Opportunistic infections, including mycoses, represent a pressing problem in modern medicine. Paradoxically, it was precisely the achievements of science that ensured the success of clinical medicine that led to an increase in the number of patients with opportunistic mycoses. In particular, advances in the treatment of a number of oncological and autoimmune diseases (the use of chemotherapy, anti-cytokine therapy, glucocorticosteroids and immunosuppressants) are associated with the emergence of a population of patients with acute and chronic iatrogenic immunodeficiency states. In turn, immunodeficiencies and local disorders of antimicrobial resistance in humans are the basis for the development of opportunistic mycoses, primarily candidiasis. Diagnosis and treatment of candidiasis of the mucous membranes of the digestive tract in some cases are associated with significant difficulties.
Fungi (Latin fungus, Greek mykes) are an independent vast kingdom of eukaryotic microorganisms, including about 90 thousand studied species. Until the end of the 1960s. Fungi were mistakenly classified as members of the plant kingdom. Among fungi, macromycetes and micromycetes are distinguished. The former are visible with the naked eye, the latter - with the help of microscopes. Unicellular (lower fungi, for example, Mucor) and multicellular (higher fungi, for example, Penicillium) forms of micromycetes are known [1].
Yeast-like fungi of the genus Candida are single-celled microorganisms 6–10 microns in size. These micromycetes are dimorphic: under different conditions they form both blastomycetes (bud cells) and pseudomycelia (threads of elongated cells). This morphological feature has, as will be shown below, important clinical significance.
Micromycetes of the genus Candida are characterized by ubiquity - widespread occurrence in the environment. Viable cells of Candida spp. can be found in soil, drinking water, food products, on the skin and mucous membranes of humans and animals. Thus, contact with these micromycetes of a person’s “open systems,” i.e., his skin and mucous membranes, is an ordinary fact.
What is candidiasis?
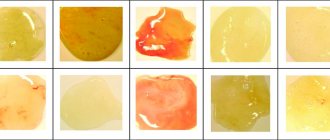
Candidiasis is a group of fungal diseases of local localization and systemic nature, manifested by purulent discharge and caused by yeast-like fungi of the genus Candida.
All representatives of this genus are classified as opportunistic fungi - this means that they normally exist in the human body, but their number is strictly limited. Under certain circumstances, the fungus begins to multiply rapidly, causing the development of the disease.
This fungal infection is popularly called “thrush”, which is associated with a characteristic symptom – white discharge. Most often, the impetus for the development of the disease comes from a decrease in immunity due to stress, failure to comply with basic hygiene rules, or the introduction of a more pathogenic strain of fungi of the genus Candida, which itself begins to actively develop and stimulates the development of normal microflora fungi.
Causes of candidiasis
Conventionally, the disease can be divided into childhood and adult. Infantile candidiasis can be transmitted during childbirth, by passing through infected mucous membranes of the mother, during feeding, and through everyday objects.
Due to the fact that children's immunity is poorly developed and largely depends on the mother, it is important to pay enough attention to one's own hygiene and the cleanliness of the space surrounding the child.
Adult candidiasis most often develops when the immune system is weakened, but the cause may be in factors that give impetus to the development of the disease.
Factors contributing to the development of candidiasis:
- External factors - temperature changes, humidity, skin damage, harmful environmental factors, chemical influences, leaching of one’s own microflora;
- Internal factors - metabolic disorders, non-inflammatory endocrine diseases, courses of treatment with hormonal drugs, taking hormonal contraceptives;
- Changes in the virulent properties of a fungal organism, tilting its qualities towards pathogenic ones.
Doctors note that candidiasis often occurs unnoticed by the patient, in a mild form. The body itself is able to cope with the fungus, and everything returns to normal quite quickly. However, if you notice symptoms of candidiasis, immediately contact GMS Clinic specialists to receive qualified treatment. We can provide the necessary and timely assistance to your immune system.
There are superficial and systemic candidiasis. Let's look at all types in more detail and analyze the systems of each type of candidiasis.
Risk factors for mucosal candidiasis
Defects in the antifungal resistance system briefly described above are factors contributing to the occurrence of candidiasis, or so-called. risk factors. Risk groups for the development of candidiasis of the digestive tract are presented below: • physiological immunodeficiencies (early childhood, old age, pregnancy); • genetically determined immunodeficiencies (for example, selective IgA deficiency); • iatrogenic immunodeficiencies – (for example, the consequences of treatment with glucocorticosteroids, immunosuppressants, anticytokine, radiation and polychemotherapy); • diseases of the endocrine system (for example, diabetes mellitus, autoimmune polyendocrine syndrome, hypothyroidism); • dysbiosis of mucous membranes after antibiotic therapy; • AIDS; • chronic “debilitating” diseases (for example, cirrhosis of the liver); • nutritional status disorders (for example, starvation and vitamin deficiencies).
In these groups, candidiasis is detected more often than usual. Note that sometimes the clear cause of the violation of antifungal resistance cannot be determined.
Superficial candidiasis, types, symptoms
This type of candidiasis includes damage to mucous membranes, smooth skin, nail beds and other surfaces.
Candidiasis of the oral mucosa
Most often, this type of disease occurs in newborns who have not yet developed the acidity of the oral cavity, which protects the mucous membranes from pathogenic microorganisms. The main symptom of the disease is a white cheesy discharge on the mucous membrane of the cheeks and tongue. It looks as if a child just drank kefir or ate cottage cheese. Most often, mucosal candidiasis does not pose a particular danger to the patient’s health if treatment is taken in a timely manner.
Candidiasis of the skin
It manifests itself as a secondary allergic reaction in the form of small swollen spots and ulcers. It can develop as a concomitant disease to inflammatory processes of various etiologies, falling on unprotected areas of the skin. In addition, it can develop when dirt gets into the wounds, so it is necessary to promptly protect and treat even the smallest scratches.
Intestinal candidiasis
It occurs with dysbacteriosis, since it is in this condition that the intestines are least protected. A decrease in the general acidity of the environment promotes the development of foreign microorganisms, and a decrease in the number of native microflora contributes to an increase in the variety of colonies.
Symptoms of intestinal candidiasis are loose stools mixed with white flakes, excessive gas formation, and abdominal pain. This condition is dangerous because, along with diarrhea, vitamins and nutrients are washed out of the body, food is practically not absorbed, and dehydration occurs. If you notice even the slightest symptoms, contact your doctor immediately.
Candidiasis of the genital organs in men and women (vaginal)
A characteristic symptom of the disease is copious white curdled discharge and itching. Pain during sexual intercourse and urination. This is typical for both the disease in men and female (vaginal) candidiasis. Most often, the disease is transmitted sexually, but can also occur as a result of an inflammatory process.
- Vaginal candidiasis is dangerous because disruption of the microflora of the uterus is dangerous due to inflammatory processes that can lead to infertility. That is why, when the first signs of candidiasis are detected, it is necessary to urgently contact specialists for treatment;
- Candidiasis of the male genital organs, in addition to pain and white plaque, can be characterized by redness of the foreskin and penis, as well as the formation of a white coating. If you notice symptoms, do not delay, immediately contact the specialists of the GMS Clinic Dermatology Center to prescribe qualified treatment.
Systemic candidiasis
Systemic candidiasis develops from local candidiasis with a sharp decrease in the level of immunity, as well as with persistent ignoring of the symptoms of visceral candidiasis. Symptoms of the disease can be different and similar to the symptoms of other diseases. Systemic candidiasis can be identified only after undergoing tests from a good specialist.
The consequences of systemic candidiasis can be different. Their severity depends on how much time passes from the moment of transition of visceral candidiasis to systemic and the delay in the start of treatment. GMS Clinic doctors will help reduce the consequences of candidiasis to a minimum and quickly get rid of the disease with virtually no harm to the body.
An integrated approach to the treatment of patients with candidiasis of the digestive tract
Candida fungi are opportunistic microorganisms that normally populate the digestive tract, participate in the process of fermentation, food digestion, etc. This phenomenon, called colonization, is clinically asymptomatic. A study of adult healthy volunteers showed that Candida albicans was present in their oropharyngeal zone in 20–30%, in the small intestine – in 50–54%, in the large intestine – in 55–70%, in feces – in 65–70% of cases .
So, with physiological well-being, there is a certain balance between macro- and microorganisms, in which, on the one hand, factors of the body’s resistance to microscopic fungi play a role, on the other, factors of the pathogenicity of fungi. The body's resistance depends on belonging to risk groups and the competence of its immune system. For protection, macrophage and neutrophil phagocytosis is also important, preventing the dissemination of fungal, especially candidiasis, infection.
According to most researchers, the asymptomatic presence of fungi in the gastrointestinal tract (GIT) can cease when they acquire pathogenic properties, and the patient’s immune system fails.
The most common mycoses of the digestive tract are esophageal candidiasis and intestinal candidiasis, which occur both in immunocompetent and (much more often) in immunosuppressed individuals. Primary mycoses of the stomach, including candidiasis, are rarely diagnosed, which is associated with the physiological acidic environment of the stomach, where fungal cells die.
Risk factors for the development of candidiasis of the esophagus and intestines are:
1. Gastrointestinal diseases:
- diseases of the mucous membranes of the oral cavity;
- gastroesophageal reflux disease;
- stomach contamination with Helicobacter pylori;
- atrophic gastritis, gastric hypoacidity, achalasia, bulbitis;
- erosive and ulcerative diseases of the esophagus and intestines;
- mixed intestinal infection, dysbiosis;
- diverticulosis, polyposis;
- enterocolitis, Crohn's disease, irritable bowel syndrome, etc.
2. Other diseases:
- oncological;
- hematological;
- endocrinological;
- allergic;
- AIDS and HIV infection.
3. Injury to the gastrointestinal mucosa:
- esophagogastric tube;
- burns of the esophagus;
- surgical interventions.
4. Taking medications:
- antibiotics;
- cytostatics;
- hormones and other chemotherapy drugs.
Malnutrition, fasting, alcoholism, smoking, drug addiction contribute to the development of candidiasis. Risk factors also include old age, when the immune system ages, numerous somatic diseases occur, the amplitude of longitudinal contractions of the esophagus and the strength of sphincter contractions decrease, absorption processes are disrupted, etc.
Clinically, candidiasis of the digestive tract is divided into:
- oropharyngeal candidiasis (pseudomembranous, atrophic, erythromatous, rhomboid glossitis, angular cheilitis);
- candidal esophagitis (erosive and without erosion);
- gastric candidiasis (erosive-fibrinous and secondary to peptic ulcer);
- intestinal candidiasis (pseudomembranous, collagenous, lymphocytic);
- candidal proctosigmoiditis;
- perianal candidiasis;
- secretory diarrhea associated with candidiasis.
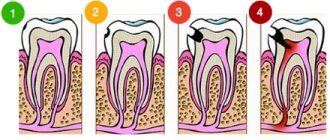
Candidal esophagitis in general hospitals occurs in 1.3–2.8% of patients, in transplant departments - up to 4%, with disseminated carcinomatosis - from 2.8 to 6.7%. This disease often occurs without subjective complaints and is detected incidentally in population studies in 1–7% of cases. Sometimes patients note pain and discomfort when passing solid and liquid food, dysphagia, and hypersalivation. According to the depth of the lesion, 4 types are endoscopically distinguished: from mild edema, hyperemia, single white plaques <1 mm in diameter to massive inflammation, deformation and bleeding of the mucosa, ulceration, even perforation.
Gastric candidiasis, as a rule, develops secondary to peptic ulcer and gastroesophageal reflux disease. Achlorhydria, in turn, promotes the colonization of fungi on the mucous membrane with subsequent invasion, especially in defect areas (ulcers, erosion), which slows down repair (healing), pain syndrome appears, and sometimes bleeding of the ulcer.
Candidiasis of the intestine usually manifests itself as abdominal discomfort, diarrhea, bloating, pain and other symptoms. The study of intestinal microbiocenosis makes it possible to specify amorphous “enterocolitis”, namely: to differentiate pseudomembranous colitis caused by Clostridium difficile, an acute process in the intestine caused by rotoviruses and Escherichia coli, Crohn’s disease, irritable bowel syndrome from candidiasis or dysbiosis with a predominant candidal component.
In most cases, fungal infections of the gastrointestinal tract are accompanied by changes in microbiocenosis and a decrease in the body's colonization resistance. To treat gastrointestinal candidiasis, a wide variety of antimycotics, both systemic and local, are used. Also, one of the goals of therapy is to create conditions for the growth and functioning of normal microflora.
In modern scientific literature, drugs for the correction of dysbiosis are divided into 3 main groups: probiotics - contain viable microorganisms; prebiotics – contain microflora growth stimulants; synbiotics – contain live microorganisms and prebiotics. There are probiotic complexes, which are a combination of the above components, as well as sorbents, vitamins and microelements. There are a lot of means for correcting intestinal microflora disorders, and new options and varieties are constantly appearing.
A further development of traditional probiotics are natural metabiotics. The terms "metabiotics", "metabolic probiotics", "postbiotics", "biological drugs" or "pharmacobiotics" are used to refer to small molecules that are structural components of probiotic (symbiotic) microorganisms and/or their metabolites, and/or signaling molecules with a specific (known) chemical structure that are capable of influencing the microbiome and/or metabolic and signaling pathways in humans. One of the representatives of metabiotics is Baktistatin.
The Baktistatin complex includes natural components that complement each other: sorbent, probiotic, prebiotic. One of the advantages of the Baktistatin complex is the absence of live bacteria foreign to the human gastrointestinal tract, the long-term presence of which in large quantities is undesirable. Instead of living bacteria, the Baktistatin complex includes products of their vital activity - active metabolites. Therefore, Baktistatin begins to work immediately, and its action is aimed at restoring one’s own normal microflora, which is unique to each person.
We conducted a study to evaluate the effectiveness and safety of the probiotic complex Baktistatin in treatment regimens for patients with candidal esophagitis and enterocolitis.
The study assessed the effectiveness and safety of 2 treatment regimens for esophageal and intestinal candidiasis in 2 groups: Group 1 – control, in which patients received etiotropic antifungal therapy; 2nd – the main group of patients in whom the Bactistatin complex is included in the above-mentioned therapy regimen.
In both groups of patients, selective decontamination with modern effective antifungal drugs of targeted action was carried out for 7–14 days. Patients in the main group additionally received Baktistatin, 2 capsules 2 times a day for 20 days.
To study clinical, endoscopic and laboratory indicators over time during the treatment of patients with candidal esophagitis and enterocolitis, a special questionnaire was developed, including a physical examination, gastroscopy, colonoscopy, and bacteriological examination of stool.
The results of comparing the scores of clinical symptoms showed that while taking the Baktistatin complex, manifestations of candidiasis of the esophagus and intestines went away faster. Thus, before treatment, the overall score for the severity of symptoms of candidal esophagitis was 355; after treatment, this figure decreased to 123 in the control group and to 60 in patients of the main group taking Bactistatin (Fig. 1). With regard to candidal enterocolitis, before treatment the total symptom severity score was 645, after treatment - 317 in the control group and 120 in the main group (Fig. 2).
In addition, the use of the Baktistatin complex in the treatment of gastrointestinal candidiasis significantly influenced the restoration of colon microbiocenosis due to an increase in the number of bifidobacteria and lactobacilli and a decrease in the number of enterobacteria, non-fermenting bacteria and fungi.
The data obtained indicate that the use of the metabiotic Baktistatin allows one to avoid the side effects of systemic antimycotics on the intestinal microflora and improve the condition of the esophagus and intestines in a short time due to a more pronounced reduction in the severity of the disease.
Thus, the use of the Baktistatin complex in treatment regimens for fungal infections of the gastrointestinal tract helps to quickly create conditions for the growth and functioning of normal microflora and reduce the side effects of systemic antimycotics.