Inflammation of the maxillary sinuses is not the most dangerous disease today. The large number of effective antibiotics makes treatment of this disease relatively simple. However, if left untreated, sinusitis can cause serious complications. It is known that everything in the human body is interconnected. The source of infection and inflammation in the nasopharynx can spread to other parts of the head. The most dangerous are meningitis and cerebral edema.
Sinusitis can be acute or chronic. The acute form of sinusitis most often occurs due to infection entering the nasopharynx. The causes of this disease are viruses, bacteria or fungi. Most often, sinusitis occurs against the background of a viral infection. Inflammation of the maxillary sinuses caused by a fungal infection is difficult to treat.
In addition, inflammation of the paranasal sinuses can occur as a result of its injuries, which can lead to disruption of the anatomical structure of the bone walls of the nasal cavity and sinuses. Also, sinusitis often appears after a long allergic rhinitis.
Chronic sinusitis occurs in the absence of proper and timely treatment of the acute form of the disease. Treatment of chronic sinusitis requires much more time and effort. Therefore, it is better not to bring your body to such a state.
Main symptoms of sinusitis
The main and most well-known symptom of inflammation of the maxillary sinuses is headache. In some cases, pain can cause a lot of inconvenience; in rare cases, the pain reaches such heights that it is necessary to take painkillers. At the beginning of the disease it has a certain localization. With sinusitis, discomfort occurs in the forehead, nose and around the eyes. However, after some time the pain becomes irritating, affecting many areas of the head.
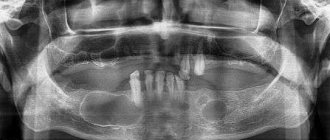
The pain of sinusitis can sometimes be very similar to the pain of a migraine. However, sinusitis also has other symptoms, which, coupled with headaches, allow the doctor to diagnose this disease quite accurately. To confirm the diagnosis, radiography of the paranasal sinuses is used.
On x-rays with sinusitis, shadows are clearly visible, in which you can guess the fluid accumulated in the maxillary sinuses of the nose. This liquid is a mixture of mucus and pus. It is the accumulation of exudate in the maxillary sinuses that is responsible for the appearance of headaches, as it puts pressure on the inflamed mucous membrane and causes discomfort.
Headache with this disease can intensify when bending the body forward, as well as from sudden movements of the head. To minimize discomfort, the patient needs rest. There are also other symptoms of inflammation of the maxillary sinuses:
- nasal discharge;
- nasal congestion;
- swelling of the soft tissues of the face, eyelids;
- increased body temperature;
- weakness, irritability.
These symptoms are characteristic not only of sinusitis, but coupled with a severe headache, they indicate precisely this disease. If you suspect an inflammatory process in the maxillary sinuses, you should immediately consult a doctor and undergo an examination to confirm the diagnosis. Untreated sinusitis can have serious consequences for the body.
Prevention
To prevent malignant tumors of the nose and sinuses, it is important to promptly treat inflammation of the nasal structures, prevent the development of hyperplastic processes and immediately remove polyps.
Subsequently, after completing the course of treatment, patients are observed by an oncologist. The first two years should be examined monthly, the next five years - every six months. If there is an increased risk of relapse, routine examinations are prescribed individually.
List of references on the topic:
- Gantsev Sh.H. Oncology – M, 2012 – P.204-205.
- Golovin D.I. Errors and difficulties in diagnosing tumors, D.: Medicine. Leningr. department, 2015 305 pp.
- Golovin D. Im Dvorakovskag I. V. Tumors of the nose and paranasal sinuses. L.: Medicine. Leningr. department 2014. 94 p.
- Selected lectures on clinical oncology/Ed. IN AND. Chissova, S.L. Daryalova. – M., 2010
- Matyakin E.G., Alferov V.S. Chemotherapy of head and neck tumors // Mat. 2nd Ros. oncol. conf. “Current trends in the development of drug therapy for tumors” December 8–10, 2021 – M., 256 p.
- Podvyaznikov S.O., A.I. Paches, T.D. Tabolinovskaya Diagnosis and treatment of malignant tumors of the nasal cavity and paranasal sinuses // SIBERIAN JOURNAL OF ONCOLOGY. . — 2011.
- Tumors of the head and neck: hands/ A.I. Paches. - 5th ed., add. And revised - M.: Practical Medicine, 2013. -478 p.
- Khasanov A.I. Comparative assessment of the effectiveness of treatment of locally advanced malignant tumors of the upper jaw of the nasal cavity and paranasal sinuses Vestn RORC im. N.N. Blokhin RAMS. 2006. T. 17. No. 1 P. 45-49
- Shine A.A. Oncology. M – 2014 365 pp.
- Encyclopedia of Clinical Oncology/Ed. M.I. Davydova. – M., 2014 –P.140-179.
Features of radiography for sinusitis
The main way to confirm sinusitis today is still radiography. The procedure takes very little time and is available in most clinics in Russia.
On an x-ray of the paranasal sinuses with sinusitis, darkening in the area of the maxillary sinuses is clearly visible, indicating that there is an inflammatory process and there is excess fluid. Depending on the severity of the disease, the darkening can be local (small), subtotal and total.
Small darkening indicates that the disease began not long ago, the painful manifestations are not very pronounced, and drug treatment will be most effective.
Subtotal blackout
Subtotal darkening of the maxillary sinuses may indicate a severe inflammatory process. This suggests that the disease is in an advanced state. In such cases, in addition to antibacterial therapy, procedures may be prescribed to remove fluid from the inflamed sinus cavity.
Sometimes the inflammation spreads to other paranasal sinuses. Sinusitis can turn into frontal sinusitis or sinusitis. In such cases, the pathological process affects, respectively, the frontal sinuses or the ethmoid labyrinth.
Total blackout
Detection of total darkening on an x-ray is an alarming sign. However, modern medicine copes with such advanced cases. The most important thing is that treatment is started immediately.
If the sinuses are filled with pus and inflammatory processes are in full swing, then doctors prescribe fairly high doses of antibiotics to prevent the development of serious complications. Additionally, a puncture of the maxillary sinuses can be performed to remove accumulated exudate.
Specific signs
In the later stages of oncology development, characteristic clinical features appear that help identify the location of the tumor.
Thus, cancer of the maxillary sinuses causes forward displacement of the eyeballs, swelling of the cheeks, and decreased visual acuity. When the posterolateral and posterior wall is damaged, the temporal fossa swells and exophthalmos develops. Complete obstruction of the nasal passages indicates cancer of the medial wall. A tumor of the ethmoidal labyrinth is recognized by lacrimation, deformation of the inner corner of the eye, and changes in the shape of the lower eyelid.
Already in the later stages of development, nosebleeds appear, protrusion of the eyeballs worsens, the hard palate is deformed, and the retropharyngeal, cervical and parotid lymph nodes enlarge.
Possible complications of advanced sinusitis
Sinusitis in itself is not a dangerous disease. However, inflammation in tissues so close to the brain can have serious consequences, especially if not treated adequately and promptly.
Meningitis and meningoencephalitis
Meningitis is a dangerous disease characterized by an inflammatory process in the membranes of the brain. This disease can lead to disability and even death.
Meningoencephalitis is an even more serious disease. Inflammation in meningoencephalitis covers both the membranes and the substance of the brain.
The symptoms of these diseases are similar:
- headache;
- nausea;
- vomit;
- chills;
- elevated body temperature.
These diseases are very insidious. If there are prerequisites for their occurrence, they can develop in an acute form within just a few hours.
Both diseases are extremely dangerous and have a poor prognosis. High probability of death.
Chronic sinusitis
If acute sinusitis is treated incorrectly or not treated at all, the disease may become chronic. Chronic sinusitis is difficult to treat, and it is impossible to guarantee a positive treatment outcome.
Periodically, with a decrease in immunity, chronic sinusitis will worsen, causing a lot of inconvenience. In addition, a chronic inflammatory process in the maxillary sinuses is fraught with much more serious problems, including:
- chronic rhinitis;
- inflammation of bone tissue;
- inflammation of brain tissue.
You should take care of your health. Then the occurrence of a disease such as chronic sinusitis is unlikely.
Chronic rhinosinusitis
characterized by parietal thickenings caused by hyperplasia of the mucosa and partial fibrous changes in it. The thickness of the mucous membrane ranges from 4-5 mm.
Sinonasal polyposis, hypertrophic sinonasal rhinosinusitis. Non-tumor inflammatory swelling of the mucous membrane.
Recently, there has been an increase in the number of fungal sinusitis. Chronic forms occur under the guise of polypous recurrent sinusitis, the MRI picture is nonspecific, and laboratory diagnosis is difficult. There may be a change in the bony walls of the sinuses due to hyperostosis or destruction of the sinus wall as a result of prolonged pressure from the fungal body.
Treatment of advanced sinusitis
After developing radiographs, one can judge the severity of the inflammatory process occurring in the maxillary sinuses. In case of total blackout, the doctor may prescribe a shock course of antibiotics and antihistamines to suppress inflammatory processes and reduce the severity of some symptoms.
In the most severe cases, surgical intervention may be indicated - puncture of the sinuses. This procedure has been known for a long time and is widely used in many countries around the world. Using a special syringe, excess fluid and pus are pumped out of the maxillary sinus. Then the sinus is filled with a special solution containing antiseptic drugs. This is done to reduce inflammation of the mucous membrane. Then the solution is pumped out of the sinuses. That's it, the procedure is completed.
This type of surgery is not dangerous, but it can speed up recovery and reduce the appearance of major symptoms, such as headaches.
For more effective treatment of sinusitis, the pus obtained after puncture can be sent for culture to identify the pathogen and determine which antibacterial drugs it is most sensitive to. Along with antibiotics, antihistamines are often prescribed to help reduce swelling, nasal congestion and other manifestations of the disease.
Some traditional medicines can be used to treat sinusitis. Such remedies should not replace the primary treatment prescribed by a doctor. They can only complement it. Moreover, before using any means, you should consult your doctor.
Using exclusively traditional medicine to treat sinusitis can lead to disastrous results. Untreated sinusitis will become chronic and will periodically trouble the patient throughout his life.
Causes
Oncological processes develop against the background of chronic hyperplasticity. Based on practice, cancer of the nose and sinuses becomes a consequence of complications:
- cysts of radicular or follicular type;
- purulent glandular-fibrous polypous rhinosinusitis;
- purulent polypous rhinosinusitis, complications of which are caused by dysplasia and metaplasia of the epithelium;
- hyperplastic sinusitis with dysplasia;
- chronic sinusitis;
- pigmented nevus;
- perforation of the nasal septum;
- leukoplakia.
The development of a malignant tumor is influenced by such diagnoses as squamous cell papilloma, hemangioma, fibromatosis, osteoblastoclastoma, pleomorphic adenoma of the minor salivary gland. Nasal cancer is diagnosed at any age, but a greater prevalence of the disease is recorded in old age after 60 years. A malignant tumor ranks 35th among all oncological pathologies. The risk group includes:
- patients who had nasal polyps removed or cauterized;
- people working in hazardous industries. Inhalation of carcinogens and chemicals affects the condition of the mucous membrane;
- unfavorable ecology and other environmental factors.
The harm of self-medication
The most obvious harm of self-medication is the lack of positive results. People often take medications until they feel better. However, this approach is wrong. Antibacterial drugs should be taken only as prescribed by a doctor. Strictly in the volumes and within the time frame that he announced at the reception. Otherwise, the symptoms will go away, but the source of infection will remain. Inflammation in the maxillary sinus will become chronic.
Or, if the drugs were chosen incorrectly, there may be no improvement at all. The disease will become advanced, the pain due to overcrowded sinuses will become unbearable, and inflammation will have a chance to spread to the organs and tissues closest to the sinuses, causing all sorts of complications.
Another risk of self-medication is the medications that must be taken for sinusitis. If the dosage is incorrect, taken too often, or if there are problems with internal organs, antibacterial drugs can do more harm than good. Cases of drug-induced liver damage from uncontrolled use of antibiotics are not so rare. What can we say about gastrointestinal tract disorders, dysbacteriosis, and so on.
GBOU "NIKIO im. L.I. Sverzhevsky" of the Moscow Department of Health
Developer institution:
State Institution "Moscow Scientific and Practical Center of Otorhinolaryngology" of the Moscow Department of Health.
Compiled by:
- doctor med. Sciences, Professor A.I. Kryukov
- doctor med. Sciences, Professor N.L. Kunelskaya
- Candidate of Medical Sciences Sci., Head of Pathology Department
- upper respiratory tract A.B. Turovsky
- Candidate of Medical Sciences Sciences D.V. Kravchenko
Reviewers:
Head Department of Otorhinolaryngology RUDN, Professor V.F. Antoniv
Professor of the Department of Ear, Nose and Throat Diseases at MMM named after. I.M.Sechenova V.P.Gamov
Purpose:
The guidelines contain a diagnostic and treatment algorithm for orbital rhinosinusogenic complications. The recommendations are intended for otorhinolaryngologists and ophthalmologists.
This document is the property of the Moscow Department of Health and may not be reproduced or distributed without appropriate permission.
List of abbreviations
- HBOT - hyperbaric oxygenation.
- CT – computed tomography examination.
- MRI – magnetic resonance imaging examination
- AGS – acute purulent sinusitis.
- ORO – orbital rhinosinusogenic complications.
- RNET - regional indirect endolymphatic therapy.
- TAME – transport activity of ciliated epithelium.
- FERSH - functional endoscopic rhinosinus surgery.
- CHC is chronic purulent sinusitis.
- EI – endoscopic examination.
Introduction
Paranasal sinusitis, especially its purulent forms, are the most common cause of orbital inflammatory complications, according to the observations of a number of authors, from 0.5% to 8.4% of cases, posing a danger to both the vision and the life of the patient. However, by now, the causes of this orbital pathology, with the advent of CT and EI, require clarification.
A large number of scientific works by both otorhinolaryngologists and ophthalmologists are devoted to the issues of diagnosis and treatment of orbital rhinosinus complications. Improving the general condition of the patient was the main goal. Mortality from this disease is currently minimized thanks to the use of antibiotics and developed methods of surgical treatment of purulent sinusitis. But the prognosis in terms of vision remains unfavorable and is associated with impaired blood circulation in the optic nerve. According to various studies, blindness occurs in 0.8 - 3% of patients with rhinosinusogenic orbital complications.
Therefore, the problem of increasing the efficiency of diagnosis and treatment of ORO remains relevant and modern.
Etiological prerequisites for the occurrence of orbital
rhinosinusogenic complications.
It is traditionally believed that the etiological factor in the occurrence of ARO are the same pathogens as in sinusitis, which caused this complication. As a rule, the main causative agents of AGS are Streptococcus pneumoniae, Haemophillus influenzae and Moraxella catarrhalis, anaerobic microorganisms. With CHC, the proportion of gram-negative microflora and anaerobic microflora increases (40%). Among the strains sown from discharge obtained from the paranasal sinuses during chronic inflammation, the most frequently identified are: Staphylococcus aureus (18.4%), Pseudomonas aeruginosae (5%), Escherichia colli (4.5%), Haemophilus influenzae (4.5 %), Streptococcus pneumoniae (3.9%), Enterobacter aerogenes (3.4%), Moraxella catarrhalis (2.8%). Serratia marcenscans, Klebsiella species, Proteus mirabilis, Citrobacter, Streptococcus agalactiae, α-hemolytic Streptococcus, β-hemolytic Streptococcus are much less common.
Currently, there is an increase in the resistance of pneumococcus to drugs such as semisynthetic penicillins and macrolides. There are practically no strains resistant to aminopenicillins (amoxicillin) and the latest generation of fluoroquinolones (levofloxacin and moxifloxacin).
There has been an increase in resistance to penicillins in many strains of Haemophillus influenzae, which is associated with their production of betalactamases. In Russia, the frequency of occurrence of penicillinase-forming strains does not exceed 14%. High activity against H. influenzae is observed among aminopenicillins potentiated against β-lactamases with clavulanic acid (amoxicillin-clavulanate, ampicillin - sulbactam, ticarcillin - clavulanate); cephalosporins (cefuroxime, ceftriaxone) and fluoroquinolones (levofloxacin, moxifloxacin).
M. catarrhalis strains (up to 98%) produce β-lactamases, and therefore are insensitive to the action of unprotected aminopenicillins. They remain highly sensitive to protected aminopenicillins (amoxicillin-clavulanate), cephalosporins, macrolides (azithromycin, clarithromycin) and fluoroquinolones (levofloxacin , moxifloxacin).
According to our studies, S. aureus, group A streptococci, enterobacteria, and H. Influenzae are most often observed in the inflammatory process in the orbit. Along with this, in some cases, bacteria of the intestinal group (enterococci, Escherichia coli, Proteus) are determined. In almost all cases, a mixed flora is observed (aerobic and anaerobic), among the latter there are representatives of Peptostreptococcus spp., Prevotella spp., Bacteroides spp., Peptococcus spp., Veillonella spp., Prevotella spp., Fusobacterium spp., Corynebacterium spp. together with Staphylococcus aureus, β-lactamase-producing streptococci.
Anatomical prerequisites for the occurrence of orbital
rhinosinus complications
The possibility of OPO occurrence is due to the anatomical features of the location and structure of the orbit. The bony base of the orbit has the shape of a four-sided pyramid, which is made up of seven individual bones. The upper wall is in contact with the bottom of the frontal sinus, the lower wall is the roof of the maxillary sinus, the medial wall consists of a very thin tissue plate of the ethmoidal labyrinth and is in contact with the sphenoid sinus. The walls of the orbit are covered with a periosteum, which is loosely connected to the underlying bones, with the exception of the suture area. This structural feature contributes to easy detachment of the periosteum when the infection spreads by contact. The tarsorbital fascia separates the contents of the orbit from the soft tissues of the eyelids, acting as an additional wall; in front of it in the initial part of the orbit are the eyelids and lacrimal sac, the eyeball and muscle endings. Posterior to the orbital septum are the optic nerve, extraocular muscles, neurovascular formations of the orbit, and fatty tissue.
In the pathogenesis of orbital complications in sinusitis, the following anatomical factors are also important: 1) the upper and lower walls of the orbit are the walls of the frontal and maxillary sinuses, 2) the medial wall of the orbit borders the cells of the ethmoid sinus and has 3 slits (lacrimomaxillary, lacrimal-ethmoidal and sphenoid-ethmoid), 3) the venous and lymphatic systems of the orbit are closely related to those of the nose and paranasal sinuses, 4) the periosteum of the orbit is the weakest point in the spread of infection from the nasal sinuses, since the contents of the orbit are separated by a barrier only of soft tissue.
One of the options for the structure of the orbit is the presence of dehiscence in the area between the upper and medial walls of the orbit, which leads to contact of the mucous membrane of the cells of the ethmoidal labyrinth and the contents of the orbit.
The spread of the pathological process from the paranasal sinuses most often occurs hematogenously, contact - through dehiscence of the tissue plate or through the bone destroyed by a purulent - inflammatory process, perineurally, and also lymphogenously.
Hematogenous infection of the orbit occurs through small venous vessels of the ethmoidal labyrinth, which pierce the bone wall of the orbit and through venous branches flowing into the superior ophthalmic vein. The lymphogenous route of infection plays an important role in ORO, despite the absence of lymph nodes and vessels in the orbit. The main flow of lymph occurs through the perivascular spaces and through the inferior orbital fissure into the pterygopalatine fossa.
According to our observations, in most cases the cause of OPO is inflammatory processes in the ethmoidal labyrinth, which occurred in 100 (41.5%) cases. Involvement of the maxillary sinus in the inflammatory process was observed in 70 (29%) cases, the frontal sinus in 50 (20.7%), and the sphenoid sinus in 21 (8.7%).
Thus, the pathogenesis of OPO in sinusitis is direct contact with an infectious agent (often with congenital defects of the orbital walls), bacterial phlebitis, or penetration of bacteria through perivascular pathways.
Classification of ORO.
B.V. Shevrygin and N.I. Kuranov in 1976 proposed a classification that included: 1) reactive edema of the tissue of the orbit and eyelids; 2) diffuse non-purulent inflammation of the tissue of the orbit and eyelids; 3) periostitis of the orbit; 4) subperiosteal abscess; 5) eyelid abscess; 6) fistulas of the eyelid and orbital wall; 7) retrobulbar abscess; orbital phlegmon; 9) thrombosis of veins of the orbital tissue. This classification is the most complete and allows for a more thorough development of statistical materials about ORO and recording of long-term results.
Shevrygin and N.I. Kuranov in 1976 proposed a classification that included: 1) reactive edema of the tissue of the orbit and eyelids; 2) diffuse non-purulent inflammation of the tissue of the orbit and eyelids; 3) periostitis of the orbit; 4) subperiosteal abscess; 5) eyelid abscess; 6) fistulas of the eyelid and orbital wall; 7) retrobulbar abscess; orbital phlegmon; 9) thrombosis of veins of the orbital tissue. This classification is the most complete and allows for a more thorough development of statistical materials about ORO and recording of long-term results.
We observed various forms of OPO. Thus, reactive edema of the eyelids was detected in 16 (14%) cases, reactive edema of the eyelids with orbital edema in 22 (19.3%) cases, serous (non-purulent) inflammation of the orbital tissue (orbital cellulitis) was noted in 13 (11.4% ) sick. Purulent inflammatory processes in the orbit predominated both in acute (25 (54.3%) and chronic purulent sinusitis (38 (55.9%). The most common purulent complications were subperiosteal and orbital (retrobulbar) abscesses (in 25 (55.9%). 21.9%) and 19 (16.7%) cases, respectively). Orbital phlegmon was detected in 12 (10.5%) cases, eyelid abscess in 7 (6.1%) cases.
Clinical symptoms
The clinical symptoms of OPO consist of manifestations of a purulent inflammatory process in the paranasal sinuses and inflammation from the orbit. Common symptoms include weakness, headache, general malaise, low-grade or febrile body temperature.
From the side of the nasal cavity and paranasal sinuses, as a rule, there is difficulty in nasal breathing, a feeling of nasal congestion, lack of smell, and nasal discharge of a purulent or mucopurulent nature. Along with these symptoms, headache, a feeling of heaviness or pressure in the projection of the affected sinus are noted.
According to the data of an otorhinolaryngological study, patients with ORO experience pain upon percussion of the projection sites of the paranasal sinuses and pain at the exit points of the trigeminal nerve. The main pathognomonic sign of purulent sinusitis that caused OPO is a strip of purulent or mucopurulent discharge under the middle turbinate, however, this symptom in 36.1% of cases may be absent due to a violation of the patency of the anastomosis of the paranasal sinus involved in the purulent-inflammatory process. Swelling and hyperemia of the nasal mucosa also occur in other inflammatory diseases, so they cannot be considered reliable symptoms of paranasal sinusitis.
Signs of an early inflammatory reaction from the orbit are swelling and hyperemia of the eyelids, pain in the eye, purulent nasal discharge and increased body temperature. If the inflammatory process continues to develop further, then ptosis, exophthalmos, chemosis and limited mobility of the eyeball up to complete ophthalmoplegia appear, which are signs of a purulent process in the retrobulbar area (abscess or orbital phlegmon). These signs already indicate inflammation of the soft tissues and possible thrombosis of the orbital veins. The further course of inflammation leads to thrombosis of the cavernous sinus, which is characterized by a fairly rapid spread of inflammation to the other eye, intracranial complications (meningitis, brain abscess), visual impairment - diplopia, decreased visual acuity, blindness.
Exophthalmos, as a symptom of orbital disease, occurs with inflammation, trauma, tumors and may be the first clinical sign of ongoing orbital orbital disease. Chemosis, as a rule, is characteristic of purulent inflammatory processes in the orbit, both preseptal in relation to the tarso-orbital fascia and post-septal localization.
The location of the purulent focus in the anterior cells of the ethmoid labyrinth is accompanied by swelling of the inner corner of the eye, dacryocystitis, and chemosis of the inner half of the conjunctiva of the eyeball. In the case of the presence of a purulent focus in the posterior cells of the ethmoid labyrinth and the sphenoid sinus, central scotoma, paralysis of the III, IV and VI pairs of cranial nerves, and an increase in the blind spot are characteristic.
The inflammatory process in the tissues of the orbit leads to an increase in orbital tone, which disrupts the physiological drainage of fluid in the venules and capillaries, as a result of which hydrostatic pressure increases, which causes venous congestion in the eyeball and, as a result, pseudoedema of the optic disc occurs.
The closer the focus of inflammation is to the eyeball, the higher the likelihood of an ophthalmological picture. In this regard, the following appear in the fundus: swelling, hyperemia of the optic nerve, hemorrhages, changes in the caliber of blood vessels. Inflammation and swelling of the optic nerve lead to its compression in the bone canal, the diameter of which is 4 - 5 mm, and the nerve itself without membranes is 3 mm.
The most dangerous thing is that the optic nerve and main vessels get into the center of the inflammatory process. This circumstance explains the more frequent occurrence of blindness with phlegmon than with orbital abscess.
Of the orbital complications of inflammatory diseases of the paranasal sinuses, diseases of the walls of the orbit and retrobulbar tissue are the most frequent and better studied, while damage to the eyeball and optic nerve is observed less frequently. Of the diseases of the eyeball, damage to the connective tissue and cornea is primarily worthy of attention.
Panophthalmitis - inflammation of all tissues and membranes of the eye - occurs more often as a result of exogenous infection when the eyeball is injured, but metastatic infection is also possible. The primary focus of inflammation can be localized not only in distant organs, but also in the neighborhood, in particular the paranasal sinuses. Severe cases of panophthalmitis lead to atrophy of the eyeball and, naturally, to complete loss of vision in that eye. In addition, panophthalmitis is dangerous due to the possibility of developing intracranial complications with a fatal outcome when the infection spreads through the vessels into the cavernous sinus. In case of recovery, paresis of the III, IV and VI pairs of cranial nerves remains.
Diagnostic methods for ORO.
In the diagnosis of OPO, the most important role is played by the x-ray method. In most cases, using standard radiography of the paranasal sinuses in a direct frontonasal or chin-nasal projection, in a vertical position and, in the presence of homogeneous darkening in the sinus, in order to differentiate the exudative form from neoplasms of the paranasal sinuses, in a horizontal position, as well as an image of the skull in oblique projection, we can conclude that there is a pathological process in the paranasal sinuses and orbit.
It should be noted that the number of cases of discrepancy between the X-ray report and pathological intraoperative changes in the paranasal sinuses during ORO ranges from 12.5% to 27.3%.
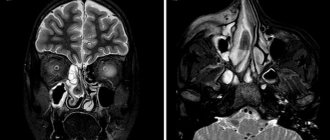
X-ray computed tomography has significantly increased the level of diagnosis of AGS, CHC and ORO. The advantage of CT is the absence of summation of shadows due to multiplanar reconstruction of the obtained images using a computer and, as a result, visual determination of the spatial relationships of the pathological process in the paranasal sinuses and adjacent anatomical structures. Densitometry makes it possible to indirectly judge the nature of pathological changes in the inflammatory focus. As a rule, CT scan of the paranasal sinuses during ORO is performed in the coronal and axial projections, in exceptional cases - in the sagittal.
CT is used for the purpose of differential diagnosis of inflammatory edema of orbital tissue and its purulent melting, assessment of the condition of retrobulbar structures after sanitation of the paranasal sinuses, which did not lead to an improvement in the clinical picture, to identify a tumor or cystic process, to establish pathological changes in the sphenoid sinus and in the posterior parts of the ethmoid labyrinth .
Based on the degree of decrease in airiness of the paranasal sinuses, weak homogeneous darkening, intense homogeneous darkening, inhomogeneous darkening, marginal decrease in airiness of the paranasal sinuses, horizontal fluid level, and the presence of a space-occupying formation are determined.
In the “bone” mode, CT scans determine the presence of blurred contours of the orbital bone wall, the presence of destruction in the form of defects, and discontinuity of the contour.
Depending on the form of the orbit, different severity of pathological changes in the orbit is noted. In patients with reactive edema of the eyelids, CT shows changes characteristic of the inflammatory process in the preseptal region, while in the postseptal region there is no increase in density and, on average, it ranges from - 120 to - 100 HU. Visual acuity and mobility of the eyeball are not impaired.
Among patients with eyelid edema and retrobulbar edema, thickening (edema) of the eyelids, exophthalmos, and increased orbital density during densitometry up to – 80 – 70 HU are most often noted on CT data.
The picture of orbital cellulitis (non-purulent inflammation in the orbit) is characterized by thickening of the eyelids, pronounced exophthalmos, an increase in density to 10 - 30 HU of a diffuse nature and can easily be mistaken for orbital phlegmon. The diagnosis is finally established during surgery, since these patients are indicated for surgical intervention.
CT scans of patients with clinical data of subperiosteal abscess indicate in all cases the presence of a formation of increased density (23–30 HU), adjacent to one or another orbital wall, delimited by an inflamed detached periosteum.
A retrobulbar abscess is characterized by pronounced thickening of the eyelids, a sharp displacement of the eyeball, and the presence of one or more foci of uneven increased density. The X-ray picture is complemented by changes in the optic nerve, which manifest themselves in thickening, “blurring” of contours; the nerve is not identified along its entire length, which indicates its involvement in the inflammatory process. The most common location of the abscess is between the medial rectus muscle of the eye and the optic nerve.
CT scans of orbital phlegmon are characterized by a clear, diffuse, heterogeneous increase in soft tissue density from 28 to 32 HU, displacement and deformation of the eyeball, and thickening of the optic nerve. In the paranasal sinuses, contents with a level of density corresponding to fluid or a total homogeneous decrease in transparency are determined, but in some cases of disorders, pneumatization of the paranasal sinuses on the side of the affected orbit is absent, which may indicate rhinogenic hematogenous or lymphogenous routes of infection of the orbit.
In all forms of OPO on computed tomograms, the radiological diagnosis of purulent inflammation in the paranasal sinuses coincides with the results of surgical interventions. In all cases of non-purulent ORO (reactive edema of the eyelids, reactive edema of the eyelids with intraorbital edema), the diagnosis on computed tomography can be established accurately, which allows one to avoid surgical intervention in the orbit.
According to our data, the most difficult thing in differential diagnosis with CT is to determine the purulent nature of inflammation in the orbit with orbital cellulitis and orbital phlegmon. In 11.4% - 15.3% of cases, computed tomograms can show signs resembling purulent inflammation in the orbit (increased densitometric density, blurred contours of the eye muscles, anterior displacement of the eyeball), but the final diagnosis can only be established by opening the orbit , in the absence of purulent discharge. The orbital tissue is swollen, the color is not light yellow, as is normal, but gray or with a hemorrhagic component.
In other cases of purulent inflammation in the orbit (subperiosteal abscess, orbital abscess, orbital phlegmon), the form of purulent inflammation according to the results of CT is established accurately, which allows you to choose the tactics of surgical intervention.
In case of AGS and CHC on computed tomograms, the localization of the purulent-inflammatory process in the paranasal sinuses practically coincides with the data of therapeutic and diagnostic punctures and the results obtained during operations.
During ORO, CT scans are used to identify various disturbances in the architectonics of the nasal cavity, which contribute to the emergence and development of the inflammatory process in the paranasal sinuses and its further spread into the orbit.
According to our data, hypertrophy, a low location of the ethmoid bulla, one of the most important components of the ostiomeatal complex, was detected by CT in 29 (44.6%) cases with orbital complications, which was significantly more often than with acute complications (14 (21.5%) %) and chronic (22 (33.8%) purulent sinusitis. Along with this, hypertrophy of the uncinate process with orbital complications was noted in 36 (42.4%) cases. This anatomical anomaly was noted in 19 (22.4%) cases in acute sinusitis and in 30 (35.3%) in chronic sinusitis, which was significantly less (p<0.01).
In a larger number of observations, inversion of the uncinate process was noted in orbital complications (16 (50%)) than in acute (6 (18.7%) and chronic purulent sinusitis (30 (35.3%). True hypertrophy of the inferior turbinate was more common in chronic sinusitis (71 (62.3%) than with orbital complications (32 (28.1%). It should be noted that even a study such as CT does not always fully reflect objective changes in the anatomy of the nasal cavity and finally determine various pathologically significant features anatomy is only possible during surgery.Depending on the form of the orbit, varying degrees of pathological changes in the orbit were noted.
An MRI study, in comparison with a CT scan, provides less information about the nature of the process in bone tissue, which is quite important in cases of OPO, AGS and CHC. One of the features of magnetic resonance imaging of the paranasal sinuses is the high sensitivity of the method to increased blood supply to the mucous membrane, which can lead to overdiagnosis of inflammatory changes.
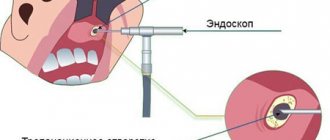
Endoscopic examination of the nasal cavity.
EI of the nasal cavity is one of the most informative intravital research methods, along with CT and MRI.
One of the main difficulties when performing EI of the nasal cavity is the curvature of the nasal septum. This feature of the anatomical disorder leads, according to our observations, to the diagnosis of a smaller number of combined deformities of the nasal septum due to the difficulty of examining the posterior sections on the side of the deviation of the nasal septum and the narrowing of the general nasal passage. Thus, in patients with ORO, combined curvature of the nasal septum was noted in 20.9% of cases. With CT, combined curvatures of the nasal septum were diagnosed more often than according to EI, which amounted to 23.9% of cases in patients with ORO. At the same time, isolated ridge-shaped deformities in the indicated main subgroups according to CT data were diagnosed with the same frequency as in EI.
During the endoscopic examination, we also paid great attention to the dimensions of the ethmoidal funnel, uncinate process, ethmoidal bulla, the state of the middle and inferior nasal conchae, the presence of opposing surfaces, upon closure of which, according to H. Stammberger et al. (1990), the movement of the cilia of the ciliated epithelium is blocked, the aeration of the paranasal sinuses is disrupted, which leads to stagnation of the secretion of the mucous membrane and the development of inflammation.
In 21.7% of cases with OGS, in 33.3% of cases with CHC, hypertrophy of the ethmoid bulla was noted, which was significantly less than with ORO (44.9%).
Hypertrophy of the uncinate process was noted according to endoscopic examination in OGS and CGS in 20.5% and 36.4% of cases, which was significantly less common than in OPO (43.2%).
True hypertrophy of the middle turbinate was observed in 13.5% of cases with AGS, and in 32.4% of cases with CHC. In 48.6% of cases, the indicated anomaly in the development of this most important component of the ostiomeatal complex was noted in orbital complications.
Also, as in the case of true hypertrophy, bullous deformation of the middle turbinate was determined by endoscopic examination in OPO in 44.1% of cases, which was significantly more than in OGS (23.5%) and CHC (32.4%) .
Inversion of the uncinate process, which usually accompanies bullous hypertrophy, is also detected in a larger number of cases with ORO.
Thus, both with CT and with EI of the nose, we noted in a greater number of cases the presence of various disorders of the intranasal anatomy in ORO than in OGS and CHC, which aggravate its course and ultimately lead to the spread of the purulent-inflammatory process into the orbit.
These two methods are complementary; in particular, CT makes it possible to assess the condition of the posterior parts of the nasal cavity, which are inaccessible to the endoscope due to severe violations of the nasal septum. EI has a higher diagnostic value in determining the state of the ostiomeatal complex due to direct visualization of the complex as a whole.
Surgical treatment of ORO.
According to modern views on the treatment of this pathology, sanitation of a purulent focus in the orbit without surgical intervention in the paranasal sinuses, and in some cases in the nasal cavity, cannot guarantee a speedy recovery and the absence of relapses in the future.
Most often, in the treatment of paranasal sinusitis and ORO, radical operations on the paranasal sinuses are used in combination with ethmoidotomies and wide opening of the orbital cavity.
Most domestic authors in the treatment of chronic purulent sinusitis and orbital rhinosinusogenic complications in the case of damage to the maxillary sinuses give preference to operations using the Caldwell-Luc, Ivanov, Denker method; when purulent frontal sinusitis is combined with ethmoiditis or sphenoiditis - according to the method of Belogolov, Killian, Riedel, Jansenne-Ritter, Kunta, Jansenna – Winkler. It is almost impossible to assess the advantages or disadvantages of individual methods of surgical intervention; each of them has its own indications, depending on the extent of the process and the anatomy of the paranasal sinuses.
The negative aspects of using these surgical operations are high trauma, the risk of damage to the lacrimal sac, a cosmetic defect in the form of a scar, the likelihood of obliteration of the nasofrontal anastomosis in the postoperative period after radical removal of its lateral wall, short-term diplopia as a result of resection of the frontal process along with the block. Long-term results of radical surgical techniques, assessed as recovery, according to various authors, are observed in 50 - 80% of cases. The leading cause of recurrence of chronic sinusitis after surgery is a violation of the patency of the artificial sinus anastomosis, which, in combination with fibrous postoperative changes, chronic unsanitized foci of infection, disorders of the intranasal anatomy, causes contact between the opposite surfaces of the mucous membrane, which leads to the maintenance of a chronic inflammatory process and disruption of the repair processes in the sinus. operated sinus.
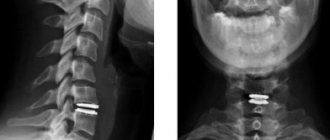
Operations performed through the endonasal approach are characterized by the absence of trauma to the soft tissues of the face and the absence of cosmetic defects. Functional endoscopic surgery on the paranasal sinuses with simultaneous orbitotomy for orbital cellulitis and purulent forms of complications began with the elimination of deformation of the nasal septum. Using CT or MRI, we determine the position of the patient’s medial wall of the orbit in the axial and coronal projections and determine the extent of the process. At the same time, during CT and MRI studies, we additionally select the site of perforation of the tissue plate and determine the volume of opening of the ethmoidal labyrinth. The more ventral location of the source of inflammation (superolateral, anterior lateral subperiosteal abscesses) determines the location of perforation of the tissue plate to the level of the terminal plate of the middle turbinate, opening the anterior part of the ethmoidal labyrinth. Involvement of the posterior sections of the ethmoidal labyrinth in the purulent-inflammatory process and the location of subperiosteal or retrobulbar abscesses more dorsally determines the opening of the anterior and posterior sections of the ethmoidal labyrinth, perforation of the medial wall of the orbit dorsal to the terminal plate.
Then we perform perforation of the medial wall of the orbit. Under endoscopic control, we displace the middle turbinate medially with a raspatory, and then, using an aggressive microdebrider cutter, we partially remove the middle part of the uncinate process and the ethmoid bulla. In this case, if the source of inflammation is localized behind the terminal plate of the middle turbinate, we additionally open the posterior cells of the ethmoidal labyrinth and the sphenoid sinus.
Under endoscopic control, we perforate the tissue plate with a sickle-shaped knife in the direction from top to bottom, from front to back, as medially as possible in relation to the medial wall of the orbit. At the same time, we ensure that the knife blade penetrates into the orbital cavity by no more than 2–3 mm, the length of the incision is 1–1.5 cm, and at the same time we open the orbital periosteum with the bony part of the medial wall. We insert a strip of latex rubber 5 mm wide and 20 mm long into the orbital cavity through the wound. Then we insert into both halves of the nasal cavity arch-shaped stents made of lamellar silicone, customized individually for the patient, with a round window with a diameter of 1.5 cm, which is cut into the silicone at the level of the middle nasal passage, glove drainage is brought out through the window into the vestibule of the nose, then The stent is fixed through the nasal septum with a single interrupted suture. The stents are removed on the 3rd day after surgery.
As a rule, this intervention is complemented by transpalpebral orbitotomy.
The use of HBOT in the treatment of ORO.
In order to accelerate the repair processes, reduce the severity of the inflammatory process and intoxication syndrome, we performed hyperbaric oxygenation sessions in patients with OPO on days 2–3 after surgery.
Before the first HBO session, under endoscopic control, an examination of the nasal passages and outlet openings of the anastomoses of the paranasal sinuses is performed, removing crusts if they are present, followed by anemization of the mucous membrane. Along with this, it is necessary to check the function of the auditory tubes using Toynbee maneuvers, Valsalva maneuvers and tympanometry.
The first sessions must be carried out at maximum pressure at a compression height of up to 0.8 ata, the second sessions up to 1.2 ata. Starting from the 3rd session, the pressure in the pressure chamber can be increased to 1.3 atm. This is facilitated by an improvement in both the general condition of the patient at the beginning of the 3rd session and a decrease in the severity of inflammatory changes in the nasal cavity and nasopharynx, which improves the barofunction of the paranasal sinuses and the patency of the auditory tubes. The duration of sessions should also be selected individually; the recommended effective duration for the first session is up to 40 minutes, subsequently up to 70 minutes.
In order to prevent barotrauma, all patients are treated with local vasoconstrictor drugs before trial sessions; in extreme cases, when the patient has concomitant chronic exudative otitis media, the tympanic membrane of the diseased ear is shunted before HBOT.
Application of regional indirect endolymphatic therapy
in the treatment of orbital rhinosinusogenic complications.
According to the results of the experimental study, we modified the method of regional indirect endolymphatic administration of antibiotics proposed by A. Alimov and K. Kasimov (1991). Patients with AGS, CHC and OPO were injected subcutaneously into the projection of the submandibular lymph node with 8-12 units of lidase dissolved in 3-5 ml of 0.25% novocaine solution. Without removing the needle, half a single dose was administered in 2 ml of saline after 3–5 minutes. Antibacterial drugs were administered according to the standard regimen for each antibiotic with the following modification: the first single dose, for example, cefotaxime, was divided in half, half of it was administered regionally lymphotropically, and the second part intramuscularly or, in case of orbital rhinosinus complications, intravenously. Further administration of the antibacterial drug was carried out according to the standard regimen with the frequency of administration specified in the recommendations for use. After administration, the patient is given a semi-alcohol compress on the submandibular area for 3 hours in order to enhance the effect of lymphostimulation.
Recommended doses and regimens of administration of antibacterial drugs for orbital rhinosinusogenic complications.
| Antibiotics | Administration modes |
| Cefuroxime | 0.75 regionally lymphotropic + 0.75 IM or IV in the morning, then 1.5 at lunchtime and in the evening IM or IV. |
| Cefotaxime | 1.0 regionally lymphotropic + 1 g IM or IV in the morning, then 2.0 in the afternoon and evening IM or IV. |
| Ceftriaxone | 1.0 regionally lymphotropic + 1.0 IM or IV 1 time per day. |
| Cefoperazone | 1.0 regionally lymphotropic + 1 g IM or IV in the morning, then 2.0 in the afternoon and evening IM or IV. |
| Ceftazidime | 1.0 regionally lymphotropic + 1 g IM or IV in the morning, then 2.0 in the afternoon and evening IM or IV. |
| Cefepime | 1.0 regionally lymphotropic + 1 g IM or IV in the morning, then 2.0 in the evening IM or IV. |
| Amoxicillin/clavulanate | 0.6 regionally lymphotropic + 0.6 IM or IV in the morning, then 1.2 in the afternoon and evening IM or IV. |
| Imepenem | 0.25 regionally lymphotropic and 0.25 IM or IV in the morning, then 0.5 x 2 times on the same day IM or IV. |
| Meropenem | 0.25 regionally lymphotropic and 0.25 IM or IV in the morning, then 0.5 x 2 times on the same day IM or IV. |
Fig.1. Treatment and diagnostic algorithm for patients with acute and chronic purulent sinusitis and orbital rhinosinus complications using computed tomography, functional endoscopic rhinosinus surgery, RNET and HBOT.