandibular canal.
3. If the dental implant is localized in the lumen of the mandibular canal and there are sensory disturbances, removal of the dental implant from the lumen of the canal as early as possible is indicated.
4. Detection of signs of dysfunction of the NAS after dental implantation is a clear indication for consultation and treatment with a neurologist.
5. If the dental implant is located outside the lumen of the mandibular canal, but in the presence of clinical symptoms of dysfunction of the NAS, it is necessary to carry out conservative therapy and dynamic observation together with a neurologist for 8 weeks with mandatory recording of the dynamics of the complication.
Recovery and treatment
In the first case, self-recovery takes approximately 1 month; the help of doctors is not needed, since there is no anatomical damage. Symptoms of the second appear after a while - usually 6-8 weeks, so recovery can be painful and incomplete: it will take more than 2 months. In the third stage of damage to the mandibular nerve, treatment gives results only at the beginning and is performed surgically, since we are talking about degeneration with a violation of integrity. Loss of sensitivity, which is observed in a patient for more than 3 months, indicates a high probability of losing it forever. Damage to the mandibular nerve, the consequences of which is the lack of sensitivity of the nerve for a year, leads to irreversible changes. Only the professionalism and responsibility of the doctor, which is guaranteed by the specialists of our Implantmaster clinic, can protect the patient from such unpleasant injuries.
Author:
Probability of occurrence
The mandibular nerve fascicle is a fragment of the trigeminal nerve. It provides sensitivity to intraoral and facial tissues, and is responsible for contraction of the facial muscles and dentofacial apparatus. The bundle consists of motor and sensory fibers and nuclei.
The inferior alveolar nerve (IAN) is located in the lower jaw and is one of the three endings of the trigeminal nerve. The NAN borders the root system of the mandibular arch. In this regard, there is a high risk of damage during dental treatment.
The statistics of nerve damage are especially high during the period when dental operations were performed without the use of modern technologies.
According to the latest data, the incidence of nerve damage during dental implantation does not exceed 3%. Of this number, only 1.7% end up with permanent neuropathy.
According to some dentists, these data are underestimated, and the percentage of damage to NAS reaches 30%. In any case, this issue should be given sufficient attention.