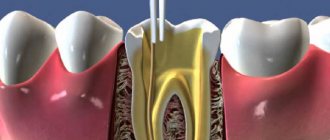
Root canal obturation is the final stage of endodontic treatment. Since you have already done the main thing that prevents the development of complications - preparation and irrigation - all that remains is to seal the root canal system three-dimensionally.
Obturation is the goal of mechanical and medicinal treatment, because first we must create conditions for filling, and only then proceed with it.
The long-term positive prognosis of the tooth is influenced by the tightness of the root canal filling throughout its entire length, the quality of the restoration, whether temporary or permanent, and, as a consequence, the absence of periapical changes in the bone.
It has now been found that microleakages are inevitable with any obturation, but it should eliminate them as much as possible. It should be remembered that adequate coronal restoration prevents the penetration of oral fluid into the root canals, and sealing the apex reduces the risk of fluid leakage from the periapical tissues.
Many people ask whether it matters what kind of filling they put - temporary or permanent.
Unambiguous results were never achieved, but most doctors claim that there is no difference in quickly replacing a temporary filling with a permanent one, with mandatory consideration of sealing. It is also not necessary to delay replacement for several months in order to prevent complications. Clinicians claim that cast structures on endodontically treated teeth prevent leakage better than any other.
The prognosis for tooth preservation is influenced by the reason for endodontic treatment. It has been studied that endodontic treatment due to apical periodontitis reduces the percentage of tooth “survival”. Taking into account the fact that instrumentation does not completely treat the canal walls - in some places they remain intact - and drug treatment does not always remove debris from the lateral canaliculi, teeth with changes at the apex are more difficult to treat than teeth without changes. Interestingly, the treatment success rate for primary and secondary endodontics is the same.
Despite all the arguments, obstruction plays a large and significant role in determining the success of treatment. Therefore, you should always properly process the canal with endodontic instruments, thoroughly rinse and obturate throughout, evenly, tightly, to the entire working length and without gaps.
Master pin
A very exciting question for everyone is: “To what level is it optimal to place the master pin and what deviations are allowed?”
For a long time it was believed that the stop signal was the dentinal-cemental junction. Later, the concepts of apical narrowing and apex began to be distinguished - anatomical and radiological.
Physiological narrowing is the point of transition between endodont and periodontium; the walls of the canal in this place are made of cement. The narrowest point is at the top.
Anatomical apex is the anatomical tip of the tooth root.
X-ray apex – image of the anatomical apex on the Rh-gram.
The dentin-cementum boundary is not a guideline for installing a master pin in the canal due to its discrepancy with the apical narrowing and different values on different walls of the root canal.
At the apex of the root there is an apical foramen, which is not always located strictly in the center of the axis of the tooth root. From the apical foramen to the narrowing, according to various sources, there is a distance of about 0.5 mm. From the hole to the root tip is about 2.5 mm. This distance may vary due to age.
With these data, it is clear that radiographic apex should not be relied upon as there is a significant potential for material leakage.
If the pulp was vital before treatment, then excessive pressure of the filling material may cause inflammation in the periodontium. If the pulp was necrotic, then the lateral tubules should be thoroughly washed with an irrigant, having previously activated it.
Causes of obliteration of tooth canals
The main and most common causes of tooth root obliteration are:
- injuries;
- chronic inflammatory processes;
- age-related changes;
- poor quality treatment;
- the presence of cancer associated with the proliferation of connective tissue.
There are also factors that increase the likelihood of root canal obliteration. These include:
- malocclusion;
- heredity (in particular with marble disease and Stanton-Capdepont syndrome);
- metabolic and endocrine system disorders;
- exposure to chemicals on teeth over a long period of time;
- decreased functionality or inactivity of the tooth during chewing.
Difficulties in root canal treatment
Author: Bobby Patel
Translation: Zvorykin Sergey
Denticles and calcifications
To locate the sclerosed canal orifices, the clinician must first visualize and evaluate the size of the pulp chamber on a two-dimensional radiographic film. You should begin preparation by mentally imagining a picture of their location and directing the bur to the expected location of the root canal mouths.
Before starting treatment, it is necessary to obtain a high-quality targeted x-ray so that you can imagine the depth to which the bur should be immersed (usually the distance from the occlusal surface to the bottom of the pulp chamber is approximately 6.5 mm). Teeth that have undergone a pronounced process of obliteration and with a small volume of the pulp chamber require special attention and caution during the preparation process. Preparation to reach the tooth cavity should be less diligent, as overzealous preparation can lead to iatrogenic perforation. Teeth that have been crowned also require appropriate assessment of the crown-root orientation to allow proper preparation to access the canals (see Figures 1, 2 and 3).
Figure 1. Clinical radiograph and photographs showing (a) preoperative radiograph showing the radiolucent area associated with the 36th tooth. The referring physician performed emergency pulp extirpation but had difficulty identifying the “calcified canals.” Intraoperative photographs obtained using a microscope show
Figure 1 (b) Intraoperative microscopic images show an intact pulp chamber.
Figure 1 (c, d) view after complete removal of the chamber roof and operation of ultrasonic tips to determine the internal anatomy with direct access to all four channels. The canals can be easily processed along their entire length.
Figure 1(d) (continued).
Figure 2. Clinical radiograph and photographs showing (a) preoperative radiograph showing an obliterated pulp chamber (black arrow). Tooth 16 with irreversible pulpitis and a history of cracking.
Figure 2 (b) Bitewing radiograph confirms the presence of a radiopaque mass in the coronal portion of the pulp chamber and is suggestive of denticles. The preparation depth can be measured before the access begins.
Figure 2 (c) After opening
Obliteration of root canals. Clinical case.
A patient contacted us. The orthopantomogram image clearly shows complete obliteration of the lumen of the root canal of the 21st tooth.
Fig. 1 Complete obliteration of the root canal of the 21st tooth on an orthopantomogram
Diagnosis was made using cone beam computed tomography (CBCT).
Rice. 2 Sagittal section of the area of the 21st tooth on a CBCT image
Taking into account the skeletal asymmetry of the lower jaw in the image, the main cause of obliteration of the root canal in this case can be assumed to be trauma.
Rice. 3 Axial section of the upper jaw area with obliteration of the root canal of tooth 21
Medical Internet conferences
Tooth perforation is the formation of a pathological communication between the internal cavities and canals of the tooth with the surrounding tissues.
The reasons for the development of this complication:
1. Insufficient opening of the tooth cavity;
2. Insufficient knowledge of the topography of the dental cavity;
3. Wrong choice of tool and violation of the methodology for its use;
4. Excessive expansion of the mouths;
5. Significant bends of the root canals.
Clinically, perforation of the bottom or walls of a tooth manifests itself in the form of a characteristic “sinking” of the instrument, bleeding and sharp pain in the patient in the case of treatment without anesthesia, and probing in the perforation area also causes acute pain. However, for a more accurate diagnosis of perforation, an apex locator and x-ray should be used. The best prognosis is observed in cases where the perforation is closed immediately, which minimizes trauma and infection of surrounding tissue. The most unfavorable localization of perforation is the area of root furcation. Almost any perforation in this area leads to destructive changes in the periodontium [1].
The main goal of endodontic treatment is to eliminate infection and restore the integrity of the body's tissue barriers against microbial invasion. Materials that come into contact with living tissues must be biocompatible. There are many materials available for closing perforations: amalgam, composites, and glass ionomer cements. The main negative properties of these materials are microleakage, toxicity, and sensitivity to moisture. The ProRoot MTA material does not have all these disadvantages.
This material was developed at Loma Linda University (USA, California) by Professor of the Department of Endodontics Mahmoud Torabinejad [2].
The ProRoot MTA (Mineral Trioxide Aggregate) system is a powder consisting of small hydrophilic particles that turn into a solid cement paste in the presence of water due to hydration of the powder in less than four hours.
Composition: 75% Portland cement, 20% bismuth oxide, 5% dehydrated calcium sulfate [3].
Indications for use of the material:
1. perforation of the root and bifurcation area;
2. vital amputation;
3. apexification;
4. retrograde filling of the root apex;
5. elimination of root resorption [4].
Method of using the ProRoot MTA system to restore root canal perforation:
1. Having applied a rubber dam, we clean the root canal of sawdust and half-life products;
2. Dry the root canal system with paper points and isolate the perforation site;
3. Obturate all canals located apically from the perforation;
4. Prepare the ProRoot MTA material in accordance with the attached instructions;
5. Using the supplied application probe, place the material in the defect area. We compact the material in the cavity;
6. We make sure that the material is placed correctly using an x-ray;
7. Place a moistened cotton swab into the cavity and fill the canal with temporary restoration material for at least 4 hours;
8. After 4 hours, or during the next appointment, we inspect the ProRoot MTA material. The material must be hard. If this is not the case, wash and repeat application;
9. When the material has hardened, we obturate the remaining part of the canals. ProRoot MTA should remain as a permanent part of the root canal filling [5, 6].
Treatment methods for root canal obliteration
Treatment of a tooth with root canal obliteration is quite difficult. Most often, in such cases, surgical removal of the part of the tooth affected by the pathological process is used, as well as chemical devitalization, in which tissue mummification is performed using special injections.
Treatment of root canal obliteration is a rather painful procedure, since due to the obstruction of the tooth patency, injection anesthesia is ineffective. The complexity of treatment causes the possibility of complications. These include perforation of the root canal and/or dental crown and possible pain due to incomplete elimination of canal obstruction.
Posted in Articles | Tags: 3-D CT, clinical case, CBCT
New technologies for problematic channels
Pulpitis and periodontitis are still the main reasons for tooth extraction. Teeth with elements of destruction at the root apex are foci of chronic infection, sometimes leading to systemic diseases. Many authors attribute the presence of additional unopened canals and great difficulties in monitoring the passage of the canal and its filling as reasons for the low quality of canal sanitation. Back in 1970, Mayer presented reconstructed models of tooth roots, which show how many lateral branches a root canal can have and how extensive the apical delta can be (Fig. 1).
Currently, more and more supporters are gaining the point of view that modern instrumental-mechanical endodontics is fundamentally unable to solve the problems of combating root infection.
Fig. 1 Variants of the apical delta of root canals
Fig. 2 Cross sections of teeth showing difficult canals
By measuring electrical conductivity with the main hole well open and carefully insulated with varnish prof. A. Knappvost revealed that 70-90% of the flow of substances entering the pulp passes through the lateral (!) canals of the apical delta. The work of Noldin (1994) shows the shapes of channels that are poorly accessible to mechanical instruments (Fig. 2).
At the same time, only complete sterility of the entire canal system is a prerequisite for effective sanitation.
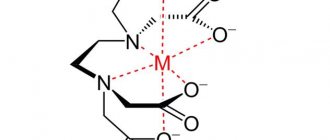
Based on the previously known methods of electrophoresis and iontophoresis of Prof. A. Knappvost has developed a technology for successfully resolving endodontic problems using a unique technology of depophoresis of a substance new to dentists - an aqueous suspension of copper-calcium hydroxide, which has exceptional bactericidal and physicochemical properties.
During treatment under the influence of an electric field, from the depot of the above-mentioned suspension created in the root canal, OH-ions and hydroxycuprate ions [Cu(OH)], which have a strong bactericidal effect, penetrate into the entire canal system, including secondary and lateral canals, up to the openings.
As a result of this, the following processes occur that underlie the therapeutic effect of electrophoresis:
- Proteolysis of biological tissue residues located in the canal system. (Professor A. Knappvost speaks of sterile oligopeptides and saponification mycelia, which, after leaving the canal system, are resorbed by the body).
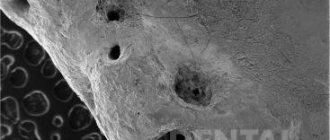
- Killing remaining microorganisms by removing sulfur from amino acids. Fig. 3 At the apexes of the roots, copper “plugs” are clearly visible, tightly obliterating all exits of the apical delta to the cement surface
- Lining the unfilled part of the root canal, as well as all microcanals, with copper-calcium hydroxide, which ensures long-term sterility and also stimulates the formation of bone tissue in the area of microholes (Fig. 3).
- Stimulation of osteoblast activity in the periapical region as a result of alkalization.
Clinical practice
This method is suitable for the treatment of all gangrenous teeth. Especially for difficult-to-reach, partially obliterated and/or severely curved canals, the depophoresis method is the preferred and sometimes the only feasible alternative to traditional methods. After trephination of the tooth, the pulp chamber is opened in the usual way and the orifices of the canals are exposed. The canal is prepared over up to 2/3 of the length, and a width of ISO 35-50 is quite sufficient. It is advisable to expand the channel in the third closest to the mouth a little more in order to create a sufficient depot of the copper-calcium hydroxide suspension. We use the “Original II” device (Fig. 4). A negative needle electrode is inserted into the canal to a depth of 4-8 mm. (The electrode is not secured with any sticky wax.) The positive electrode is placed behind the cheek on the opposite side so that it does not touch the dentition. To reliably ensure the distance and for better conductivity, place a damp cotton swab between the electrode and the cheek. It is recommended to lubricate the corner of the patient's mouth with Vaseline. (The procedure is not performed in a physiotherapy room, but in the doctor’s chair).
Fig.4 Appearance of the “Original-11” device
Turn on the device and slowly increase the current until the patient signals, for example with his hand, that a feeling of warmth or tingling appears in the root area. (This is agreed upon with the patient in advance).
The current is reduced and increased again even more slowly, usually reaching 1 to 2 milliamps (mA). The session lasts 2-5 minutes. The required amount of electricity received by the patient is 5 mA X min.
Using the described method, you should influence each channel separately. During the procedure, bubbles are released from copper-calcium hydroxide into the cavity, which, especially if the tooth is covered with a crown, must be removed from time to time with a swab to avoid the discharge of electric current. Care should be taken that during depophoresis the needle electrode does not come into contact with the metal edge of the crown or filling. This will relieve the patient from unpleasant effects.
Finally, the channels and cavity are washed with distilled water or a 10% suspension of simple calcium hydroxide, but a diluted suspension of copper-calcium hydroxide itself can also be used).
As a tab until the next session, which is usually carried out after 8-10 days, after drying the canal, a fresh portion of copper-calcium hydroxide paste is injected. In most cases, three treatment sessions are sufficient to ensure treatment success. The patient must receive a total amount of electricity per channel (that is, the product of mA X minutes) equal to 15. After the last procedure, the entrance to the channel is filled with atatasamite, a special cement included in the kit (alkaline, copper-containing material). The rest of the canal (up to 1/3 of the apical part) is not filled with anything at all.!!)
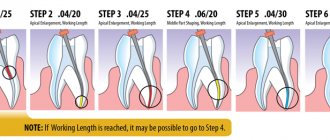
Steps demonstrating gradual sterilization of canals
PSHa time between treatment sessions, according to the recommendations of prof. A. Knappvost, the cavity can be left open to prevent the development of pressure during the outflow of the still formed exudate. Recontamination is practically excluded due to the powerful disinfectant activity of medicalcium hydroxide.
Dr.S.Rocholl (Germany) says: “This method personally seemed unreliable to me at first. However, gradually I became convinced that it was completely justified. Currently, in my practice, I almost always use the depophoresis method. Only in rare absolutely “clear” cases after vital extirpation of single-rooted teeth with straight canals and in the absence of apical changes do I use traditional methods.”
Main differences between depophoresis and traditional methods
| Actions | Depophoresis | Mechanical-instrumental method |
| Channel search | No difference | No difference |
| Channel preparation | The apical third is not affected | Expansion throughout the depth of the canal up to the physiological opening |
| Canal sterilization | Complete sterility of the entire apical delta | Reducing the number of microbes in the main channel. The apical delta is unreachable. |
| Canal filling | Only the mouth of the canal | Filling for Pulpitis up to 1-1.5 mm to the apex, for periodontitis - completely |
| Subsequent audit | Hassle-free | Problematic |
| Risk of complications | Insignificantly small | Quite big |
| Treatment success | About 96% | 40-60% |
Indications for treatment using depophoresis
General indications
- functional ability of the tooth in perspective
- possibility of crown reconstruction
- sufficient tooth stability despite periradicular tissue changes (granulomas, cysts)
- satisfactory general condition of the patient (as for other types of endodontic treatment)
Specific indications
- canals with gangrenous contents 4 severely deformed root
- obliterated canals
- after unsuccessful treatment or in the presence of a crown, if most of the root filling can be removed
- channels with wide opening
- after the so-called vital extirpation
Advantages of depophoresis compared to other endodontic methods
- reliably proven treatment success in 96% of cases
- much less loss of tooth substance and therefore preservation of mechanical stability of the root
- much lower risk of perforation
- no need for channel measurement
- minimal risk of the healing or filling substance leaving the root apex
- reliable sterilization of the entire apical delta
- no need for root apex resection
- increase in indications for successfully predicted endodontic treatment - severely curved roots, obliterated canals, wide main opening
- treatment of canals that are not accessible to an instrumental approach
- low probability of hematogenous reinfection
- Osseoid closure of the hole leads to complete physiological cure
- exceptional efficiency (saving time, money, effort of the doctor and patient)
Clinical case 1
Chronic periodontitis 5 bottom left. Depophoresis sessions with copper-calcium hydroxide were performed. Additional filling with gutta-percha/silapex not up to the apex
After 6 months, significant reduction of the lesion
Clinical case 2
Chronic periodontitis 7 bottom left
Image 12 months after 3 sessions of depophoresis and incomplete filling with atacamite - gutta-percha