Increased body temperature, painful sensations in the throat, weakness, headache - people usually attribute these symptoms in the spring-winter period to a common cold. However, often such signs indicate the development of a dangerous infectious disease, which doctors call purulent tonsillitis. The disease is manifested by severe inflammation of the tonsils (glands), located in the nasopharynx. The infection primarily affects the parenchyma and lymphoid tissue lining the tonsils. The disease is dangerous due to severe complications that develop when symptoms are ignored and there is no proper treatment.
If you suspect that you have a sore throat and need to consult a doctor, call +7 (499) 653-58-25 - we will definitely help you. Reception is carried out both in the clinic and with a visit to the patient’s home. To register online, fill out the form on the website.
Causes
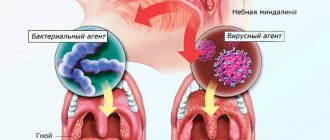
Inflammation of the palatine tonsils is provoked by infections transmitted by airborne droplets. Less commonly, infection occurs through contact and household contact (through shared dishes, towels, bed linen). The most common causative agent of purulent sore throat is hemolytic streptococcus. However, if a person’s immune system works normally, bacteria of this group die immediately after entering the body. The development of pathology is facilitated by weakened immunity and provoking factors.
Indirect causes of purulent sore throat include:
- severe hypothermia;
- chronic diseases of the upper respiratory tract;
- oral infections;
- alcoholism and smoking history;
- stress, overwork, strong emotional tension;
- living in areas with difficult environmental conditions;
- deficiency of vitamins and nutrients;
- mechanical damage to the tonsils (trauma, surgery).
The disease is diagnosed with equal frequency in adults and children.
A sore throat
Roza Ismailovna Yagudina, Ph.D.
Sc., prof., head. Department of Organization of Drug Supply and Pharmacoeconomics and Head. laboratory of pharmacoeconomic research of the First Moscow State Medical University named after. I. M. Sechenov. Evgenia Evgenievna Arinina, Ph.D., leading researcher at the laboratory of pharmacoeconomic studies of the First Moscow State Medical University named after. I. M. Sechenov.
One of the most common complaints in the autumn-winter and, oddly enough, in the summer periods is a sore throat. The causes of painful sensations can be various pathogenetic processes occurring in the human body, and in the summer - also a violation of the environmental situation (humid, dusty air, air conditioners). The most common types of throat lesions are laryngitis, pharyngitis and tonsillitis. The last of these diseases is inflammation of the tonsils. Tonsillitis is the most common cause of sore throat; moreover, the inflammation often has a chronic course.
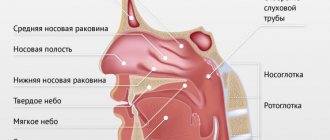
Causes and mechanism of tonsillitis
Sore throat, according to patients themselves, is always associated with hypothermia. However, the etiology of the development of oropharyngeal lesions is very diverse: from bacteria to viruses. The occurrence of pain in these cases is almost always associated with damage to the palatine tonsils, located on the side walls of the oropharynx - the junction of the respiratory and digestive tracts. The tonsils have many lacunae into which crypts or sacs open, having a dichotomous division and immersed in the depths of the tonsils. This structure of the tonsils contributes to the accumulation of various exudates in them. The palatine tonsils do not have afferent lymphatic vessels, since they themselves actively produce lymphocytes. Also, the palatine tonsils take an active part in the formation of local and general immunity.
NB ! A sore throat should not be confused with chronic tonsillitis (more precisely, its exacerbation, which, with similar symptoms, requires different treatment).
Sore throat is a general infectious disease with acute inflammation of the components of the lymphadenoid pharyngeal ring (usually the palatine tonsils). Sore throats are divided into: primary, secondary and specific.
- Primary - ordinary, simple, or banal sore throats. They manifest themselves as acute inflammatory diseases that have signs of damage only to the lymphadenoid ring of the pharynx.
- Secondary - symptomatic tonsillitis. Damage to the tonsils with scarlet fever, diphtheria, infectious mononucleosis, etc., as well as with blood diseases - leukemia, agranulocytosis, acute infectious diseases.
- Specific - sore throats caused by specific infections (fungal tonsillitis, Simanovsky-Plaut-Vincent tonsillitis).
Chronic tonsillitis is a chronic inflammatory, periodically exacerbating focus of infection in the palatine tonsils with a general infectious-allergic reaction.
The mechanism of infection spread is airborne, mainly occurs when coughing, sneezing, kissing, sharing dishes, towels, etc. The most common cause of chronic tonsillitis is group A β-hemolytic streptococcus, other pathogens are St. Aureus, H. influenzae, M. Catarrhalis, N. Gonorrhoeae, C. haemolyticum, M. Pneumoniae, C. pneumoniae, Toxoplasma, anaerobes, adenoviruses, cytomegaloviruses, herpes viruses, etc. Chronic tonsillitis is not always a consequence of previous tonsillitis. In most cases, it develops unnoticed, masquerading as other diseases (ARVI, stomatitis, etc.). As tonsillitis progresses, the parenchyma of the tonsils is slowly replaced by connective tissue, encapsulated foci of necrosis are formed, and regional lymph nodes are involved in inflammation. There are several forms and types of chronic tonsillitis with different symptoms.
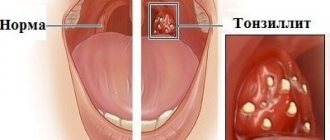
The presence of only local signs characterizes simple tonsillitis (initial stage)
- liquid pus or caseous-purulent plugs in the lacunae of the tonsils (sometimes with an odor);
- tonsils are small, sometimes smooth or with a loose surface;
- persistent hyperemia of the edges of the palatine arches (Gise's sign);
- swelling of the edges of the upper parts of the palatine arches (Zach's sign);
- thickened, roller-shaped edges of the anterior palatine arches (Preobrazhensky sign);
- fusion and adhesions of the tonsils with the arches and triangular fold;
- enlargement of individual regional lymph nodes, sometimes painful on palpation (in the absence of other foci of infection in this region).
Also at this stage, other diseases not related to tonsillitis may worsen, which can have serious consequences.
Toxic-allergic form I (TAF I ) - is caused by repeated previous sore throats. In addition to local symptoms (the same as at the initial stage), general toxic-allergic phenomena develop:
- low-grade body temperature (occasionally);
- weakness, malaise;
- increased fatigue, decreased ability to work;
- periodic joint pain;
- enlargement and pain on palpation of regional lymph nodes (in the absence of other foci of infection);
- functional disorders of cardiac activity (can manifest themselves during exercise and at rest, but only during exacerbation);
- Abnormalities in laboratory data are variable.
Concomitant diseases in this case are the same as in the simple form, but they do not have a common infectious basis with chronic tonsillitis.
Toxic-allergic form II (TAF II ) - characterized by local symptoms inherent in the simple form and general toxic-allergic reactions:
- periodic functional disorders of cardiac activity (disturbances in heart rhythm are recorded on the ECG, pain in the heart area occurs both at the latent stage and at the acute stage);
- joint pain (both at the latent stage and at the acute stage);
- low-grade fever (may be prolonged);
- functional kidney disorders;
- deviations from laboratory data norms.
Concomitant diseases may be the same as in the simple form (not associated with infection). The course of this stage of chronic tonsillitis may be accompanied by the development of severe complications: peritonsillar abscess, tonsillogenic sepsis, etc.
Treatment of tonsillitis
How to get rid of tonsillitis? The palatine tonsils play a large role in the normal functioning of the immune system, so treatment of the disease should first of all include the restoration of the body's protective functions. Pharmacotherapy for chronic tonsillitis includes a set of measures aimed at eliminating the bacterial environment, relieving inflammation and eliminating purulent plugs from the pharyngeal mucosa. Treatment of chronic tonsillitis is carried out in accordance with the form and phase of the disease (acute tonsillitis, latent).
NB ! Conservative therapy is carried out at the initial stage of the disease and TAF I outside the period of exacerbation and not earlier than 1 month after it. Patients with TAF II are indicated for tonsillectomy!
Principles of pharmacotherapy of chronic tonsillitis:
- antibacterial drugs. To treat tonsillitis, various types of antibiotics are used: penicillins (mostly “protected”) or cephalosporins (2nd or 3rd generation), macrolides can be used, less often fluoroquinolones;
- desensitizing drugs that have an anti-edematous effect on tissues and help facilitate tolerance and improve the absorption of prescribed therapy;
- oral antiseptics: miramistin, octenisept at a dilution of 1:5, various gargles, etc. (how to gargle for tonsillitis is described below);
- homeopathic preparations that normalize and improve the trophism of the palatine tonsils;
- drugs that stimulate local immunity of the palatine tonsils.
Antibacterial therapy - what antibiotics are taken for tonsillitis
- Penicillins: preference in this group is given to amoxicillin in combination with clavulanic acid, since it is this combination that ensures the effectiveness of treatment in the event of penillinase-producing staphylococci joining the pathogenic flora. However, they are ineffective against methicillin-resistant strains of Staphylococcus aureus.
- Cephalosporins: cefepime (IV generation), ceftriaxone, cefoperazone, cefixime (III), cefuroxime (II). The first three drugs have only parenteral forms of release, while cefixime is produced only in oral form. Cefuroxime has both forms of release.
- Macrolides: azithromycin, clarithromycin, josamycin. The drugs are active against all pathogens, including penicillin-resistant strains.
- Aerosol forms of antibacterial drugs: fusafungine, active against hemolytic streptococcus, Staphylococcus aureus and Candida albicans.
Immunomodulators
Immunomodulators are prescribed as part of complex therapy. Among vaccine-like immunomodulators that activate both specific and nonspecific local immunity, preparations containing lysates of thirteen microorganisms are used (including lysates of hemolytic streptococcus, Staphylococcus aureus, Candida albicans). A similar mechanism of action (increased phagocytosis, increased lysozyme content, stimulation of immunoglobulin A production) is also characteristic of nasal sprays containing bacterial lysates: Streptococcus pneumoniae type I, II, III, V, VIII, XII, Staphylococcus aureus, Neisseria subflava, Neisseria perflava, Klebsiella Pneumoniae, Moraxella Catarrhalis, Haemophilus Influenzae Type B, Acinetobacter Calcoaceticus, Enterococcus Faecum, Enterococcus Faecalis, Streptococcus Pyogen ES Group A, Streptococcus Dysgalae Group C, Streptococcus Group G. Natural immunostimulating agents are also used: ginseng, leftze, echinacea, chamomile, garlic, garlic, garlic propolis, pantocrine. Peptides with immunoregulatory, detoxification, hepatoprotective, antioxidant effects are also used as an immunomodulator - arginyl-alpha-aspartyl-lysyl-valyl-tyrosyl-arginine, azoximer bromide, glucosaminyl muramyl dipeptide. Recently, herbal medicines such as tonsiral and tonsilgon have become widespread.
Antiseptics
Rinse solutions
An important stage in the treatment of sore throat is the sanitation of the oropharynx using a variety of antiseptics. The best option for sanitation is systematic (up to 8-10 times a day) gargling for tonsillitis with antiseptic and anti-inflammatory solutions of furatsilin, tinctures of eucalyptus leaves (have an antimicrobial effect), calendula, propolis (have an antiseptic and anti-inflammatory effect), preparations containing the NSAID agent benzydamine and so on.
Sprays and lozenges
The above-mentioned benzydamine is available not only in the form of a solution, but also in the form of a spray, which provides the so-called “spot” sanitation of the oropharynx. Other sprays used for sore throats contain hexethidine, povidone-iodine, mixtures of camphor, levomenthol, chlorobutanol and eucalyptus oils.
Another convenient local form of throat sanitation is lozenges and lozenges based on the same antiseptics (a combination of dry sage extract with essential oil, ambazone, chlorhexidine in combination with tetracaine and vitamin C). As a rule, in addition to the analgesic effect, tablets and lozenges have a bactericidal, local anesthetic and immunomodulatory effect. The basis for local drugs for resorption can also be drugs from the PNVP group: flurbiprofen, acetylaminonitropropoxybenzene, benzydamine.
Antioxidants
Antioxidants in the treatment of sore throat are used to improve metabolism, restore the functioning of enzyme systems and reduce the destructive effects of free radicals and peroxide compounds, as well as to improve immunity (rutin-containing complexes, vitamins A, E, C, microelements Zn, Mg, Si, Fe , Ca, dietary supplements, etc.).
Criteria for treatment effectiveness
Indicators that the treatment is sufficiently effective are:
- disappearance of pus and pathological contents in the tonsils;
- reduction of hyperemia and infiltration of the palatine arches and palatine tonsils;
- reduction or disappearance of regional lymph nodes.
But even in this case, it is better to carry out courses of treatment at least three times a year, especially during the off-season.
However, if a patient has a relapse even with a simple form of chronic tonsillitis or TAF I, then after the first course of treatment, pus remains in the palatine tonsils and caseous masses form, so it is necessary to discuss with the patient the possibility of tonsillectomy.
Thus, conservative treatment of chronic tonsillitis should to some extent be considered as a stage in preparing the patient for tonsillectomy for chronic tonsillitis TAF I, and in a simple form (if there is a positive result of treatment), the patient must be taught to maintain the tonsils in a satisfactory condition - that is, to carry out prevention chronic tonsillitis. Many people are interested in how to cure chronic tonsillitis once and for all. Unfortunately, there are no universal recipes for the treatment of chronic tonsillitis, since it is a focal infection that constantly reduces immunity and can at any time cause an exacerbation of the patient’s condition.
Table 1. List of drugs for the treatment of chronic tonsillitis in adults and children (group Rx)
Drugs for the treatment of chronic tonsillitis (exacerbation stage). Prescription group (Rx-drugs)*
| INN | TN |
| Penicillin series | |
| Amoxicillin + clavulanic acid | Panclave 2X, Panclave, Augmentin®, Augmentin EC, Augmentin® SR, Amovycombe®, Arlet®, Amoxiclav® Quiktab, Amoxiclav®, Ecoclave®, Flemoklav Solutab, Fibell, Rapiclav, Ranclave®, Medoclav, Liclave, Klamosar, Verclave, Bactoclav , Amoxicillin + clavulanic acid-Vial, Amoxicillin + clavulanic acid, Amoxicillin + clavulanic acid Pfizer |
| Cephalosporins II generation | |
| Cefuroxime | Cefurus®, Cefuroxime Kabi, Cefuroxime, Cefurabol®, Cefuroxime J, Cetyl Lupine, Super, Proxim, Xorim, Kefstar, Ketocef, Zinoximor, Zinacef®, Zinnat®, Acenoveriz®, Antibioxime, Axosef®, Aksetin® |
| III generation | |
| Cefoperazone+[Sulbactam], | Tsefpar SV, Cefoperazone and Sulbactam Spencer, Cefoperazone and Sulbactam Jodas, Cebanex, Sulcefazone, Sulcef, Sulperacef®, Sulperazone, Sulmover®, Sulzoncef®, Pactocef |
| Cefoperazone | Cefpar, Cefoperus®, Cefoperazone-Vial, Cefoperazone-Agio, Cefoperazone, Cefoperabol®, Cefobid®, Ceperon J, Operaz, Movoperiz, Medocef, Dardum |
| Ceftriaxone | Ceftriaxone-Promed, Ceftriaxone-LEKSVM®, Ceftriaxone-KMP, Ceftriaxone-Jodas, Ceftriaxone-Darnitsa, Ceftriaxone-Vial, Ceftriaxone Elfa, Ceftriaxone Protech, Ceftriaxone Kabi, Ceftriaxone DS, Ceftriaxone Danson, Ceftriaxone, Ceftria bol®, Cefson, Cefogram, Cefatrin , Cefaxon, Hizon, Triaxone, Torocef®, Tercef®, Stericef, Rocephin®, Oframax®, Movigip, Medaxone, Loraxone, Lifaxone, Lendacin®, Ifitzer®, Biotraxon, Betasporina, Axone, Azaran |
| Cefixime | Ceforal Solutab, Cemidexor®, Suprax®, Pancef, Pancef®, Ixim Lupin |
| IV generation | |
| Cefepime | Epipim, Cefomax, Cefepim-Jodas, Cefepim-Vial, Cefepim-Agio, Cefepim, Movisar, Maxicef®, Maxipim®, Ladef, Cefsepim, |
| Macrolides | |
| Azithromycin | Ecomed®, Hemomycin, Tremac-Sanovel, Sumatrolide solutab, Sumamox, Sumametcin, Sumamed® forte, Sumamed®, Sumaclid, Safocid, Zi-factor®, Zitrocin, Zitrolide® forte, Zitrolide®, Zitnob®, Zetamax retard, Azicide, AzitRus forte, AzitRus, Azithromycin-McLeodz, Azithromycin-BI, Azithromycin-OBL, Azithromycin Forte, Azithromycin, Azitrox®, Azitral, Azimicin, Azivok |
| Clarithromycin | Ecositrin, Helitrix®, Fromilid Uno, Fromilid, SR-Klaren, Seydon-sanovel, Lekoklar, Coater, Clerimed, Klacid® SR, Klacid®, Klasine, Claromin, Claricite, Claricin, Clarithrosin, Clarithromycin-Teva, Clarithromycin-Verte, Clarithromycin retard-OBL, Clarithromycin Pfizer, Clarithromycin Protech, Clarithromycin Zentiva, Clarithromycin, Clarbact, Klabax®, Klabax OD, Kispar® Zimbactar |
| Josamycin | Vilprafen, Vilprafen solutab |
* State register of medicines
The more appropriate form of release of the drug in this case is determined by the doctor.
Table 2. List of drugs for chronic tonsillitis at the acute stage (tablets, solutions, sprays)
| INN | TN | Release forms |
| Fusafungin | Bioparox® | dosed aerosol for inhalation |
| Lysates of microorganisms | Kameton-MHFP Kameton | aerosol for topical use topical spray |
| Salvia officinalis leaf extract + Salvia officinalis leaf oil | Sage | lozenges |
| Ambazon | Faringosept | lozenges |
| Flurbiprofen | Strepfen, Strepsils® Intensive Rakstan-Sanovel | lozenges [honey-lemon] film-coated tablets |
| Benzydamine | Tantum verde forte Tantum verde | dosed topical spray dosed spray for topical use, solution for topical use, lozenges |
* State register of medicines
Incubation period
The period from the moment the pathogen enters the body until the appearance of the first characteristic symptoms can range from 2 to 6 days. During the first few days, the sick person is still unaware of his condition, becoming a source of infection for others. During the incubation period, the infection is actively transmitted by airborne droplets (through coughing, sneezing, kissing, talking). The onset of the disease is manifested by a feeling of chills, increased body temperature, weakness and headache. The sooner the patient sees a doctor, the easier the treatment is.
Symptoms of purulent sore throat
In most patients, the first signs of purulent tonsillitis appear 2-3 days after the pathogen enters the body. When the patient's immunity is weakened, the clinical picture is most pronounced. In adult patients, the following symptoms are observed:
- the appearance of noticeable white or yellowish spots of pus on the tonsils;
- high body temperature (in the range of 39-40 ° C);
- intense pain in the throat that increases during swallowing;
- significant enlargement of the lymph nodes located under the lower jaw;
- easily removable whitish coating on the tongue;
- severe headaches;
- feeling weak and overwhelmed;
- loss of appetite;
- aching joints.
In adults, with timely treatment, the acute stage of the disease rarely lasts longer than a week. If the patient does not seek help from specialists, there is a risk of complications.
Treatment of tonsillitis plugs
The appearance of plugs indicates long-term inflammation occurring in the body, so the removal of purulent plugs must be combined with measures to treat chronic tonsillitis. Chronic tonsillitis should be treated by a competent otolaryngologist. Only an ENT doctor knows how to treat tonsillitis plugs effectively and safely. There is no need to try to get rid of pustules on your own at home. Many patients begin to put pressure on the tonsils, scraping off the “plaque” with a spoon and other improvised means. But this measure is ineffective - pus is removed only from the surface, but this is only the tip of the iceberg, the main problem is inside. Such inept actions often lead to injury to the tonsils, which will only provoke the appearance of new caseous formations.
Stages of disease development
The disease progresses rapidly. This is especially true in children and adults with a weakened immune response. Symptoms depend on the current state of the body, age, concomitant diseases and the stage of infectious tissue damage.
Signs of the development of the disease at different stages from the moment of infection:
- 2-3 days.
This stage is characterized by the maximum severity of the symptomatic picture. The patient's tonsils increase significantly in size and white or yellowish ulcers appear on their surface. The inflammatory process covers the entire surface of the tonsils. The patient notes deterioration in health, weakness, loss of appetite and signs of fever, including an increase in body temperature to 39-40 ° C. The patient also experiences excruciating pain in the throat, which gets worse when swallowing. - Day 4
The ulcers that form on the tonsils begin to spontaneously open, releasing the contents (pus). In their place, lacunae are formed - characteristic depressions. If at this stage the patient follows the doctor’s recommendations, the lacunae quickly close. - 5-6 day
. At this stage, patients feel a noticeable improvement in their condition - body temperature normalizes, headaches go away, strength and appetite are restored. - 7-10 day
. The last pathological sign – sore throat – recedes. The size of the lymph nodes located under the lower jaw also decreases. The patient ceases to feel pain and discomfort in this area.
Competent and timely therapy allows you to avoid serious complications.
Classification B.S. Preobrazhensky
| Form of the inflammatory process | Distinctive manifestations |
| Simple (uncomplicated) form | Only local signs are present: Pus and dense plugs from it, closing the lumen of the lacunae, and the inflamed surface of the tonsils (they are loose, red, swollen). Inflamed edges of the arches of the palate (they are swollen, red, infiltrated). |
| Toxic-allergic tonsillitis 1st degree | Local manifestations of an uncomplicated form are superimposed by general symptoms of an allergic-toxic nature: Periodic low-grade fever (temperature readings up to 37.5°C). Tonsillogenic intoxication, present constantly or periodically - decreased performance, fatigue, poor appetite, general weakness, malaise, feeling of weakness throughout the body. Enlargement of the lymph nodes of the neck, their soreness. Periodically appearing joint pain. Changes in blood tests - increased leukocytes, accelerated ESR. |
| Toxic-allergic tonsillitis 2nd degree | Signs of the 1st degree are accompanied by severe manifestations of a toxic-allergic nature: Functional ECG changes. Heart pain. Heart rhythm disturbances. Long-lasting low-grade fever. Development of autoimmune complications of tonsillitis. |
Forms of the disease
The form of purulent tonsillitis depends on many associated factors and conditions. The most common three forms of development are follicular, lacunar and ulcerative-membranous (necrotic). Each type is characterized by characteristics of the course, specific lesions of the tonsil tissue and varying duration.
Follicular
Follicular tonsillitis is manifested by pinpoint purulent lesions of the parenchyma of lymphoid tissue and follicles of the tonsils. The disease in 85% of cases is caused by group A streptococci. The remaining cases of infection are associated with staphylococcal infection, Haemophilus influenzae, pneumococcus, and adenovirus. This form of pathology is accompanied by a rapid increase in the symptom complex, severe hyperthermia, sweating, loss of sleep and appetite. Intense pain in the throat can radiate to the ear.
Lacunarnaya
This type of disease causes severe inflammatory damage to the tissues of the peripharyngeal ring. The opening of abscesses is accompanied by the formation of specific perforations on the surface of the tonsils - lacunae. The acute phase of the disease is manifested by an increase in the size of the tonsils, up to difficulty breathing. Along with other symptoms, a characteristic sign of the lacunar type of pathology is bad breath. Sometimes doctors note a noticeable change in voice and diction problems. Inadequate therapy can lead to the development of a paratonsillar or retropharyngeal abscess.
Necrotic
Necrotizing ulcerative tonsillitis is rare (about 5-6% of cases). The main cause of the development of this type of disease is fusospirochetous infection. The rapid development of the infectious-inflammatory process causes the formation of histological changes in the tissues of the palatine tonsils. Violations of vascular permeability, associated with the active production of histamine and cytokines, lead to hypertrophy and sometimes tissue necrosis. The first sign of the disease is the feeling of a “lump in the throat.” Later, a sharp, unpleasant putrid odor appears from the mouth and salivation increases.
Causes of development of chronic tonsillitis
The development of chronic tonsillitis is possible according to 2 scenarios:
- as a result of tonsillitis (acute tonsillitis), which was incorrectly treated or the treatment was not completed;
- as a result of decreased immune defense and constant exposure to aggressive factors (this is a non-anginal option).
The following are aggressive stimuli:
- inhalation of tobacco smoke;
- poor nutrition;
- alcohol abuse;
- carious teeth;
- inflammatory processes in the paranasal sinuses (sinusitis, sinusitis, etc.);
- impaired nasal breathing that occurs when the nasal septum is deviated, polyps or hypertrophy of the inferior turbinates. Under such conditions, the oral mucosa dries out and the formation of immunoglobulin A is disrupted, which reduces the immune defense of the ENT organs.
However, exposure to the described factors alone is not enough for the development of chronic tonsillitis. Currently, it is considered the result of infection with pathogenic bacteria against the background of allergization (altered immune reactivity). Local changes in the lymphoid tissue after previous tonsillitis, as well as the factor of heredity, which manifests itself only under certain conditions of the internal and external environment, also have a role in this process.
Infection. The most common causes are streptococci and staphylococci. In this case, the maximum danger is posed by pyogenic streptococcus, which is called beta-hemolytic (belongs to group A). The risks associated with this pathogen are the likelihood of developing autoimmune diseases, i.e. when your own immune cells damage other cells in your body. This happens with glomerulonephritis, rheumatism, polyarthritis and other similar diseases.
Altered reactivity of the body (its allergization), which is characterized by excessive production of class E immunoglobulins. Under such conditions, the re-entry of antigens (for example, foreign bacterial proteins) triggers an allergic reaction that constantly maintains inflammation. This corresponds to the exacerbation phase of the pathological process.
It has been proven that the likelihood of chronic tonsillitis in people whose first- or second-degree relatives suffered from this disease is much higher than in other people. This is due to the peculiarities of the anatomy of the tonsillar crypts and immune status (tendency to an allergic response).
Diagnosis and treatment
To make a diagnosis and determine treatment approaches, you need to consult an otolaryngologist. Diagnostics is carried out according to the following algorithm:
- collection of medical history and complaints;
- examination of the pharynx using special lighting (pharyngoscopy);
- general and biochemical blood test;
- bacteriological examination of a smear with the preparation of an antibiogram.
How to treat a purulent sore throat is determined by an ENT specialist. In severe cases, hospitalization is required. General medical recommendations include bed rest, drinking plenty of fluids, taking vitamins and restorative medications.
Specific treatment of the disease is a complex of procedures and medications:
- Drug treatment of the oral cavity.
Complex therapy necessarily includes gargling with antiseptic solutions. For this purpose, solutions of furatsilin, manganese, hydrogen peroxide, sea salt, and natural herbal decoctions (chamomile, calendula) are used. This procedure is aimed at removing pathogenic microorganisms from the throat and mouth. - Taking systemic antibacterial drugs.
A full course of antibiotic therapy allows you to get rid of pathogenic flora. Antibiotics and their dosages can only be determined and prescribed by a doctor. The most commonly used drugs are from the groups of penicillins, macrolides and cephalosporins. - Symptomatic therapy.
To alleviate the patient’s condition during the acute stage, the specialist prescribes symptomatic treatment in the form of antipyretics, antihistamines and anti-inflammatory drugs. Sometimes it is recommended to undergo physiotherapeutic procedures during the recovery period.
Correctly selected treatment helps to avoid serious consequences and ensures healing of the affected tissue areas without visible defects.
Treatment of chronic tonsillitis
Chronic tonsillitis is treated using both conservative and surgical methods.
Conservative methods are:
- antibiotics that are prescribed both locally (gargling) and systemically (tablet or injection forms);
- direct washing of lacunae and introduction of antibacterial and anti-inflammatory drugs into them;
- physiotherapeutic procedures (hallotherapy, magnetic laser treatment of lymph nodes, phonophoresis and ultraviolet irradiation of the palatine tonsils).
| Treatment method | Mechanism of action | Target |
| Irrigation of lacunae using a cannula | The lacunae are cleaned of pus, microorganisms, food debris, and epidermal plugs using a jet of antiseptic solution. In the future, an antibacterial and anti-inflammatory drug may be administered | Cleansing lacunae Bactericidal effect Anti-inflammatory effect |
| Washing lacunae using a vacuum nozzle | Due to the action of vacuum, the contents are removed from the lacunae. | Cleaning gaps |
| Magnetic laser therapy (MILTA) | The effect of a magnetic field and laser radiation on the area of inflammation. The microcirculation of the affected area improves, and the local protective properties of the mucous membrane are activated. | Anti-inflammatory effect Activation of local immunity |
| Phonophoresismedicines | The effect of drugs (antibacterial, anti-inflammatory) on the mucous membrane of the tonsils. Under the influence of ultrasound, drugs penetrate into the deep sections of the lacunae. | Anti-inflammatory effect Bactericidal effect |
| Ultraviolet radiation (UV) | Ultraviolet radiation has a bactericidal effect and activates local immunity of the mucous membrane. | Bactericidal effect Activation of local immunity |
Surgical treatment methods:
- Tonsillectomy – removal of the tonsils along with the capsule (instrumental and bloodless technique).
- Destruction of lymphoid tissue in the tonsil (radio wave ablation, cryodestruction).
- Cryptolysis (“soldering” of palatal lacunae).
| Method of therapy | Mechanism of action | Advantages | Indications |
| Tonsillectomy performed with traditional instruments (instrumental) | Isolation of the tonsil and its capsule is carried out with surgical instruments (loop, raspatory) | Speed of surgery | Previous treatment was ineffective. Beta-hemolytic streptococcus was detected. Toxic-allergic form of tonsillitis. |
| Tonsillectomy bloodless | The tonsil is released from the capsule using a laser, radio wave, cold plasma energy or other physical methods | Simultaneous dissection and coagulation of tissue. The intervention is bloodless | Previous treatment was ineffective. Beta-type hemolytic streptococcus was detected. Toxic-allergic form of tonsillitis. |
| Destruction (ablation) of the lymphoid elements of the tonsil | Radio waves, laser, high or low temperatures destroy most of the lymphoid structures of the tonsils | Can be carried out in a clinic setting | Previous treatment was ineffective Simple (catarrhal) form of tonsillitis |
| Cryptolysis | Destruction of the epithelial layer of lacunae due to physical methods of influence. Under such conditions, they stick together, so food particles and microorganisms do not penetrate there, i.e. inflammation cannot develop. | Can be carried out in outpatient settings | Previous treatment was ineffective Simple (catarrhal) form of tonsillitis |
Purulent sore throat in children
If the disease develops in a child, in addition to the main symptoms, digestive disorders often appear - diarrhea, nausea, vomiting. Children may complain of abdominal pain caused by intestinal spasms. The follicular type of pathology is especially difficult for children aged 5-10 years, causing inflammation of the meninges. Young patients often experience fainting, dry cough and complaints of a feeling of a foreign object in the throat.
If parents ignore the symptoms, the pathology becomes chronic. Pediatricians call this condition chronic tonsillitis, exacerbations of which occur 2-3 times a year.
Causes, main risk factors
Up to 30 different colonies of pathogenic microbes can be sown on the surface of the tonsils of patients suffering from chronic tonsillitis. But in crypts and lacunae staphylo- or streptococcus is usually determined. A key role in the pathogenesis of chronic tonsillitis is played by beta-hemolytic strains of streptococcus (type A). Other flora - gram-negative coccal, fungal, viral - have an impact on local immunity, they support inflammation.
There are a number of factors contributing to the occurrence of the disease:
- hypothermia;
- decreased immunity;
- microtrauma of the tonsils;
- foci of inflammation in the mouth and in the head area (caries, sinusitis, adenoids, etc.);
- smoking;
- poor nutrition;
- allergy.
Viruses and bacteria that cause tonsillitis can come from the external environment.
Complications and consequences
The advanced form of the disease leads to inflammatory damage to other organs, including the heart, kidneys, and joints. The most dangerous complications include:
- mediastinitis
– inflammation of the mediastinal tissue; - chronic bronchitis
- inflammatory damage to the bronchi; - sepsis –
spread of infection through the bloodstream; - arthritis -
inflammation of the joints; - glomerulonephritis is
a dangerous kidney disease; - purulent meningitis -
damage to the meninges; - peripharyngeal abscesses
- suppuration of the lymph nodes and tissue of the peripharyngeal space.
Timely access to a medical facility allows you to avoid negative health consequences.
Prevention
By paying attention to preventive measures, you can reduce the risk of developing the disease. Effective prevention includes:
- avoiding hypothermia (wearing warm clothes, monitoring microclimatic indicators in the room);
- regular preventative visits to the dentist to identify the early stages of caries and stomatitis;
- giving up bad habits (smoking, drinking alcohol);
- moderate physical activity, regular walks in the fresh air;
- normalization of diet, sleep and wakefulness;
- compliance with hygiene standards and requirements, maintaining cleanliness in the home and workplace;
- limiting contacts with unfamiliar people during periods of unfavorable epidemiological conditions.
Strengthening the immune system based on leading a healthy lifestyle helps to avoid infection and make it easier to endure purulent sore throat.
If you have a sore throat, call us and we will definitely help you!