From this article you will learn:
- what is tooth root cement,
- its structure and functions,
- histological preparations.
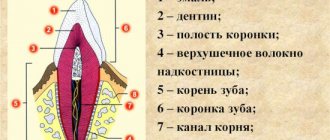
Dental cement (cementum) is a highly mineralized tissue, reminiscent in its structure of coarse-fiber bone, which covers the root of the tooth (up to its neck) with a thin layer. But unlike bone tissue, root cement is not subject to constant restructuring, it does not have vessels, and its trophism is carried out through the usual diffusion of nutrients dissolved in the main amorphous substance in the periodontal structure.
The main function of cement is to form the ligamentous apparatus of the tooth (periodontal attachment), which holds the tooth in the alveolus, and also contributes to the redistribution of chewing pressure from the tooth to the alveolar bone. Let us recall that periodontal fibers begin to grow simultaneously - both from the side of the root cement and from the side of the compact lamina of the alveoli. Next, with the help of immature collagen (procollagen) in the center of the periodontal fissure, the ends of these fibers are tied together, bundles of fibers are formed.
Tooth root cement: diagram and photo
The cementum layer is present only on human teeth, as well as on the teeth of other mammals. In the area of the tooth neck, the thickness of the cement is less - from 20 to 50 microns, while in the area of the root apex - from 100 to 150 microns. I think you are familiar with the fact that “secondary dentin” is produced by odontoblasts throughout life, and in the same way, constant formation of cement on the root surface occurs throughout life. And therefore, if you live to retirement age, the cement of your teeth will most likely have time to at least triple its thickness (Fig. 3).
Tooth root cement: structure
Cement is close in chemical composition and strength to coarse-fiber bone tissue. Inorganic components in the composition of cement make up approximately 65% - mainly calcium phosphate (in the form of hydroxyapatite crystals or amorphous calcium phosphates) and calcium carbonate. Organic components make up about 23%, and they are almost entirely represented by collagen; plus about 12% water.
Cementum is divided into 2 forms - primary (acellular) and secondary (cellular). A layer of primary cement lines the dentin of the entire surface of the tooth root, and in turn, a layer of secondary cement will be located on top of it. However, this so-called secondary “cellular cement” will no longer cover the entire surface of the root, but only its apical third + in multi-rooted teeth, also the area of bifurcation/trifurcation of the roots (Fig. 4).
Cement layers (electron microscopy) –
Cellular and acellular cementum (histology) –
1) Primary (acellular) cement –
Primary cement covers the entire tooth root. It does not contain cells, and consists only of calcified intercellular substance, which includes collagen fibers and the main amorphous “gluing” substance. The collagen fibers of this cement layer are characterized by uniform mineralization, and some of them have a longitudinal direction - in relation to the root surface, and some - a perpendicular (radial) direction. The latter are called "Sharpey's fibers", and they are very important for fixing the tooth in the alveolus.
2) Secondary (cellular) cement –
Secondary cement is formed after tooth eruption, and it no longer covers the entire surface of the root, but only its apical third + the area of furcations of multi-rooted teeth. It can be placed either on top of the primary cementum or directly adjacent to the root dentin. Secondary cement consists mainly of cells (cementocytes and cementoblasts), as well as intercellular substance, which in turn consists of the main amorphous substance and randomly directed collagen fibers.
- Cementocytes (Fig. 5-6) - lie on the surface of the cement in special lacunae (cavities) and in their structure they are very similar to cementocytes of bone tissue. Cementocytes have long processes, and where the cellular cement is directly adjacent to the surface of dentin, the processes of cementocytes can directly contact the dentinal tubules. When new layers of cement are formed, the cementocytes of the inner layers gradually die, forming empty lacunae in the cement.
- Cementoblasts - these cells are “cement builders”, i.e. ensure the deposition of more and more of its layers. The deposition of cement by cementoblasts occurs throughout a person’s life, and therefore the thickness of cement in the area of the root apices increases several times towards the end of life.
Cementocytes in secondary cementum (histology) –
Fig. 6 (designations), where 1 – cementocyte, 2 – dentinal tubules, 3 – contacts of cementocyte processes with dentinal tubules.
3) Collagen fibers –
The most important part of the collagen fibers of cement are the so-called “Sharpey fibers”. They are the terminal sections of the fibers of the periodontal attachment of the tooth on the cementum side. In Fig. 7 you can see a histological specimen, which shows that the radial collagen fibers of the periodontal fissure and cementum of the tooth root are “a single whole.”
Connection of periodontium and cementum of the tooth root –
Previously, it was believed that the radial fibers of the periodontium (which on one side are fixed to the compact lamina of the alveoli, and on the other to the root cement) were a single whole. But modern research shows that this is not entirely true. The terminal sections of the dento-alveolar fibers of the periodontium begin to form separately from each other: one part - from the side of the cement of the tooth root, and the other part - from the side of the alveolar bone plate.
And when both parts of the fibers reach the middle of the periodontal fissure, they are connected through immature collagen fibers (procollagen fibers) into a single network. The plexus of immature collagen fibers in the center of the periodontal fissure is called the “Siecher plexus” (24stoma.ru).
Summary:
| Acellular (primary) | Cellular (secondary) | |
| localization | – adjacent to dentin, – covers the root. | – covers acellular cement in the area of the apical third of the root and the furcation area of multi-rooted teeth. |
| structure | – collagen fibers (longitudinal and radial arrangement), – amorphous substance, – growth lines are located close to each other. | – cementocytes in lacunae (their processes anastomose with each other), – collagen fibers (chaotic direction), – amorphous substance, – growth lines are located relatively far from each other. |
Dental cement: histology
Below in video 1 you can see the histology of tooth tissue in stunning resolution. Video 2 is the best lecture on cement histology you can hear. The video is in English, but if you wish, you can turn on subtitles, and then select translation from English into Russian in the settings.
Cementocytes and cementoblasts: functions and composition
These two types of cells make up the cellular cement. They have different compositions and perform different functions.
Cementocytes are located in lacunae and resemble osteocytes in structure. The short processes in their composition are directed towards the periodontium. In turn, functionally active cementoblast cells are located on the surface of the cement and are responsible for the regular appearance of new layers on it. They are the ones who take part in the restoration of damaged parts of the tooth, for example, in the event of a traumatic root fracture, they form a “coupling”.
Topography of cement in the area of the tooth neck –
There are 3 options for connecting cement and tooth enamel. It can be either “joint to joint”, or the cement may extend slightly onto the enamel, or there may be a strip of exposed dentin (Fig. 8). Studies have shown that enamel and cement border “joint to joint” - only in 30% of cases. At the same time, 60% of teeth have a layer of cement on the edge of the tooth enamel (Fig. 9), and a strip of exposed dentin is found in 10% of cases.
Variants of the enamel-cementum boundary (scheme and histology) –
Fig. 8, where 1 – enamel, 2 – dentin, 3 – cement, and options for joining enamel and cement (I – cement partially touches the tooth enamel; II – cement joins the enamel, III – cement does not reach the tooth enamel).
Functions of tooth root cement –
1) Protective function – the content of inorganic components in cement reaches 70%, which makes it resistant to mechanical loads. Consequently, one of its functions will be to protect root dentin from damaging effects.
2) Participation in the formation of periodontium - the formation of periodontal fibers occurs simultaneously both from the cementum of the tooth root and from the bone plate of the alveoli. According to a number of authors, these collagen fibers are subsequently intertwined with each other through immature collagen (procollagen), turning them into a single whole. The depth of immersion of periodontal fibers into the cement of the tooth root is from 3 to 5 μ.t.
3) Fixing (retaining) - cement of the tooth root together with the compact plate of the alveolus and periodontal fibers - ensures fixation of the tooth in the alveolus.
4) Compensatory function - when the length of the tooth decreases as a result of physiological abrasion of the enamel, increased production of cement occurs in the area of the apex of the tooth root. As a result, the tooth is pushed out of the alveoli into the oral cavity, and thus the size of the clinical crown of the tooth increases. This becomes especially noticeable in elderly patients.
5) Participation in reparative processes - for example, when the cause of root resorption is eliminated, its partial restoration may occur. Or, if there is a crack in the tooth root, cement may form between the fragments, which can lead to the elimination of the defect.
Reasons for additional formation of cement –
In case of periodontitis and chronic periodontitis, when the enamel on the occlusal surfaces is worn away, when the load on the tooth increases, as well as in the absence of an antagonist tooth, intensive deposition of cement occurs in the area of the apical third of the root (hypercementosis is formed, Fig. 3).
Trauma to the tooth root, as well as orthodontic treatment, can also lead to this. In addition, there is also such a formation as “cementicle”. This is nothing more than a round-shaped formation consisting of cement, located in the periodontium. They arise as a result of mineralization of microvessels in the area of islets of Malasse epithelial cells.
What is hypercementosis
Sometimes during treatment of periodontitis in children or adults, dentists diagnose excessive cement deposition. It often forms over the entire root surface and is caused by chronic infection of the periapical area. Against the background of hypercementosis, the root sometimes fuses with the alveolar wall. This disease develops more often in the lower jaw - mainly in molars and premolars.
The cement in baby teeth is thinner than in molars. As a rule, this is acellular cement, while secondary cement occurs occasionally in the apical part of the root. This trend is also noticeable if we compare the structure of enamel and dentin of adult and children’s teeth: in childhood they are thinner, therefore more sensitive to external factors that cause caries.
Development of cement (cementogenesis) –
The formation of cement occurs in two stages. At stage 1, the synthesis of an organic matrix (cementoid or primary cement) occurs. At stage 2, mineralization of the cementoid occurs - with the formation of secondary cement. Let's look at how this all happens.
First, the cells of the dental papilla (as a result of the inducing influence of the epithelial sheath) differentiate into root odontoblasts, which form root dentin. Next, the cementoblasts of the dental sac begin to produce the organic cement matrix (cementoid), as well as collagen fibers and the main amorphous substance. As a result, cementoid is deposited on the surface of the root dentin - in the form of a highly mineralized structureless “Hopewell-Smith” layer (this layer contributes to the strong attachment of cement to the root dentin).
Next, primary cementum, which does not contain cells, is the first to form. It is slowly deposited as the tooth erupts, covering 2/3 of the root surface (closer to the crown of the tooth). Next, mineralization of the cementoid occurs, which is associated with the deposition of phosphates and calcium carbonate. This process occurs in waves, and then in the apical third of the root and the furcation zone, a cell is formed, i.e. secondary cement. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Therapeutic dentistry” (Politun, Smolyar), 5. “Histology of the oral cavity” (Glinkina V.V.).
Composition of mature dentin
- Inorganic substances – phosphate salts of magnesium and calcium (70%);
- organic substances – type 1 collagen (20%);
- water (10%).
Dentin looks like bundles of collagen fibers containing mineralized intercellular substance. The bundles are penetrated by dentinal tubules with processes of odontoblasts, or Toms' processes. The fibers are arranged differently in different areas. In the outer, or mantle, dentin, formations of the radial direction predominate, in the inner - tangential.