If you go to the mirror and open your mouth wide, you can see two formations that are located on the side surfaces, in the depths of the pharynx, which are shaped like an almond. This is why the tonsils are called tonsils. And since the tonsils are located in the soft palate, they are called palatine tonsils.
Also, in common parlance, the palatine tonsils are also called tonsils. They are one of the important organs of the pharyngeal immune system and form an important part of the Pirogov-Waldeer lymph-epithelial pharyngeal ring.
Palatine tonsil, tonsila palatina. It is located in the tonsillar fossa between the palatoglossus and velopharyngeal arches.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
What other tonsils are there in the pharynx?
Other tonsils that form the lymphoid pharyngeal ring are: adenoid vegetations, or, more simply, adenoids, which are not a paired organ. They are located in the dome of the nasopharynx. It is impossible to see them with the naked eye. In order to recognize the condition of the adenoids, it is necessary to perform an endoscopic examination of the nasopharynx. Inflammation of the adenoids is called adenoiditis and is more common in children.
Also in the pharynx there is a lingual tonsil, located at the root of the tongue, which, like the adenoids, is an unpaired organ.
There are also tubal ridges, which are also called tubal tonsils. They are located at the entrance to the pharyngeal mouth of the auditory tube. The tube ridges are located deep in the nasopharynx, on the lateral (medial) surfaces of the nasopharynx on the right and left. Tubal tonsils perform an important function - they protect against infection entering the auditory tube. Since each of the tonsils of the lymphoepithelial pharyngeal ring deserves separate close attention, in this article we will only talk about the palatine tonsils and chronic tonsillitis. Other tonsils and the pathology they cause will be described in detail separately, in other relevant ENT articles.
Complications after tonsillectomy
The most common complication is bleeding from the tonsillar niches, mainly in the early postoperative period in the presence of concomitant diseases;
bleeding can be vascular and parenchymal. Vascular bleeding is stopped with hemostatic clamps followed by ligation of the vessel. In case of parenchymal bleeding, the niche is tamponade with hemostatic agents (if it is necessary to hold the tampon for a long time in the niche above it, the palatine arches are sutured). Other complications are extremely rare: subcutaneous emphysema, acute inflammation of the lingual tonsil, stomatitis, glossitis, acute otitis media, exacerbation of chronic diseases of the ENT organs, exacerbation of chronic diseases of the internal organs, phlegmon of the neck, paresis of the cranial nerves, pharyngeal hematoma. [/td]
Read more about tonsils
It must be said that the palatine tonsils are the largest lymphoid formations of the entire pharyngeal ring, and they play, perhaps, the leading role in the disposal of bacterial and viral infections that enter the pharynx by airborne droplets.
Due to their size, the palatine tonsils are the first to stand in the way of microbes that enter the oral cavity from the external environment, and protect the body from infection by viruses, bacteria, spirochetes, protozoa and other microorganisms.
The palatine tonsils have depressions - lacunae, which in turn are exit holes for deep and sharply convoluted canals - crypts, which are located in the thickness of the palatine tonsil, leading to its root. The number of lacunae and crypts can vary from 1 to 14, but on average, in each amygdala there are from 4 to 7 lacunae. The diameter of the lacunae can also vary, depending on gender, age, individual characteristics of the patient, as well as the duration and severity of the disease and the presence of scar changes in the tonsils themselves.
It is believed that the wider the exit hole - the lacuna - the higher the likelihood of the palatine tonsil to self-cleanse. This statement is true. Accordingly, the smaller the diameter of the lacuna, the more pronounced and severe the tonsillitis. Moreover, if the tonsil produces a large amount of caseous-necrotic detritus (plugs), the severity of the course also noticeably increases.
Normally, on the mucous membrane of the palatine tonsils, as well as in the thickness of the palatine tonsils, in the lacunae and crypts, there is a growth of non-pathogenic and conditionally pathogenic microflora, in normal (permissible) concentrations. If there are more microorganisms (for example, due to intensive growth, or the addition of other pathogenic microflora from the outside), the palatine tonsil immediately destroys and utilizes the dangerous infection and normalizes a dangerous condition for the body. At the same time, the macroorganism, that is, the person, does not notice this in any way.
The tissues of the palatine tonsils produce the following main protective substances: lymphocytes, interferon and gamma globulin.
The palatine tonsils act as a serious infectious and inflammatory barrier and are an important component in creating not only local, but also general immunity in the human body. Therefore, when it comes to removing the palatine tonsils, you first need to think ten times, weigh the pros and cons, and only after that make a decision about removing the tonsils.
Treatment of sore tonsils in adults
Most often, inflammation can be dealt with at home. However, if the lingual tonsil is affected, hospitalization is always required.
Self-therapy can only be carried out if a person is firmly convinced that the inflammation has a viral basis. A bacterial infection requires contacting a doctor, as it poses a danger to the patient’s health. Treatment boils down to taking medications that are aimed at eliminating the causative agent of inflammation. In addition, efforts need to be directed towards making a person feel better. This treatment is called symptomatic.
If a person decides to cope with inflammation on his own, but after 3 days there is no improvement, then he should consult a doctor.
Recommendations to speed up recovery:
- You need to drink as much fluid as possible. In addition to water, it is good to drink tea, compotes, broths, and fruit drinks.
- During the acute phase of the disease, a person must adhere to bed rest.
- There is no need to force yourself to eat. Food is consumed as appetite appears.
If the disease is complicated by suppuration, which cannot be relieved at home, the person is recommended to wash the tonsils in the ENT office.
Removal of tonsils is rarely done. Surgery is required only when all conservative methods have proven ineffective. Patients with chronic tonsillitis and adenoiditis may also need the help of a surgeon.
Medication correction
If the inflammation of the tonsils is of a viral nature, then it will be possible to limit oneself to symptomatic therapy; it is recommended to take antiviral drugs that have a local immunomodulatory effect. The body must cope with the infection on its own. You just need to help him a little.
For this purpose, drugs such as:
- Sore throat sprays and cough drops. Effective drugs are: Strepsils, Septolete, Ingalipt, Chlorophyllipt, Givalex, Tantum Verde, Lizak, Lizobakt, Faringosept, Throat spasm, etc. These drugs have not only an analgesic, but also an antiseptic effect.
- Gargles: Angilex, Chlorophyllipt, Furacilin, Streptocide, Rotocan, Givalex, etc. The more often a person performs this procedure, the faster the recovery will occur. Gargling allows you to remove not only viral flora from the tonsils, but also pus, as well as dead tissue.
- Drugs to reduce body temperature: Panadol, Nurofen, Nimesil, Efferalgan, Nise, etc.
If the inflammation was caused by microbial flora, then it can only be dealt with using antibiotics for a sore throat. Taking them helps prevent the development of complications. The drug must be recommended by a doctor. The dose is selected depending on the severity of the infection. For local therapy, agents with an antibacterial component are used, such as: Polydexa, Isofra, Rinil. If they do not achieve the desired effect, then the patient is advised to take systemic antibacterial drugs. These may be drugs such as: Augmentin, Flemoxin, Amoxiclav, Amoxicillin, Vilprafen, etc.
In order to avoid relapses, antibacterial drugs are taken in full course. The patient needs to complete treatment, even if he feels better after a couple of days of taking medications.
If more than 3 days have passed since the start of antibacterial therapy and there is no effect, then it is necessary to change the drug. This means that the pathogenic flora has resistance to it. In the future, tetracyclines (Tetracycline, Doxycycline, Unidox Solutab, etc.) or macrolides (Sumamed, Hemomycin, Azithromycin) can be used.
Taking a smear from the throat allows you to identify the representative of the pathogenic flora that caused the inflammation and determine which drugs it responds to. However, the results of the LHC culture will be known no earlier than in 5-7 days. Delaying treatment for such a long period of time can be dangerous. Bacterial inflammation, as well as a viral infection, requires symptomatic therapy with mandatory gargling.
Treatment of inflamed tonsils in children
Treatment of inflamed tonsils in children should be pathognomic, that is, aimed at eliminating the cause of the disease.
- If a child has an acute respiratory viral infection, then he needs to treat his throat, lower his body temperature, and give painkillers.
- A bacterial infection requires consultation with a pediatrician. The doctor must select the antibiotic.
- Adenoiditis takes longer to cure than other diseases. To carry out therapy, they resort to corticosteroid drugs (Flicosnase, Nasonex). Vasoconstrictor nasal drops (Nazivin, Xylometazoline, Rinazoline) are also used. To combat pathogenic flora, agents such as Protargol, Collargol, etc. can be used.
For the disease to lead to serious complications, parents should consult a doctor in the following situations:
- Body temperature remains high, even after taking antipyretic medications.
- White plugs or white plaque are visible on the tonsils.
- The child coughs a lot.
- Nasal discharge is yellow-green in color.
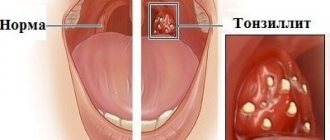
Chronic tonsillitis
Chronic tonsillitis is an autoimmune disease that occurs as a result of frequent sore throats and a decrease in the body’s overall resistance since childhood. With the development of the disease and its exacerbation, a person does not have enough general immunity to keep the palatine tonsils “in working order” and adequately fight the infection.
If harmful microbes get onto the surface of the mucous membrane and into the lacunae of the palatine tonsil, a real battle occurs between the microbes and the human immune system.
The palatine tonsil fights all pathogenic and conditionally pathogenic infections, but not being able to fully resist attacking microbes, it provokes either a new outbreak of sore throat or an exacerbation of chronic tonsillitis (treatment cannot be delayed in any case), thereby triggering an infectious-inflammatory process in palatine tonsils.
As a result of a lost fight, pus accumulates and stagnates in the lacunae of the tonsils, that is, dead leukocytes that come to the aid of the tonsil in the fight against a dangerous infection. The purulent masses irritate and inflame the tonsil tissue from the inside and have a toxic effect on it, thereby causing a sore throat - a severe infectious outbreak of inflammation of the tonsils.
In the absence of quick and adequate treatment, the contents of the lacunae and crypts of the palatine tonsils serve as a breeding ground for pathogenic microbes and a constant source of infection, even after an attack of tonsillitis.
How is inflammation treated?
The tactics for treating enlarged tonsils in a child consists of treating the underlying disease that caused this symptom (taking antibiotics, antiviral or antifungal drugs), and influencing them directly to regenerate the affected tissues. The latter includes:
- washing the tonsils from pathogenic microorganisms and mucus with antiseptic solutions;
- reducing swelling - taking antihistamines and ultraviolet irradiation;
- UHF therapy, which improves blood microcirculation;
- exposure to ultrasound to free the lacunae of the tonsils from pus, which can accumulate in them;
- laser exposure to destroy infection and its pathogens.
Forms of the disease
- recurrent form, that is, with frequently recurring sore throats;
- protracted form, when the inflammatory process in the palatine tonsils is characterized by a sluggish and prolonged course;
- compensated form, when episodes of sore throat and exacerbation of tonsillitis are not observed for a long time.
Chronic tonsillitis is the most common disease among all diseases of the pharynx and one of the most common diseases of all ENT organs, along with such a diagnosis as acute sinusitis.
Chronic tonsillitis can affect both adults and children, from the moment the palatine tonsils begin to develop (from 2-3 years). Moreover, the incidence of this disease in childhood is much higher.
Some respiratory diseases can also be classified as social diseases. For example, sinusitis and tonsillitis are among them. Poor environment, stress, lack of sleep, overwork, monotonous and poor nutrition, as well as poor heredity are predisposing factors to the development of the disease.
Stages of the disease
The staging of tumors with intracellular DNA inclusions of human papillomavirus type 16 (16HPV) and without it differs.
For virus-negative neoplasms, everything is simple:
- Stage 1 - local formation up to 2 cm, without metastases in the lymph nodes;
- 2 tbsp. - tumor less than 4 cm and lymphatic collector without signs of cancer;
- 3 tbsp. - neoplasm more than 4 cm with “clean” lymph nodes or less and there is a node up to 3 cm;
- 4 tbsp. suggests either a primary tumor of any size with distant metastases, or a very widespread lesion of the oropharynx with a large conglomerate of lymph nodes on the same side, or a not very large cancerous node with lymph nodes on the opposite side of the neck.
When staging papillomavirus cancer in stages 1 and 2, metastatic lymph nodes are possible, and stage 4 - only with distant metastases from any tumor and lymph nodes.
Causes
The development of the disease is closely related to frequent sore throats (acute tonsillitis). Very often, incompletely cured tonsillitis leads to chronic tonsillitis. Very often, tonsillitis is an exacerbation due to the accumulation of plugs in the tonsils - caseous-necrotic masses, which are often confused with food debris.
Main reasons for development
- Unfavorable working conditions. The greatest influence is exerted by gas and dust levels in the air at work.
- Poor environmental conditions, pollution from vehicle exhaust gases, harmful emissions into the atmosphere.
- Low quality of consumed water.
- Weak (low) immunity.
- Severe hypothermia of the body.
- Stressful situations.
- The presence of chronic diseases in the nasal cavity, paranasal sinuses and oral cavity - dental caries, purulent sinusitis, etc., which often leads to infection of the tonsils.
- Irrational or poor nutrition, in which excess amounts of proteins and carbohydrates are consumed.
- Heredity (mother or father suffers from chronic tonsillitis). It is very important for a woman to undergo one or two courses of treatment for tonsillitis during pregnancy (depending on the severity of the process) in order to minimize the likelihood of the disease developing in the unborn child.
- Frequent overwork, fatigue syndrome, inability to fully rest.
- Smoking and alcohol abuse.
Acute tonsillitis: treatment
Treatment of acute tonsillitis lasts seven to ten days and takes place at home according to the therapy prescribed by the otolaryngologist.
The patient needs strict bed rest and dietary adjustments. Since the throat hurts unbearably during a sore throat, food should not injure the throat: it should not be very hot or cold, too spicy or hard. It is ideal to eat pureed foods, and do not forget to drink plenty of fluids.
In the patient's room, it is necessary to maintain conditions conducive to rapid recovery: ventilate the room more often and carry out wet cleaning.
You also need to remember that sore throat can easily be contracted through the patient’s personal items, so if someone in the family has a sore throat, you should not share the same dishes, towels, etc. with the patient.
Drug therapy includes taking antibiotics. An antibacterial drug can only be prescribed by an ENT doctor. It is necessary to take the full course of the medicine, even if it has become easier and it seems that your throat no longer hurts. Incomplete treatment can cause chronic inflammation and other complications.
The temperature with a sore throat needs to be brought down with antipyretic drugs. When your throat hurts due to a sore throat, you should stock up on anti-inflammatory sprays, antiseptic gargles, lozenges and lozenges with an anesthetic effect. If you follow all the instructions of the ENT doctor, the sore throat goes away quickly enough and recovery occurs.
Symptoms
How to independently recognize chronic tonsillitis? Symptoms and treatment in adults and children can only be correctly determined by an ENT doctor. Below are characteristic signs - if you find them in yourself, consult a doctor.
The disease is characterized by symptoms such as:
- Headache.
- Feeling of something foreign in the throat, as if something was stuck in the throat. In fact, this is nothing more than large accumulations of caseous masses, that is, plugs in the thickness of the palatine tonsils.
- Increased fatigue, weakness, decreased performance. All this is due to the so-called tonsillogenic intoxication, or in other words, intoxication syndrome.
- Aching pain in the joints and muscles (with severe illness).
- Aching pain in the heart, with interruptions in heart function - extrasystole (with severe illness).
- Pain in the lower back, in the kidney area (with severe disease).
- Bad mood, and in some cases increased body temperature, and for a long time.
- Persistent skin rashes, provided that there was no previous skin pathology.
All these symptoms appear due to the entry of waste products of microorganisms into the blood from the palatine tonsils, i.e. staphylococcal and streptococcal infections, poisoning the entire body.
Bad breath appears due to the accumulation of organic substances and the decomposition of bacterial infection in the lacunae (recesses of the tonsils) and crypts (their canals). Tonsils become a source of bacterial infection, which can spread throughout almost the entire body and cause inflammation of the joints, myocardium, kidneys, paranasal sinuses, prostatitis, cystitis, acne and other diseases.
If the tonsils do not cope with their function as an immune organ, then even slight overwork, stress, or mild hypothermia can significantly reduce the immune defense and open the way for microbes and exacerbation of the disease.
Symptoms of inflammation of the tonsils
Symptoms characterizing the inflammatory process in the tonsils may vary, although slightly.
Common signs of the disease include:
- Increase in body temperature to high levels.
- Swelling of the mucous membrane of the oropharynx, hyperemia of the mucous membranes.
- Cough.
- Runny nose. With angina, this symptom is most often absent.
- General physical weakness.
If a person is infected with herpetic sore throat, then in addition to a sore throat and high body temperature, he experiences discomfort in the abdomen, and a small rash that looks like blisters is noticeable on the tonsils and back wall of the throat. They contain liquid. In the future, it can become purulent. After opening the blisters, the affected areas become covered with crusts.
If a person has an inflamed lingual tonsil, this is manifested by the following symptoms:
- The tongue swells and it hurts for a person to move it.
- When chewing and swallowing food, severe discomfort occurs.
- Pain forces a person to change his speech, as intense movements of the tongue become impossible.
Sometimes the patient notices that his tonsils are inflamed, but does not experience pain. This symptom may indicate chronic tonsillitis.
The temperature remains within normal limits, as the immune system stops making efforts to fight the source of infection.
Inflammation of the tonsils
More often than other tonsils, it is the tonsils that suffer in people. The most common pathology is acute or chronic tonsillitis. This disease becomes dangerous for humans if there is no treatment. The therapy must be selected by a doctor; this is the only way to make it effective.
The success of treatment is determined by its focus. To do this, you need to know which microorganism caused the inflammatory reaction. For this purpose, the doctor prescribes a bacteriological examination of a throat smear. When the analysis is ready, the doctor will be able to select the optimal therapy.
Unilateral inflammation of the tonsil
If the infection affects the tonsil on one side, this indicates activation of local immunity. He dealt with the pathogenic flora on one of the tonsils on his own and is able to maintain its health.
Sometimes unilateral inflammation is a sign of facial neuritis, lymphadenitis or other disorders that are not associated with otolaryngological diseases.
Unilateral inflammation requires treatment, which is selected in accordance with the causes of the disease.
Complications
Chronic tonsillitis is very dangerous due to rapidly occurring complications. The most severe of them are heart disease - myocarditis, inflammation of the joints - rheumatism and serious kidney damage - glomerulonephritis.
Some toxins that are produced by microbes in the tonsils and then enter the bloodstream can damage cartilage and ligament tissue. The result is inflammation and pain in the muscles and joints. Other toxins often cause persistent fever, changes in blood tests, fatigue, depression, and severe headaches.
Chronic tonsillitis can affect the functioning of such a vital organ as the heart. The tonsils are often parasitized by group A beta-hemolytic streptococcus, the protein of which is very similar to the protein found in the connective tissue of the heart. Because of this, the immune system can show retaliatory aggression not only to the emerging streptococcus, but also to its own heart. As a result, heart rhythm disturbances, heart valve prolapses, and even the development of severe myocarditis and bacterial endocarditis occur.
For the same reason, articular surfaces and kidney tissue are at great risk. Unfortunately, the development of diseases such as rheumatoid arthritis and glomerulonephritis is extremely high.
Due to the fact that the source of infection remains in the tonsils for a long time, a distortion of the body’s reactivity occurs, resulting in allergic changes. In some cases, just one course prescribed by a doctor can get rid of itching and allergic rashes, and in some cases stop the development of bronchial asthma attacks.
Complications of tonsil cysts
A cyst on the tonsil is a chronic source of infection that can behave in an unknown way, causing various complications. The neoplasm in the pharynx is constantly rubbed with food, which leads to the formation of a chronic inflammatory process. The longer the patient does not seek medical help, the longer the infection progresses; along with the bloodstream, infectious pathogens are carried to all cells and organs, disrupting their normal functioning.
A long-term infectious process is accompanied by general intoxication of the body. Toxins produced during the activity of pathogenic microorganisms disrupt the functioning of the liver and kidneys, provoke the development of chronic fatigue syndrome, reduce immunity and make a person vulnerable to even the most harmless infections.
Only an otolaryngologist can choose the treatment for a cyst on the tonsils, based on the results of pharyngoscopy. If the doctor suspects the development of a malignant process, a consultation with an oncologist will be required. Other studies may also be prescribed: rhinoscopy, audiometry, computed tomography and magnetic resonance imaging of the brain, otoscopy. In advanced cases, the tumor can grow into nearby tissues, including brain structures.
Chronic tonsillitis during pregnancy
It is very important to pay attention to the disease during pregnancy. When planning a pregnancy, even in the case of a compensated condition, that is, a condition outside of an exacerbation of tonsillitis, it is highly advisable to carry out a planned course as prescribed by a doctor. This will reduce the bacterial load on the entire body in general and on the palatine tonsils in particular.
It is very encouraging that doctors are now referring pregnant women and women who are just preparing for pregnancy for treatment of tonsillitis. Unfortunately, in some cases one of the reasons for not carrying a pregnancy to term is this disease, although at first glance it is hard to believe, tonsillitis is a traffic jam, the treatment of which and other manifestations may seem in no way related to pregnancy.
Before conceiving a child, it would be correct to examine the future father of the child for the disease and, if necessary, treat it as well. This will significantly reduce the risk of developing chronic tonsillitis in the unborn child. And, on the contrary, the worse the condition of the future father and especially the mother, the risk of developing the disease in the child increases many times over.
Before pregnancy, it is very important to carry out comprehensive treatment of the symptoms of chronic tonsillitis. But even during pregnancy, it is recommended to repeat the course, preferably in the second trimester, when the woman’s condition is perhaps the most comfortable. It is important to note that physiotherapeutic procedures cannot be carried out during pregnancy, but it is highly desirable to wash the palatine tonsils using a vacuum method, followed by treatment with antiseptic solutions.
Which doctor should you consult if you have inflammation of the tonsils?
The diagnosis and treatment of diseases of the tonsils is carried out by an ENT doctor, that is, an otolaryngologist. You should contact a specialist when the first symptoms of inflammation appear. However, few people rush to consult a doctor if their throat starts to hurt a little. It is possible that you will be able to cope with the disease on your own.
However, there are some conditions that require immediate medical attention:
- Body temperature reaches 38 °C and above. It lasts longer than 3 days.
- The person’s well-being deteriorates sharply.
- First there is an improvement, and then a deterioration in the condition.
- The child's tonsils become inflamed.
- Purulent foci of infection are visible in the throat.
The right approach
Sore throat, tonsillitis - treatment in children and adults is important to carry out immediately for all diseases of the oral cavity and nasopharynx that bother you. If breathing through the nose is impaired, and mucus or mucopurulent discharge flows down the back wall of the pharynx, then these symptoms should be given special attention.
Chronic tonsillitis - treatment (effective) can be conservative and surgical. Due to the fact that the removal of tonsils can cause serious harm to the defenses and immunity of the human body, otolaryngologists should try their best to preserve the tonsils and restore their functions without resorting to surgery to remove the tonsils. Modern methods of treating tonsillitis provide a greater chance of recovery without intervention.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Chronic purulent tonsillitis - treatment of a conservative type must always be carried out in an ENT clinic, performing a complex, pathogenetically based course of treatment, as well as using a medicinal approach - medications prescribed by an ENT doctor.
Treatment of tonsil cysts
Treatment of cysts can be either conservative or surgical. Often, specialists first prescribe effective drug therapy to relieve inflammation and prepare the patient for surgery. Conservative treatment of a cyst will not reduce its size, but can stop the active growth of the tumor and prevent complications. Treatment tactics should be selected by a competent specialist based on medical history, diagnosis and professional examination.
Conservative therapy for tonsil cysts includes the following measures and procedures:
- gargling with herbal decoctions, antiseptic solutions that disinfect tissues and have an anti-edematous and anti-inflammatory effect;
- physiotherapy: ultraviolet irradiation, massage, ultrasound - physiotherapeutic treatment methods are used to increase blood supply to tissues in the area where the tumor is located, to ensure lymph outflow;
- pumping out pus using hardware methods, which makes it possible to stop the development of the infectious process and the spread of infection to surrounding tissues;
- injection rinsing of the tonsils with anti-inflammatory drugs and antiseptics to cleanse plaque and purulent contents;
- strengthening the immune system with multivitamin complexes and immunostimulants;
- giving up bad habits that contribute to traumatization of the tonsils and the preservation of the chronic inflammatory process.
Some specialists practice opening the cyst and pumping out its contents. But, as a rule, the therapeutic effect does not last long and the tumor is filled with fluid again. Therefore, if the cyst has not disappeared after several weeks of active medical therapy, it is better to remove it surgically.
A complex approach
First stage
Viral tonsillitis - treatment with a good and pronounced effect is obtained by washing the lacunae of the palatine tonsils. There are two ways to wash the tonsils.
A very old method is to rinse the tonsils with a syringe. Previously, this method was widely used, but today it is used for lack of a better one or when the patient’s gag reflex is very pronounced.
The disadvantages of this method are that during the process of washing the palatine tonsils, the pressure created by the syringe is not sufficient to effectively wash out caseous masses from the lacunae of the tonsils. Also, this technique is contact and traumatic, since when using a straightened attic needle, its thin and sharp end can prick the inner surface of the palatine tonsil, namely the crypts - the channels into which the needle enters. Also, the tip from the set with a syringe is used for rinsing the tonsils and injecting into the larynx. On the contrary, it is very wide in diameter and injures the tonsil tissue when inserting the tip into the lacuna, or in general, due to the large outer diameter, it cannot always get there.
Practice has shown that today, the best results are achieved by the approach when the ENT uses the Tonsilor attachment.
First, it is necessary to rinse the lacunae of the palatine tonsils with a modified attachment of the Tonsilor apparatus with a transparent antiseptic solution, for example, saline solution (also known as isotonic sodium chloride solution). This is necessary so that the doctor can clearly see what he is washing out of the palatine tonsils.
Second phase.
Since the tonsils are washed from pathological secretions, it is necessary to immediately influence the tissues of the palatine tonsils with low-frequency ultrasound. At the same time, a medicinal solution passes through the ultrasonic tip of the “Tonsilor” apparatus, which, due to the ultrasonic effect of cavitation, turns into a finely dispersed medicinal suspension, which, due to hydraulic shock, hits the tissues of the palatine tonsil and the posterior wall of the pharynx with force and impregnates the medicinal solution into the submucosal layer of the tonsil.
The procedure for exposure to ultrasound is correctly called: Ultrasonic medicinal irrigation. In our clinic we use a 0.01% solution of Miramistin. This drug is good because it does not lose its properties under the influence of ultrasound. Miramistin is a very strong antiseptic drug, and ultrasound exposure further enhances the durability of the physiotherapeutic effect.
Third stage.
It is necessary to treat (lubricate) the palatine tonsils with Lugol's solution, which is also a strong antiseptic based on iodine and glycerin.
Fourth stage.
The otorhinolaryngologist at our clinic conducts a laser therapy session on the tissue of the palatine tonsils and the mucous membrane of the posterior pharyngeal wall. Laser treatment of tonsillitis in adults is very effective. Its action is aimed at reducing swelling and inflammation of the tissues of the palatine tonsils.
The laser radiation source can be installed in the oral cavity and acted in close proximity to the palatine tonsils and the mucous membrane of the posterior pharyngeal wall, thereby achieving the best results.
You can also install the laser emitter on the skin of the anterolateral surface of the neck in the projection of the location of the palatine tonsils and the posterior wall of the pharynx.
Fifth stage.
It is recommended to conduct sessions of vibroacoustic influence. They are carried out with the aim of normalizing microcirculation in the tissues of the palatine tonsils and improving the trophism (nutritional function) of the palatine tonsils themselves.
Sixth stage.
Effectively sanitize the microflora located on the surface of the palatine tonsils using ultraviolet irradiation (UVR).
This method has long been known, has proven itself very well and is still in service in many city (especially children's) clinics.
In this case, it is necessary to approach courses. The number of procedures in each specific case is determined individually at the first consultation with an ENT specialist. But for a lasting effect to occur, at least five sessions must be performed. If, during the fifth procedure, caseous and mucous masses are still washed out of the lacunae of the palatine tonsils, rinsing and other procedures must be continued “until clean rinsing waters”. As a rule, the number of ENT procedures does not exceed 10 treatment sessions.
After a full course, the lacunae of the palatine tonsils restore their ability to cleanse themselves, and the patient feels much better and more energetic.
In order to have a lasting result, it is necessary to carry out conservative treatment 2 to 4 times a year, as well as independently once every 3 months, take homeopathic and antiseptic medications.
In this case, you will most likely be able to avoid exacerbations of this disease and the need to remove the tonsils.
If, 2-4 weeks after the end of the course, caseous detritus again begins to accumulate in the thickness of the palatine tonsils, and the patient’s ENT complaints begin to bother them, as before the start of the course, conservative treatment of chronic tonsillitis in children and adults is considered ineffective. In this case, the patient is asked to consider the option of surgical removal of the tonsils. But fortunately, such an outcome (result) is quite rare.
Chronic tonsillar pathology occupies a special place among chronic lesions of the ENT organs. This is due to both the relatively rapid chronicization of the process in the palatine tonsils and the possibility of the development of generalized, even fatal, complications, as well as the peculiarities of the course and influence on the body of associated (metatonsillar) diseases. According to various authors, from 4 to 35% of the population suffer from chronic tonsillitis, while in different regions of the Russian Federation there is an increase in the number of patients suffering from this pathology.
Chronic tonsillitis, being a classic example of a focal infection, is essentially a chronic infectious-allergic disease with a local inflammatory reaction in the palatine tonsils, which makes it possible to develop a whole set of complications based on the activity of β-hemolytic streptococcus, its antigens and various pathogenicity factors , in which streptolysins play a key role.
It is known that most acute inflammatory diseases characterized by damage to the ENT organs, in the absence of adequate therapy, tend to become chronic. However, the pathology associated with the palatine tonsils has pronounced distinctive features both in the formation of chronic inflammation and in the strict phasing of the development of this pathological process. In the natural physiological functions of the palatine tonsils, normal and pathological processes interact so closely that, despite the large number of diverse studies that have been carried out on this problem, until now it has been practically impossible to establish an absolutely definite “point of no return” when irreversible pathomorphological changes occur in the structure of the palatine tonsils, and radical treatment methods, in particular tonsillectomy, are already required. The lack of a consensus solution on this issue in the modern medical community only further aggravates the problem.
Thus, very often in routine clinical practice, when choosing further tactics for patient management, doctors are guided primarily by anamnestic data on the number of sore throats and peritonsillar abscesses suffered, focusing more on subjective sensations than on objective clinical symptoms and data from laboratory research methods. Meanwhile, the currently existing classification of chronic tonsillitis B.S. Preobrazhensky—V.T. Palchun (and the diagnostic criteria embedded in it), developed at one time at the Department of Otorhinolaryngology of the Russian National Research Medical University named after. N.I. Pirogov, allows you to clearly differentiate various forms of chronic tonsillar pathology and gives a clear indication of further tactics for managing this patient [1, 2]. Unlike existing classifications of chronic tonsillitis, this classification reflects the stages of development of the pathological process in the structure of the palatine tonsils and the influence of these processes on the body as a whole in accordance with the main pathogenetic links of this disease. At the same time, the comments to this classification directly state the need to perform tonsillectomy in patients with chronic tonsillitis of the toxic-allergic form (TAF) II, as well as, in case of ineffectiveness of conservative therapy, in patients with chronic tonsillitis TAF I. However, despite this, it is regrettable to state that in the medical environment and especially in the therapeutic community, there is still an opinion about the need to preserve the palatine tonsils as an immunocompetent organ by any means, even despite the possible severity of general somatic symptoms and the obvious failure of the palatine tonsils in conditions of profound changes in its structure against the background of pronounced chronic changes .
That is why, when choosing a treatment method for a patient with chronic tonsillar pathology, it is necessary, first of all, to be guided by the knowledge that has been accumulated on this problem at present, and to objectively assess the risk of complications that can lead to the development of, including lethal symptoms, and the classification of chronic tonsillitis B.S. Preobrazhensky - V.T. Palchuna should be the main guideline for detailing the diagnosis and, on this basis, choosing tactics for further management.
The stages of development of pathomorphological changes in the structure of the palatine tonsils, as well as the formation of general and local associated diseases (metatonsillar complications), reflected in the classification of B.S. Preobrazhensky—V.T. Palchun, are largely determined by the biological properties of the main etiologically significant microorganisms [3].
According to the results of many studies conducted in recent decades, among the microorganisms that claim to be the leading etiological factor in the development of chronic tonsillitis, one can find a large number of pathogens with different properties, including streptococci, staphylococci, Haemophilus influenzae, lymphotropic viruses, etc. In accordance with According to the results of these studies, chronic tonsillitis is considered to be a polyetiological disease. Considering this issue from the perspective of clinical microbiology, it should be noted that in most cases, causally significant microorganisms are primarily bacteria growing in the distal parts of the crypts of the palatine tonsils. Since these sections of the tonsils have an extremely low oxygen content, the dominant flora growing on the surface of the mucous membrane of the tonsil crypts are microorganisms with an anaerobic type of metabolism, which are represented by peptococci and bacteroides. prevotella, fusobacteria, etc. However, the leading role in the development of chronic changes in the palatine tonsils, as well as local and general complications of chronic tonsillitis is given to β-hemolytic streptococcus of the serological group, A ( S
.
pyogenes
) - a microorganism that also uses anaerobic respiration for its life. At the same time, the palatine tonsils are the only natural reservoir of pyogenic streptococcus in the macroorganism [4, 5].
And it is this fact that in most cases determines the development of toxic-allergic manifestations in the human body, leading to the formation of common diseases associated with chronic tonsillitis. Among these diseases, acute rheumatic fever and post-streptococcal glomerulonephritis should be particularly highlighted, which, as a rule, lead to pathology of the cardiovascular and urinary systems, and also worsen the quality of life and, ultimately, shorten it [6-8].
S
.
pyogenes
are microorganisms that are gram-positive cocci, having a classic type of arrangement for streptococci - in the form of a chain, giving complete lysis of red blood cells (beta-hemolysis) on blood agar and belonging to the serological group, A in the antigenic classification of streptococci by R. Lensfield. Streptococcus pyogenes has significant resistance to physical and chemical environmental factors. The only natural reservoir of pyogenic streptococcus in the macroorganism is the distal sections of the lacunae of the palatine tonsils.
The pathogenesis of pyogenic streptococcal infections is associated with the activation of these microorganisms in the deep sections of the lacunae of the palatine tonsils, their subsequent invasion into the structures of the lymphoid tissue of the tonsils due to the presence of a large number of extracellular enzymes - streptokinase, which catalyzes the conversion of plasminogen into the proteolytic enzyme plasmin, hyaluronidase, which destroys hyaluronic acid, which is the main a component of connective tissue, streptodornase (DNAase), which destroys elements of the genome of connective tissue cells, etc. The production of membrane-damaging toxins O- and S-streptolysins specific to this pathogen leads to the development of systemic intoxication, cardiotoxicity, which is explained by the suppression of energy processes in the mitochondria of myocardial cells under conditions of O-streptolysin activity, which also has hemolytic activity and immunogenic properties. The action of S-streptolysin together with the antichemotactic factor (peptidase C5a) is associated with the suppression of the activity of phagocytic cells and the destruction of mitochondrial membranes of cells in the lesion. The specificity of clinical symptoms of damage to the palatine tonsils is primarily due to the action of these pathogenicity factors.
In addition, a feature of the cell wall of pyogenic streptococcus can be considered the presence of a large number of surface protein structures, in particular M-protein, which is an important adhesin of these microorganisms. M-protein ensures binding to collagen, fibronectin, as well as serum proteins - fibrinogen, components of the complement system, as well as other elements of various organs and systems, causing activation of the primary phase of development of metatonsillar complications. The ability of pyogenic streptococcus to penetrate into epithelial cells with the development of the phenomenon of internalization is associated with the presence of M-protein. Streptococcus pyogenes has a hyaluronic capsule that protects it from immunological surveillance authorities and is a factor in antiphagocytic activity.
In addition, S
.
pyogenes
has and synthesizes a large number of substances that have the properties of superantigens, cause mitogenic activity and lead to polyclonal proliferation of T lymphocytes. Superantigens of streptococci include pyrogenic exotoxins (SPE A, SPE B, SPE C, SPE D), the mitogenic factor SPE F and, probably, type-specific M proteins [2, 9]. Pyrogenic toxin, A (Spe A), whose gene is localized on a temperate bacteriophage, is associated with the most severe forms of streptococcal infection. The gene encoding this toxin is detected in ½ of cases of scarlet fever and rheumatic fever. The pyrogenic toxin B gene is localized in the chromosomal DNA of the cell and is a cysteine proteinase that is capable of breaking down fibronectin in the macroorganism. In patients with invasive forms of streptococcal infection (cellulitis, pneumonia, necrotizing fasciitis), there is an increased level of antibodies to pyrogenic exotoxin B (SPE B). In addition, the production of SPE B by streptococci was combined with a high risk of developing acute post-streptococcal glomerulonephritis [10, 11].
It has now been proven that streptococci can not only attach to the cells of the macroorganism, but also penetrate them. Thus, A. Osterlund [12], examining the tonsils of children with recurrent tonsillitis, identified streptococci located inside the cells, and 30% of failures in the treatment of chronic tonsillitis are associated with the presence of the pathogen intracellularly.
It should also be noted that β-hemolytic streptococcus persists in the structure of the mucous membrane of the crypts of the palatine tonsils not in the form of planktonic cultures, but in the form of pathological biofilms, which determine not only protection from exogenous environmental factors, but also resistance to various methods of therapeutic intervention [13, 14].
In the development of the stages of the clinical picture of tonsillitis (which are reflected in the classification of B.S. Preobrazhensky - V.T. Palchun), several factors associated with pyogenic streptococcus take part: 1) a toxic factor that determines the pathological effect of streptolysins on the cardiovascular, nervous and endocrine system, which is manifested by general intoxication, fever, etc.; 2) a septic factor, which is associated with the influence of enzymes of the pathogenicity of beta-hemolytic streptococcus, resulting in a local inflammatory reaction in the structure of the palatine tonsils and further invasion of microorganisms deep into the tissues with the possibility of further generalization of the process, often hematogenously, up to the development of tonsillogenic sepsis, severe reaction of lymph nodes, etc.; 3) an allergic factor (a complex of surface substances of pyogenic streptococcus), which causes sensitization of the macroorganism to beta-hemolytic streptococcus and antigens of destroyed body tissues, which then leads to the development of glomerulonephritis, myocarditis, etc. [2].
Analyzing all of the above, we have to state that the pathogenicity factors of streptococcus pyogenes and its biological properties directly affect the nature of the clinical course of tonsillar pathology and its complications, which proves the leading role of this microorganism in the genesis of chronic tonsillitis.
Features of the anatomical and histological structure of the palatine tonsils, along with the biological properties of pyogenic streptococcus, also make a significant contribution to the development of chronic inflammation in them. Being part of the lymphoepithelial pharyngeal ring, the palatine tonsils are not only the largest in size, but also the most complex structure among all the elements of this ring, which largely determines the development of a focus of chronic infection.
Thus, it is known that the palatine tonsil consists of lobules that have a complex structure. From different parts of the connective tissue capsule of the tonsil, bundles of connective tissue run towards the pharynx surface, forming the basis of the lobules (stroma). Then these main cords branch into smaller ones that penetrate the entire amygdala. The tonsil parenchyma is a group of lymphoid follicles located in a finely looped connective tissue network. In the center of such more or less rounded follicles there is a zone that, when preparing a microslide, has a lighter color - the so-called germinal center, where young lymphocytes are formed, which, as they develop, are gradually pushed towards the periphery of the follicle. An important feature of the palatine tonsils, which determines both normal physiological and pathological processes, is the presence of crypts. They begin on the pharynx surface and go deep into the tonsil, branching like a tree. The crypts, like the entire pharyngeal surface of the tonsil, are lined with stratified squamous epithelium in 6-8 rows.
In some places of the crypts the epithelial cover is interrupted (areas of physiological angization). Here contact between microorganisms and lymphocytes occurs. It is the areas of physiological angization that provide contact of microorganisms with the mantle zone of the follicles. Microorganisms growing on the surface of the crypts freely penetrate into the lymphadenoid tissue exposed in these breaks in the epithelium. In this way, a natural biological mechanism is formed that ensures the penetration of an infectious agent from the external environment into the lymphoid tissue of the tonsil, which leads to the initiation of the development of the germinal center of the follicles of the palatine tonsil, the differentiation of B-lymphocytes into highly specific plasma cells capable of synthesizing high-avidity antibodies. Immune control ensures the death of microorganisms that have penetrated into the parenchyma of the NM. In this case, the source of infection is inactivated by the general immune factors of the macroorganism. The bacteria die, but retain particles of their antigenic structure, which is an additional stimulus for the activation of local and general immunological reactions.
Recognition of antigenic structures of microorganisms also occurs due to Toll-like receptors. At the same time, a number of authors note that not only lymphocytes express Toll-like receptors (TLRs) on their surface, which play a key role in the recognition of microorganisms. These receptors are found in epithelial cells of the tonsils, primarily in the cryptal and luminal cells [15]. The detection of these receptors in the epithelium of the tonsils may indicate its functional role as antigen-presenting cells, and this also serves as confirmation that in conditions of a normally functioning tonsil, the lining of the crypts is not damaged.
Thus, the very structure of the amygdala, namely tree-like branching crypts with 4-6 orders, contributes to the formation of acquired immunity, increasing the time of contact of the pathogen with immune cells. However, in situations where the outflow of contents is delayed beyond a certain time, the lacunae acquire the ability to cystic expansion. Under these conditions, the crypt epithelium begins to be affected for a long time by toxins of microorganisms, which subsequently take a direct part in the formation of various toxic-allergic manifestations. That is why the delay in the outflow of the contents of the lacunae is one of the important mechanisms for the development of chronicity of the process, and also takes part in the genesis of associated pathology, the further systemic impact of the formed chronic focus of infection on the macroorganism and the formation of gross pathomorphological changes in the tissues of the tonsils themselves.
The starting point in the development of chronic tonsillitis is a violation of the local immune status of the mucous membrane of the palatine tonsils, which, together with the effects of bacterial toxins and sometimes lymphotropic viruses on the crypt epithelium, can lead to its thinning and the formation of areas of no longer physiological, but pathological angization. This allows etiologically significant microorganisms to penetrate into the deep cellular layers of the mucous membrane, deep into the tonsil parenchyma, into the blood vessels and initiate further pathological processes.
It should be noted that in modern literature there is little data on the changes that occur in the palatine tonsils at different forms and stages of chronic tonsillitis at the cellular level. The research conducted at our department helped to complement the understanding of the physiology and pathophysiology of the palatine tonsils in conditions of the formation of chronic inflammation in them. During the study, the autoradiography method was used to evaluate the histoarchitecture of the palatine tonsils, as well as to determine the functional activity of microorganisms located in the tonsillar parenchyma, both normally and in patients with chronic tonsillitis. The essence of the method was the use of radioactive precursors of nucleic acids (3H-thymidine, 3H-uridine). The accumulation of 3H-thymidine by the cell demonstrates the ability of these cells to synthesize DNA, i.e., indicates their proliferative activity. The synthesis of RNA, which is the template for protein synthesis, reflects the functional activity of the cell. In addition, the cell's ability to absorb and accumulate radioactive tracers makes it possible to differentiate viable bacteria and normally functioning tonsil cells from nonviable cellular debris.
According to the results of these studies, in the tissues of unchanged palatine tonsils, microorganisms were found exclusively on the surface of the mucous membrane of the crypts, while the epithelial cells of the palatine tonsils had a normal structure, were characterized by a normal nuclear structure, and the absence of pathological proliferative activity. In addition, in healthy palatine tonsils, only individual endothelial cells showed insignificant functional activity, i.e., they synthesized RNA.
During the formation of a chronic focus of infection and the development of toxic-allergic forms, on the contrary, a violation of the cytoarchitectonics of the tonsil tissue was observed: the growth of connective tissue into the lymphoid tissue, the appearance of individual foci of necrosis, signs of destruction of the walls of microcirculatory vessels, and necrotic changes in the epithelial lining of the crypts appeared. A characteristic feature of patients with toxic-allergic forms of chronic tonsillitis was the detection of microorganisms in the tonsil tissue. At the same time, microorganisms absorbed both 3H-uridine and 3H-thymidine, which indicated not only their functional (protein synthesis), but also proliferative activity. Moreover, some functionally active microorganisms were compactly located in the structure of the pathologically altered vascular endothelium. It is necessary to understand that the formation of connective tissue, microabscesses, granulations inside the parenchyma of the tonsils contributes to the isolation of microorganisms, as well as their resistance to conservative treatment methods. Pathomorphological changes that occur in the palatine tonsils lead to the loss of the immune function of the latter.
In addition, a detailed study of tonsil follicles using various immunohistochemical markers provides insight into the processes occurring in the tonsils at the cellular level. A study on the Ki-67 cell proliferation marker in patients with hypertrophic tonsillitis and a negative test for β-hemolytic streptococcus group A in comparison with patients with chronic tonsillitis and laboratory-confirmed streptococcal presence indicates a predominance of cell division in patients without an infectious process in the tonsils, in difference from patients with chronic tonsillar pathology associated with pyogenic streptococcus. At the same time, markers of apoptotic and anti-apoptotic activity demonstrate a picture of degenerative changes in the structure of the palatine tonsils in patients with chronic tonsillar pathology. Thus, changes in caspase-3, Fac/CD95, Fax suggest the predominance of cell death processes in the tonsils with chronic inflammation caused by a bacterial nature.
The expression of markers of anti-apoptotic activity, such as Bcl-2 and surferin, also demonstrates their predominance in the palatine tonsils of patients with chronic tonsillar pathology [16].
The penetration of pathogens into the tonsil parenchyma, in addition to the events described above, is characterized by a slight increase in the volume of lymphoid follicles, disorganization of reticular fibers, and subsequently their death with replacement by connective tissue and the development of a scar process [2, 17]. All this gradually leads to a decrease in the total area of active lymphoid tissue in the tonsil and contributes to the “burying” of microorganisms between scar tissue, and also creates conditions for the development of reactive complications of chronic tonsillitis.
Thus, chronic inflammation developing in the structure of the tonsils radically changes the cytoarchitectonics of the palatine tonsils, transforming them from functionally active immune structures into a dangerous focus of the infectious process in the body, leading to its sensitization and the development of toxic-allergic manifestations.
The issue of treatment of patients with chronic tonsillar pathology remains, perhaps, one of the most controversial in otorhinolaryngology. And if making a diagnosis of “chronic tonsillitis”, as a rule, does not cause difficulties, then deciding on the stage, phase, form of the disease and, as a consequence, the choice of treatment method, raises a large number of questions and is often based on the subjective feelings of the doctor.
Along with the classical bacteriological method for diagnosing chronic tonsillitis and identifying the pathogen, in recent years a large number of new methods have been developed not only for diagnosing chronic tonsillitis, but also for assessing the functional state of the tonsils.
A method for assessing the functional state of the palatine tonsils by cytological examination of the contents of their crypts in chronic tonsillitis is proposed.
E.V. Tyrnova and G.S. Maltsev propose a biochemical method for diagnosing chronic tonsillar pathology, based on the determination of C-reactive protein, rheumatoid factor and antistreptolysin-O in blood serum [18].
V.M. Tsirkunov et al. [19] propose a method for diagnosing the degree of activity and stage of chronicity of chronic tonsillitis, based on a biopsy of the palatine tonsils.
L.A. Dyukov et al. [20] propose a method for quantitative scoring of the state of intestinal microbiocenosis in patients with chronic tonsillitis with the determination of the dysbiosis index as a method of additional diagnosis of various forms of chronic tonsillitis.
However, none of these methods are widely used in clinical practice for various reasons. But it is the timely and correct determination of the form of the disease that guarantees success in treatment and protects the patient from complications.
In the current conditions, based on the polyetiology of chronic tonsillitis, the lack of a generally accepted instrumental or functional diagnostic method, the danger of developing local and general complications, the classification of chronic tonsillitis proposed by B.S. Preobrazhensky and V.T. Palchun, not only has not lost its relevance, but, on the contrary, is acquiring primary importance in the choice of treatment methods for this disease and makes it possible to establish strict indications for surgical treatment.
The undoubted advantage of the classification of chronic tonsillitis under consideration is its clear focus on the etiology, pathogenesis of the disease, the risk of developing concomitant and associated diseases, as well as a reflection of the stages of development of the process in the macroorganism both at the systemic and cellular levels.
Thus, with a simple form of chronic tonsillitis and the absence of signs of systemic changes in the macroorganism, courses of conservative therapy are possible.
In case of chronic tonsillitis TAF I degree, when microorganisms penetrate into the tonsil parenchyma and progressive inflammatory changes develop, leading to sclerosis of the parenchyma, the walls of blood vessels are damaged and their lumen increases, the patient is shown a test course of conservative treatment, including local (washing the lacunae of the palatine tonsils) and systemic antibacterial therapy. If success is achieved with this treatment, it may be continued. However, dynamic monitoring of the patient is necessary so as not to miss the moment of transition of the disease to the next form. If there is no effect from the test course of therapy, surgical treatment is indicated.
A characteristic feature of stage II TAF is the formation of microfoci of necrosis in the structure of the tonsillar, which leads to complete functional failure of the tonsil, expressed in atrophy and death of the follicles. In the tonsils, decay processes prevail, microbial cells are found in the lumen of blood vessels along with cellular and microbial detritus, and metatonsillar complications develop. With this form of chronic tonsillitis, there is no need to talk about the possibility of conservative treatment of a source of chronic infection in the body, and the only method to cure the patient and prevent the development of complications is to remove the tonsils.
A timely tonsillectomy not only cures the patient and protects him from serious complications, but is also cost-effective. In a study conducted in 2002 by N. Bhattachatyya and L. Kepnes [21], patients were observed after tonsillectomy (average follow-up duration 37.7 months). In addition to the subjective improvement in quality of life, during the 12 months after surgery, there was a decrease in antibiotic consumption by an average of 5.9 weeks per year. The number of days of disability associated with chronic tonsillitis decreased by an average of 8.7 days per year. The number of disease-related visits to the doctor decreased by an average of 5.3 visits per year. And taking into account all the economic costs of the operation, the break-even point occurs 2 years after the operation.
Even taking into account the obvious differences in the tactics of treating chronic tonsillitis, which are a consequence of fundamental differences in the issues of financing and organization of medical care, the place of scientific research in clinical practice, the capabilities of health insurance systems in Russia and abroad, the understanding of the inevitability of eliminating the source of infection for the patient’s health remains the same . In this case, the main guideline for deciding the choice of therapeutic treatment tactics or the need to perform tonsillectomy should be the form of chronic tonsillitis in accordance with the classification of B.S. Preobrazhensky–V.T. Palchuna. In this regard, and also taking into account the stated modern ideas about the etiology, pathogenesis and clinical picture of chronic tonsillitis, it is worth thinking about the need for widespread use of this classification in the practice of otorhinolaryngologists in Russia. We invite specialists to take part in a discussion on this issue on the pages of the magazine.
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Information about authors
Palchun V.T. — e-mail; https://orcid.org/0000-0002-3521-7424
Kryukov A.I. — e-mail; https://orcid.org/0000-0002-0149-0676
Gurov A.V. — e-mail; https://orcid.org/0000-0001-9811-8397
Ermolaev A.G. - e-mail; https://orcid.org/0000-0003-2642-5173
Corresponding author:
Gurov A.V. — e-mail: [email protected]
Palchun V.T., Kryukov A.I., Gurov A.V., Ermolaev A.G. Palatine tonsils: physiology and pathology. Bulletin of Otorhinolaryngology
. 2019;84(6):11-16. https://doi.org/10.17116/otorino20198406111
Drug treatment of chronic tonsillitis
Dear patients! In this article I will describe only general principles and approaches.
More precise treatment will be offered to you at the initial ENT consultation, where an accurate diagnosis, form and degree of the disease will be made, as well as an optimal recovery plan will be proposed and a prognosis for the duration of remission will be given.
So:
- Antibacterial approach. Antibiotic therapy is important and necessary. But the decision to prescribe antibacterial drugs is made individually and only after a visual examination.
Antibiotics can be either light, prescribed for a short course and have no effect on the mucous membrane of the gastrointestinal tract, or heavy, which must be prescribed under the guise of probiotic medications. The choice of antibiotic depends on the severity of chronic tonsillitis and the microflora that supports this condition. - Probiotic treatment is prescribed in case of taking aggressive antibiotics, as well as in the presence of concomitant gastritis, duodenitis, reflux esophagitis.
- Antiseptic approach. Antiseptic sprays, aerosols, and rinses also give a very good effect and are therefore mandatory in the fight against chronic tonsillitis. I prefer a 0.01% solution of Miramistin, a 1% solution of Dioxidine (1 ampoule diluted - 10 ml + 100 ml of boiled warm water) and Octenisept, which must be diluted with boiled warm water or saline in a dilution of 1:5 , or 1:6.
- Decongestant (desensitizing) therapy is mandatory. It is needed to relieve swelling of the palatine tonsils and the surrounding tissue, as well as the mucous membrane of the posterior pharyngeal wall. This is also necessary for better absorption of all medications used. Such modern medications as Cetrin, Claritin, Telfast can cope with these tasks. But if a certain desensitizing drug helps you for a long time, you should not change it to another.
- Immunostimulating therapy. Here I want to draw your attention to the fact that the doctor prescribes drugs that stimulate the immune system. These drugs should not be confused with immunomodulators, which are strictly prescribed by an immunologist based on the results of a blood test. There are not so many drugs that stimulate local immunity at the level of the palatine tonsils and the mucous membrane of the posterior pharyngeal wall. Of the well-known drugs, Imudon comes first. The course must be at least 10 days. You need to take (dissolve) Imudon 1 tablet 4 times a day.
- Homeopathic treatment. In addition to conventional drug therapy of a chemical nature, it is necessary to take homeopathic medications that improve the trophism and, as a result, the nutritional function of the palatine tonsils. The drugs of choice may be tonsillotren and tonsilgon, as well as rinses, steam and ultrasonic inhalations with infusions and herbs: propolis, string, sage, chamomile and some other herbs.
- Emollient therapy is used symptomatically, when, against the background of exacerbation of tonsillitis, as well as taking medications, there may be dryness, rawness and soreness in the throat. In such cases, you can use peach oil, which must be instilled a few drops into the nose, throwing back the head. You can rinse your mouth with 3% hydrogen peroxide (VERY IMPORTANT! 6% and 9% hydrogen peroxide CANNOT be used!!!). To do this, you need to pour half a bottle of peroxide (10 ml) into a cup, put it in your mouth and rinse the entire solution once, for as long as possible. Then the solution is spat out and rinsed from foam and bitterness with warm boiled water. After gargling with hydrogen peroxide, you will feel a significant softening and comfort in your throat. You can gargle twice a day, but no more.
- Analgesic therapy is used if necessary, as symptomatic therapy, depending on the severity of the pain syndrome. Of the tablet forms, it is better to give preference to Nurofen or Ketanal and its derivatives: Ketarol, Ketalar, Ketanof, Ketanal.
- Diet therapy. Nutrition also plays a significant role in recovery. It is necessary to limit the intake of spicy, fried, sour, salty and peppery foods. During treatment, you should exclude hard foods from your diet. It is also recommended to protect yourself from very hot and very cold foods. Drinking alcohol, especially strong alcohol, is also contraindicated.
Features of the condition with enlarged tonsils without fever
Even at normal body temperature, but in the presence of pathological processes in the body, a person may feel completely unwell. Inflammation of the tonsils without fever, regardless of the cause, can interfere with a normal lifestyle and be accompanied by:
- headache;
- sore throat;
- lack of appetite;
- difficulty swallowing;
- dryness and sore throat;
- enlarged lymph nodes and pain on palpation;
- fatigue, weakness, drowsiness, decreased performance, irritability.
Surgical removal of tonsils
If we talk about the removal of the tonsils, then the operation to completely remove the tonsil tissue is called a bilateral tonsillectomy.
Partial removal of the tonsils is called a bilateral tonsillotomy.
It is extremely rare that the palatine tonsil is removed routinely on one side. There is also a practice of a number of hospitals (they like to do this in the Pirogov City Clinical Hospital No. 1) of removing the palatine tonsil or tonsils in case of a paratosillar abscess. This operation is called abscessonsillectomy. But it must be remembered that against the background of severe pain caused by an abscess, removal of the tonsil is extremely painful. Due to the purulent process, it is impossible to provide adequate anesthesia. Therefore, it is necessary to anesthetize the peri-almond tissue only with strong anesthetics: Ultracaine and Ultracaine DS-forte.
Routinely, palatine tonsils can be removed under local anesthesia or general anesthesia. Previously, this operation was performed only under local anesthesia.
Fortunately, there is now modern equipment that allows removal of palatine tonsils under general anesthesia or under anesthesia using cold plasma coagulation - Coblator.
Surgical methods for removing tonsils
Previously, tonsils were removed in the simplest surgical way - using a scalpel and wire thread. Today this method is practically not used.
There are many modern methods for removing tonsils, and here are just the most popular:
1.
IR laser
. Instead of a scalpel, a laser beam is used, which immediately solders the sutures along the edges and ensures quick rehabilitation with minimal blood loss.
2. Electrocoagulation
. It works in the same way as a laser, but it heats up neighboring tissues and can lead to undesirable consequences in the form of burns. However, cases are rare, and in general the method is quite safe.
3. Ultrasound
. High-frequency ultrasound cuts off inflamed tissue and instantly heals sutures. Fast recovery and minimal blood loss also indicate the safety of this method.
4. Cryodestruction
. Freezing tonsils with liquid nitrogen. The tissue is not cut off, but frozen and gradually falls off. The procedure is painless, but recovery takes a long time and can be unpleasant.
Prevention of chronic tonsillitis
- Drug therapy
. If an ENT patient undergoes treatment courses in the clinic once every 6 months, then in addition to six-month procedures, he is recommended to take the drug Tonsilotren, with a frequency of once every 3 months, i.e. 4 times a year. The course of taking (resorption) of the drug is for 2 weeks (more precisely 15 days). It is also possible to instill 0.01% Miramistin solution, 4 pumps 4 times a day for 2 weeks, in courses 4 times a year. - Climatotherapy and spa therapy
. An important point in the prevention of chronic tonsillitis is visiting seaside resorts. Sunbathing, humidified sea air, swimming and, as a result, the inevitable entry of sea water into the mouth have a beneficial effect on the prevention of chronic tonsillitis. - Work and rest schedule
. In order for the periods of remission to be long, it is necessary to fully rest and not expose yourself to stress. It is not without reason that chronic tonsillitis, like sinusitis, is classified as a social disease, in which the more stress and workload there is at work, the higher the likelihood of exacerbation of chronic tonsillitis. - Diet
. It is very important to eat right. Under no circumstances should you get carried away with fried, salty, peppery, sour, bitter, i.e. that food that irritates the mucous membrane of the back of the throat and palatine tonsils. Citrus fruits are contraindicated. The consumption of alcoholic beverages, especially strong ones, is also contraindicated. It is not advisable to eat very hot and very cold and solid foods.
Prognosis of tonsil cancer
At stages 1-2 without damage to the lymph collectors, the prognosis for life is favorable if the operation was successfully performed.
Radiation therapy does not guarantee a lifelong result even in the case of complete regression - the probability of relapse is high, however, they also try to operate on it and then the prognosis does not worsen.
The prognosis is changed in a negative direction by an initially common process that is not subject to radical therapy.
Surgeries for head and neck tumors, especially after competitive chemoradiation treatment, are technically complex and are fraught with a complicated course of the postoperative period. What adds problems is not the sterile environment inside the oral cavity, but the malnutrition induced by the tumor process. But the clinic’s specialists know how to find a way out even in the most hopeless clinical situation.
Book a consultation 24 hours a day
+7+7+78
Treatment or removal of tonsils?
Dear patients! If you have visited several specialists in this field, if a course of treatment for chronic tonsillitis has been carried out and none of the methods has brought the expected result, then only in this case should you think about removing the tonsils.
If a conservative approach gives lasting results for 4-6 months or more, then the palatine tonsils are able to fight on their own. Your task is to help the tonsils by regularly sanitizing them and stimulating their work physiotherapeutically.
Treatment of tonsil cancer
For any prevalence, excluding metastatic stage 4, surgical treatment is recommended at the first stage - removal of the tumor and lymph nodes affected by metastases.
If surgery is not possible, radiation is carried out in combination with chemotherapy or chemotherapy is performed sequentially, and then radiation therapy, and again the issue of surgical treatment is resolved. But if the cancer is completely regressed as a result of conservative measures, you can stop there; if there is any remaining cancer in the irradiation zone, removal is suggested.
The metastatic process is subject to systemic treatment - cytostatics in combination with immuno-oncological drugs. The spectrum of cytostatics is quite wide; 4 monoclonal antibodies have demonstrated effectiveness.
What to do if your child is sick
If a child is diagnosed with inflamed tonsils, the doctor will recommend what to take in this case. It is important to control the process and prevent it from becoming chronic. Separately, the doctor will dwell on recommendations for prevention. If you follow all the advice, inflamed tonsils in a child can be cured quickly and without relapse.
What to take
Drug treatment for children is most preferable to surgical removal of tonsils. Inflamed tonsils in a child are treated with antibacterial drugs, but if they do not bring results, the doctor changes them to antifungal drugs.
When you call a doctor, he will advise you on what to take if your child has inflammation of the tonsils and will prescribe a list of medications and safe antibacterial agents. Strepsils or Faringosept lozenges will help relieve sore throat. In children from the age of three, sprays can be used to irrigate the throat.
Are antibiotics needed?
Treatment with antibiotics is necessary for purulent inflammation of the tonsils. The doctor will prescribe the patient a course of broad-spectrum medications. The following groups are generally recommended:
- penicillins – Amoxicillin, Flemoxin solutab, Amoxiclav;
- macrolides – Azithromycin, Vilprafen;
- cephalosporins – Ceftriaxone, Cephalothin.
Prescriptions can be adjusted, but usually the course is at least ten days. If therapy is ineffective, the treatment regimen is changed.