Chronic tonsillitis: symptoms and treatment at home
Chronic tonsillitis is an inflammatory process localized in the palatine tonsils, which has taken on a sluggish, protracted form. The form of the disease is characterized by periodic relapses (recurrence at certain intervals in the presence of predisposing factors for acute episodes of the disease).
Considering that we are talking about an important organ that plays a decisive role in the chain of formation of the immune and physiological types of defense of the body, the importance of diagnosis and effective mechanisms for treating pathology among doctors is beyond doubt. This is an article prepared by our specialists based on materials from the work of practicing otolaryngologists.
What it is?
Chronic tonsillitis is a long-term inflammation of the pharyngeal and palatine tonsils (from the Latin tonsollitae - tonsil glands). Develops after a sore throat and other infectious diseases accompanied by inflammation of the mucous membrane of the pharynx (scarlet fever, measles, diphtheria), or without a previous acute illness.
Causes
Factors that contribute to the development of chronic tonsillitis in adults and children:
- allergic rhinitis;
- deviated nasal septum;
- decreased local and general immunity;
- frequent runny nose;
- inflammatory diseases that develop in other ENT organs;
- caries;
- the presence of foci of chronic infection in the human body;
- allergic mood of the body.
Chronic tonsillitis is an infection-dependent inflammatory process that develops as a result of the pathogenic activity of microorganisms. Normally, the tonsils in the body exist to trap infectious agents and prevent them from penetrating deeper into the respiratory tract. If there is a decrease in local or general defenses of the body, then pathogenic microorganisms that linger on the tonsils begin to actively develop and multiply, provoking the progression of the disease.
Tonsil abscess: symptoms, treatment, photo, opening, removal
Inflammatory processes localized in the pharynx area occur in the vast majority of people. Pain and sore throat often do not cause any concern, but it is completely in vain. Untreated laryngeal infections become foci of chronic infection, suppressing the immune system, and in some cases a disease such as tonsil abscess develops.
Tonsil abscess
An abscess is a hollow formation in the area of the tonsils and soft palate, filled with pus.
Visually, it may look like a swelling in the mouth, swelling on the side of the neck, or be completely invisible.
According to the classification of somatic pathologies, the disease has a special code J36.
There is no statistical data on which gender and age people are more likely to experience the disease. Therefore, information about tonsil abscess will be useful to every person.
An abscess is classified into at least two categories:
- tonsillar;
- paratonsillar.
The difference between these two types is that the peritonsillar abscess is symmetrical, affecting both tonsils.
Based on the immediate localization of the formation, they are distinguished:
- upper - upon examination it is clear that the tonsils move forward from the lacunae;
- external - the tonsils are clearly visible during visual inspection and almost cover the throat;
- internal - the formation of pus occurs inside the tissues of the tonsils;
- lower - the tonsils rise upward.
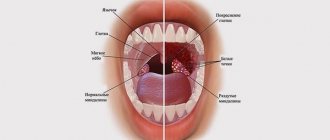
The photo shows a throat with tonsil abscess
Causes
All types of illness are provoked by tonsillitis - acute inflammation of the tissues of the larynx. In most cases, after the manifestations of sore throat decrease, the slightest hypothermia leads to a relapse of the disease.
An abscess forms in the tissues, but the person believes that this corresponds to the course of the disease and does not take timely action. People suffering from purulent sore throats are most at risk.
There are also factors that predispose to the development of pathology:
- diabetes;
- immunodeficiency, including AIDS or a decrease in the body’s defenses after an infection or taking antibiotics;
- smoking;
- frequent stress: psycho-emotional and physical;
- caries and other oral diseases;
- complications after tonsillectomy.
Symptoms
The most common symptom of a tonsil abscess is a sore throat. But the difficulty of diagnosis is that the disease traditionally occurs against the background of tonsillitis, pharyngitis or tonsillitis; it can be difficult to recognize the disease in its manifestation.
Therefore, the clinical picture is best considered in conjunction with other symptoms:
Despite the large number of symptoms, it is quite difficult to independently identify an abscess.
demonstration of examination of the throat and opening of the tonsil abscess:
Diagnostics and necessary studies
The diagnosis of pathology is carried out by an ENT doctor. First, he studies the patient’s history, finds out what he was sick with, whether he has chronic illnesses, what worries him at the moment. Then he examines the patient’s larynx for tissue inflammation and changes in the size of the tonsils and the symmetry of the larynx organs.
For more accurate diagnosis, the following are used:
These studies are necessary not only to confirm the diagnosis, but also to determine treatment tactics.
Tonsil abscess
Treatment
The goal of therapy is to open the abscess and relieve inflammation from the tissues. This can be done in two ways: surgically or through conservative treatment. As a rule, regardless of the choice of treatment method, the patient is offered inpatient treatment.
Medication
In order to achieve opening of the abscess without the intervention of a surgeon, heating the neck is used. At the same time, broad-spectrum antibiotics are used or, if there is a result of a throat smear, corresponding to the identified sensitivity spectrum.
Constant rinsing of the larynx is also necessary. The following can be used as rinses:
- salt solutions;
- furatsilin;
- decoction of oak or chamomile.
The larynx can also be irrigated with Miramistin.
If necessary, medications are prescribed for symptomatic treatment: against pain, fever, insomnia.
Surgical
If conservative treatment is ineffective, the issue of surgical treatment is decided. If the abscess can be easily removed, this is done under local anesthesia. But if the purulent formation is in a place inaccessible to low-traumatic intervention, the doctor may recommend removing the tonsils completely.
The same method can be recommended if resection of the abscess was previously carried out repeatedly, but then a relapse followed.
Opening a tonsil abscess:
Possible complications
Inflammation in the tonsil area can spread to other nearby tissues. Often, a tonsil abscess spreads to other organs of the respiratory system or to the soft tissues of the neck. There is also a risk of developing sepsis.
With a bilateral abscess, there is a risk of stenosis - closure of the throat with subsequent cessation of breathing. Death from this disease occurs infrequently, but is nevertheless possible.
In order to avoid the development of tonsil abscess, you must adhere to two rules:
Any diseases must be treated in a timely manner, preventing them from becoming chronic. Even caries can cause inflammation of the tonsils, and then an abscess.
Maintaining immunity at the proper level of activity is carried out through hardening, proper nutrition, and giving up bad habits.
Why an abscess is dangerous and how to treat it, watch our video:
Symptoms
Chronic tonsillitis in adults occurs with periods of remission and periods of exacerbation. With the development of an exacerbation, signs of tonsillitis (acute tonsillitis) develop:
- a sharp increase in body temperature to febrile levels (39-40 degrees);
- intense sore throat;
- regional lymph nodes enlarge;
- purulent plaque appears on the tonsils;
- There may also be purulent follicles on the mucous membrane of the tonsils.
During the period of remission, the patient may have the following symptoms of chronic tonsillitis:
- discomfort in the throat;
- feeling of a lump in the throat;
- slight pain in the morning;
- bad breath;
- plugs on the tonsils;
- small accumulations of pus in the lacunae.
Also, in addition to the signs of tonsillitis itself, there may be symptoms of concomitant diseases - chronic pharyngitis, rhinitis, sinusitis.
With the development of the decompensated form, the following symptoms appear:
- increased fatigue;
- general malaise;
- headache;
- prolonged low-grade fever (temperature stays around 37 degrees).
In addition, signs of complications may appear. The most common complication in the decompensated form of chronic tonsillitis is a peritonsillar abscess.
It begins as a sore throat, but later the patient cannot swallow or open his mouth at all. There is pronounced swelling of the pharyngeal tissue. The patient requires urgent medical care and hospitalization. Exacerbation of chronic tonsillitis can be triggered by hypothermia, an acute respiratory viral infection, or drinking cold drinks or food.
Infectious mononucleosis
This disease is also typical mainly for children, it is often confused with manifestations of a cold or acute respiratory infection, but it is caused by the Epstein-Barr virus, which is transmitted by airborne droplets and goes straight to the mucous membrane, where it begins to affect the nasopharynx, tonsils and lymph nodes, resulting in purulent tonsils and plaque appear on them, as in the photo. Hence, difficulty breathing, hoarseness of voice, and snoring in sleep. The main goal of the virus in this disease is to damage lymphocytes, which are one of the main cells of the immune system.
Infectious mononucleosis looks like this
As you can see, there are a lot of options why you might have pus in your tonsils. This is fraught with intoxication of the body, which will affect the digestive tract, liver, spleen, kidneys, cardiovascular system, and blood composition. To prevent this from happening, it is important to undergo treatment on time, and we suggest we talk about it further.
Diagnostics
During the examination, the doctor palpates the lymph nodes and examines the tonsils directly. But experts do not limit themselves to this, given how many complications can be caused by this disease. The contents of the lacunae are also sampled and sent for analysis. Taking material for laboratory testing is carried out by pressing on the tonsil, from which pus is released. If the pus has a mucous structure and an unpleasant odor, then most likely there is a chronic form of tonsillitis. But even this analysis cannot show the complete clinical picture and accurately determine the diagnosis.
To make an accurate diagnosis, doctors pay attention to the general condition of the body and the presence of deviations from the norm. Such deviations are primarily considered to be thickened edges of the palatine arches and hyperthermia. Experts also determine cicatricial adhesions between the palatine arches and tonsils.
Tonsils, in the chronic form of tonsillitis, have a loose appearance and a scar-altered surface. In the lacunae of the tonsils there are purulent plugs or purulent discharge.
Advantages and disadvantages of the pus removal procedure
It is necessary to remove pus from the tonsils in severe cases of the disease in a medical facility. Ulcers are containers where there is a large accumulation of various bacteria. After two days of antibiotic therapy, pathogenic microorganisms are destroyed. When the infection is defeated, the pus stops secreting, and the plugs disappear after 3–4 days.
If you do not remove the inflammation from a purulent sore throat, but simply start fighting the traffic jams, the patient’s condition will only worsen. There is a risk of reappearance of purulent discharge on the tonsils, and irritation and inflammation of the mucous membrane will cause an increase in temperature.
The situation will lead to the spread of infection and damage to the mucous membrane. When you cleanse your throat with hard objects on your own, the pus seeps even deeper.
Consequences
When tonsillitis becomes chronic, the body's immune response decreases, which can affect the functioning of internal organs. In severe cases, when symptoms of intoxication appear, some complications develop.
Prolonged infections lead to complications associated with cardiac dysfunction and kidney disease. Often, advanced tonsillitis is accompanied by rheumatism and tonsillocardial syndrome. Serious damage to health is caused by toxins that are released during sore throats.
Possible complications
Cellulitis of the neck
Purulent formations are dangerous because they spread through the circulatory and lymphatic systems, which leads to diseases of the kidneys, heart or joints. Treatment cannot be put off for a long time; if the disease is neglected, the following complications are possible:
- Peritonsillar abscess. If pus gets into the tissue, the neck begins to swell and the pain intensifies. Treatment requires surgery, which involves suctioning out the pus.
- Mediastinitis. Pus enters the neck, thereby causing swelling of the tonsils, which makes breathing difficult. This complication can be fatal.
- Cellulitis of the neck and general blood sepsis.
- Septic arthritis.
Do not delay treatment; at the slightest symptoms, you should consult a doctor.
Treatment of chronic tonsillitis
When treating a compensated form and in the absence of complications, chronic tonsillitis is treated conservatively at home using effective drugs. If the patient has signs of decompensation of chronic tonsillitis and complications develop, then surgical intervention may be required.
First of all, measures are taken to strengthen the body's defenses - proper nutrition, reduction of bad habits. If there are concomitant diseases, which are also sources of constant infection, they need to be cured:
- mandatory sanitation of the oral cavity - treatment of inflammatory diseases (caries, stomatitis);
- treatment of sinusitis, pharyngitis, rhinitis.
How to treat chronic tonsillitis: list of drugs
For the conservative treatment of chronic tonsillitis in adults, the following drugs are used:
- Antibiotics for tonsillitis. This group of drugs is prescribed only in the presence of an exacerbation of chronic tonsillitis; antibiotic therapy is recommended based on tank data. sowing. It is not worth prescribing drugs blindly, as this can cause a lack of effect and loss of time, not to mention side effects and worsening of the condition. Depending on the severity of the inflammatory process in sore throat, the doctor may prescribe a short course of the safest and easiest remedies, since with long courses of strong drugs it is necessary to supplement the treatment with a course of probiotics. In the latent course of chronic tonsillitis, treatment with antimicrobial drugs is not indicated, since this additionally disrupts the microflora of the oral cavity and gastrointestinal tract, and also provokes immune suppression.
- Painkillers. For severe pain, the most optimal is Ibuprofen or Nurofen; they are used as symptomatic therapy and for minor pain their use is not advisable (see the full list and prices of non-steroidal anti-inflammatory drugs in the article Injections for back pain).
- Probiotics. When prescribing aggressive forms of broad-spectrum antibiotics and in the presence of concomitant gastrointestinal pathologies (reflux, colitis, gastritis), before taking antibiotics, it is necessary to take probiotics that are resistant to the action of the former - “Normoflorin”, “Gastrofarm”, “Primadofilus”, “Narine”, "Rela Life", "Acipol".
- Antihistamines. To reduce swelling of the mucous membrane, tonsils, and swelling of the posterior pharyngeal wall, you need to take desensitizing medications; they will also contribute to better absorption of other medications. From this group of drugs, it is better to use the latest generation of drugs, since they have a prolonged effect and do not have a sedative effect, they are safer and stronger. Among the antihistamines, the best are Fexofast, Fexadin, Telfast, Zodak, Letizen, Zirtec, Parlazin, Cetrin.
- Antiseptic local treatment. An important condition for effective treatment is gargling; for this you can use various solutions, either ready-made sprays or dilute special solutions yourself. It is most convenient to use Miramistin (250 rubles), which is sold with a 0.01% solution spray, Octenisept (230-370 rubles), which is diluted with water 1/5, as well as Dioxidin (1% solution 200 rubles 10 ampoules), 1 amp. diluted in 100 ml of warm water (see list of all throat sprays). Aromatherapy can also have a positive effect if you gargle or inhale with essential oils - lavender, tea tree, eucalyptus, cedar.
- Antiseptic local treatment. An important condition for effective therapy is gargling. For these purposes, you can use both ready-made sprays and self-prepared solutions. It is most convenient to use Miramistin 0.01% solution, Octenisept, Dioxylin, which are diluted with warm water. Aromatherapy also has a positive effect if you gargle and inhale with essential oils - cedar, eucalyptus, tea tree, lavender.
- Immunostimulating therapy. Among the drugs that can be used to stimulate local immunity in the oral cavity, perhaps only Imudon is indicated for use, the course of therapy is 10 days (absorbable tablets 4 times a day). Among the products of natural origin, you can use Propolis, Pantocrine, ginseng, and chamomile to boost immunity.
- Emollients. Inflammation in the throat and taking certain medications may cause dry mouth, sore throat, and sore throat; in such cases, it is effective to use sea buckthorn, peach, and apricot oils, provided there is no individual intolerance to them. In order to soften the nasopharynx well, you can instill one of the oils into the nose in the morning and evening, a few drops at a time, during the procedure you should throw your head back. Another method of softening the throat is 3% hydrogen peroxide, which is used to gargle for as long as possible, after which the mouth is rinsed with warm water.
Purulent plugs in chronic tonsillitis
Pus on the tonsils (tonsils). How to treat? Reasons for education
Pus on the tonsils is not such a rare occurrence.
Almost every person has encountered it at least once in their life, and some have encountered a similar symptom more than once. Pus inside the tonsil with an unpleasant odor is the first sign of tonsillitis and chronic tonsillitis.
There are also other diseases in which suspicious plaque can be detected on the tonsils.
Before you begin to eliminate this symptom, you need to understand when it appears and what to do in each specific case.
If the ulcers on the tonsils are small and the body temperature does not rise, then clinical symptoms may be absent, or they are not pronounced: a slight tingling sensation when swallowing, an unpleasant taste in the mouth.
With a prolonged course of the inflammatory process, pus accumulates in the tonsils with food and bacteria. As a result, a hard coating with plugs is formed, the tonsils become swollen and increase in size.
Typically, such a sluggish process is characteristic of chronic tonsillitis. Liquid pus constantly appears in the lacunae.
If there are many abscesses on the tonsils, they tend to merge, occupy a large surface, then the person has a sore throat, a feeling of burning, tingling, and discomfort in the pharynx area at rest.
Symptoms intensify when swallowing food or saliva. One of the first symptoms is a feeling of putrid breath, which is explained by the sulfur content in plaque.
Toxic substances released by pathogenic microorganisms enter the bloodstream and cause a violent general reaction of the body: increased body temperature, chills, weakness, depression, fatigue, malaise.
Such a rapid development of the disease is characteristic of acute tonsillitis, commonly known as purulent tonsillitis. Source: nasmorkam.net
It is believed that pus in the lacunae of the tonsils in children is a fairly common situation. Typically, this phenomenon affects children with reduced immunity and prone to frequent sore throats.
Any questionable overlap of the posterior pharyngeal wall in a child should be shown to a specialist, since early diagnosis affects the effectiveness of treatment.
The doctor will prescribe an additional examination and select appropriate therapy. If all recommendations are followed, pathological formations in the throat completely disappear without complications.
There are other, more rare cases when a white coating in the throat is not accompanied by an increase in temperature:
Traumatic damage to the tonsils is possible when eating solid foods (chicken, fish bones, crackers). The wound surface at the site of injury is covered with a whitish film, similar in appearance to bacterial plaque.
Fungal infection of the mucous membranes of the oral cavity, known to everyone as thrush, develops with reduced immunity due to prolonged treatment with antibiotics, cytostatics, and hormonal drugs.
In this case, specific white deposits sometimes form on the tonsils. They are often mistaken for pus.
Cystic formations on the tonsils are similar in appearance to ulcers. When they reach large sizes, they begin to cause discomfort.
Oral diseases (periodontal disease, caries) lead to the formation of ulcers on the gums, palate, and sometimes tonsils. During their regeneration, a white film resembling pus is formed. Sometimes fermented milk products, which linger in the crypts of the lymphoid glands, are mistaken for purulent plaque.
When to see a doctor: how does an ENT remove pus from the tonsils?
You need to contact an ENT doctor:
- With extensive raid.
- Pus on the tonsil on one side.
- In case of a pronounced systemic reaction of the body (fever, chills, sweating).
- Ulcers appear regularly.
The doctor decides how to remove the plugs and how to clean the tonsils during the examination.
To remove pus from the tonsils, the ENT doctor uses:
1
Sanitation of the tonsils - washing the lacunae with a syringe or sucking out the pus using a vacuum method. Using a special syringe, the doctor rinses the lacunae with antiseptic substances under pressure. This is the most common and accessible method.
The vacuum method is more effective. Using a special device, pus is sucked out of the tonsils. The cleaned lacunae are filled with medicine.
2
Physiotherapy helps cleanse the tissues in the throat, reduces swelling and inflammation. There are several types of physiotherapy used to treat the ENT organs.
Ultraviolet irradiation
- has a bactericidal effect, helps remove pus from the tonsils during tonsillitis.
Laser exposure
has an antimicrobial effect, improves blood and lymph circulation in inflamed tissues.
Ultrasound is a method
with the help of which drugs with a therapeutic effect (antibiotics, hydrocortisone, dioxidine) are introduced deep into the soft tissues.
3
Laser cryptolysis is a promising method for treating tonsils using radio waves. The essence of the method is to clean the crypts from foreign substances, sterilize them, and then seal them. The method allows you to get rid of plaque in 2-3 approaches completely and for life.
Diagnosis of diseases begins with detailing complaints and collecting anamnesis. An ENT doctor can make a preliminary diagnosis by examining the pharynx, assessing the condition of the throat and the nature of the plaque.
Identification of the pathogen that caused the disease is mandatory. For this, a throat swab is prescribed.
If necessary, additional studies are prescribed.
General blood analysis
allows you to determine the body's response to the inflammatory process.
Blood chemistry
with the detection of C-reactive protein, antistreptolysin-O, rheumatoid factor is prescribed if a streptococcal etiology of the disease is suspected.
Electrocardiography
may be needed to assess heart function in complicated diseases.
Pus on the tonsils: treatment
Treatment of purulent plaque is a set of measures aimed at removing the pathogen from the body, alleviating unpleasant symptoms and cleansing the tonsils.
Pharmaceutical drugs are the most effective part of drug therapy.
Drug treatment
All medications for treating the throat can be divided into two groups: general and local action. They complement each other, and also allow you to quickly get rid of the painful manifestations of diseases.
Systemic drugs:
Antibiotics.
They occupy first place in the treatment of tonsillitis. The drugs of choice with a wide spectrum of action are penicillins (Amoxiclav, Augmentin), cephalosporins (Zinnat, Cefuroxime), macrolides (Erythromycin).
Antihistamines
(Suprastin, Zodak, Tavegil). Slightly reduce irritation and pain in the throat, reduce tissue swelling.
Antipyretic drugs.
Used when body temperature rises.
It is preferable to take medications based on paracetamol, ibuprofen (Panadol, Nurofen), as they have fewer side effects. Local treatment includes gargling and throat sprays.
Rinsing is carried out with antiseptic solutions, decoctions, and infusions of medicinal herbs. The method allows you to partially wash out the purulent plugs in the lacunae.
Most often used:
- Saline solution. Prepare by adding a tablespoon of table salt to one glass of warm water.
- Sea water. The prepared solution is sold at the pharmacy.
- Soda solution. A teaspoon of baking soda is added to a glass of warm water.
- Furacillin. The ready-made solution is commercially available, or the tablet form of Furacilin is dissolved in warm boiled water and used according to the instructions.
- Sage infusion has an antimicrobial and calming effect. Prepared by infusing a teaspoon of sage in a glass of hot water for an hour.
How to gargle effectively:
- Take the solution into your mouth, tilt your head back and pronounce the sound “Y”. This facilitates irrigation of a larger area of the affected surface with the medicine.
- During the first days of the disease, you should alternately use different solutions for rinsing every 1-2 hours. After inflammation subsides, the interval can be reduced to 3-4 hours.
- After rinsing, do not drink or eat for half an hour.
- Children should gargle under adult supervision.
Irrigation of the throat with sprays that have an antibacterial (Bioparox, Faringosept, Gramicidin) or antiseptic (Cameton, Ingalipt, Tantum Verde, Lugol's solution) effect.
Depending on the constituent components, drugs can additionally have anti-inflammatory, analgesic, enveloping, wound-healing, softening, and moisturizing effects.
Folk remedies at home
The disease can be effectively managed. But it is necessary to understand that these methods should not be used independently, but only in conjunction with traditional medicine.
Before treating your throat with folk remedies, you should consult your doctor.
1
Gargling with chamomile decoction, which has a weak antiseptic, healing, anti-inflammatory effect. To prepare such a decoction, you need to pour two tablespoons of chamomile flowers into a glass of hot water.
2
Calendula tincture has an antimicrobial effect and reduces inflammation. The finished infusion is sold at the pharmacy. Mix a teaspoon of this solution with a glass of warm water and gargle several times a day.
3
Rosehip infusion has a strengthening and stimulating effect on the immune system. To prepare it, 40 grams of rose hips are poured with boiling water in a thermos and left to steep for 10 hours. Used instead of tea for oral administration.
4
Tea with lemon normalizes metabolic processes and increases the body's protective properties. Thanks to the vitamin C content in lemon, this tea helps relieve inflammation.
5
Chewing propolis has a softening, antibacterial, anti-inflammatory, and analgesic effect on the throat. It should be remembered that propolis, like any beekeeping product, is highly allergenic.
Therefore, it is used with caution, especially in persons predisposed to allergies. It is recommended to chew propolis up to 3 times a day for 15 minutes. [ads-pc-1][ads-mob-1]
How to remove pus from tonsils yourself: can you squeeze it out?
It is not recommended to remove any deposits or formations on the tonsils yourself.
This can lead to injury to the mucous membrane if handled carelessly.
In addition, the products used may have a burning effect. As a result, such amateur activities can aggravate the underlying disease.
Currently, a popular method is when the patient, standing in front of a mirror, uses a cotton swab to press on the tonsil. When pressed, pus flows out or a hard plug comes out.
However, if excessive force is applied, surrounding tissues can become infected. Also, ulcers can be squeezed deep into the tissues and lead to the formation of an abscess.
Therefore, removing pus from the tonsils using this method should be done with caution, and it is better to entrust it to a specialist.
Prevention
- Varied and nutritious food.
- Avoid contact with infectious patients.
- Avoid hypothermia.
- Boosting immunity through vitamin therapy, hardening procedures, and daily walks in the fresh air.
- Prevention, treatment of chronic foci of infections (caries, sinusitis, chronic tonsillitis).
- Compliance with personal hygiene rules.
Share with friends
Source: //nasmorkam.net/gnoj-na-glandax-mindalinax-kak-lechit/
Physiotherapeutic methods
Physiotherapeutic treatment of chronic tonsillitis can be effective during remission - laser therapy is recognized as very effective due to its antibacterial and anti-inflammatory effect due to its direct effect on the tonsils. Short-wave UV radiation of the throat and oral cavity is also used.
There are methods of ultrasonic treatment of the tonsils, which act on the source of the disease itself, destroying the structure of the resulting cheesy mass. Using ultrasound, you can also irrigate the tonsils with antiseptic solutions.
An effective remedy is inhalation of wet steam. But there is one contraindication here - high temperature, so the temperature must first be lowered, and only then inhalation. Inhalations can be used using various medicinal herbs - chamomile, calendula, etc., chlorhexidine solution, or you can simply breathe over potatoes. You should not take deep breaths when inhaling, because in the case of tonsillitis, only the inflamed tonsils need to be affected.
Treating tonsillitis at home
Let's look at some of the most interesting recipes for treating tonsillitis at home, which include honey and its derivatives:
- For oral administration, prepare half and half onion juice and honey. Mix thoroughly and drink 1 teaspoon 3 times a day;
- Mix chamomile flowers and oak bark in proportions 3:2. Pour four tablespoons of the mixture into 1 liter of hot water and boil over low heat for 10 minutes. Before turning off, add a tablespoon of linden flowers. Let cool, strain, add a teaspoon of honey to the solution. Mix thoroughly and gargle while warm.
- To lubricate the tonsils, prepare a mixture consisting of 1/3 freshly squeezed aloe leaf juice and 2/3 natural honey. The mixture is carefully mixed and stored in the refrigerator. Before use, the medicinal composition must be warmed to 38-40 degrees Celsius. Using a wooden or plastic spatula, the composition is carefully applied to the sore tonsils 1-2 times a day, at least 2 hours before meals. Repeat treatment daily for two weeks. Then the procedure is done every other day.
Surgical treatment
Such treatment is mainly carried out when decompensated chronic tonsillitis is detected and in the absence of a positive effect from repeated conservative treatment.
A tonsillectomy can be complete or partial. A total tonsillectomy involves total excision of the affected tonsils. Partial tonsillectomy can reduce the size of enlarged tonsils, but this operation is now rarely performed due to the high risk of relapse of the disease. Rare types of surgical treatment include galvanocaustics and diathermocoagulation.
New types of treatment for tonsillitis include laser lacunotomy, an operation to remove the tonsils is performed using a surgical laser. It is possible to carry out such treatment using surgical ultrasound.
Cryodestruction – freezing the tonsils with liquid nitrogen – is gaining popularity. Its use is justified with a slight increase in the size of the tonsils.
Tonsillectomy (removal of tonsils)
Prevention
Prevention of exacerbations of chronic tonsillitis:
- Compliance with the rules of hygiene of home and work premises.
- Elimination of dust and air pollution.
- General hygiene measures.
- Hardening.
- Balanced diet.
- Sanitation measures: identification and treatment of diseases of the gums and teeth, sinusitis, otitis media, nasal breathing disorders.
It should be noted that even the implementation of all of the above measures does not at all guarantee the exclusion of relapses.
Respiratory diphtheria
This is a serious infection, which, in addition to the formation of large gray or white ulcers on the throat and swollen tonsils, as in the photo, is characterized by fever, inflammation of the lymph nodes, difficulty not only in eating and swallowing, but even in breathing.
This is what respiratory diphtheria looks like
It may be helpful for you to know that the best way to prevent diphtheria is through vaccination,1 which was first invented in the 1920s. This is what has made it possible to sharply reduce the number of children and adults with this disease. To this day, the vaccine is given at the age of 2.4 and 6 months (if there are no contraindications), then it is recommended to repeat it at the age of 18 months and when the child reaches 6 years. Further, after 16 years, it can be repeated every 10 years of life. Today, vaccines of this type make it possible to stop several infectious agents at once: diphtheria, whooping cough, tetanus.
What do you think about mandatory vaccinations? Do you think that they should be done for children or will all this only bring harm? We are waiting for answers in the comments>>>