Comparative characteristics of the use of local anesthetics in dentistry
Anesthesia is one of the pressing problems of dentistry. The most common and safe way to relieve pain is local anesthesia, the effectiveness of which largely depends on the type and method of use of the anesthetic. The problem of pain and anesthesia attracts the attention of doctors of all specialties, since after the first duty - saving a person’s life - the most important task was and remains to relieve him of pain.
For some people, fear of the upcoming treatment contributes to their refusal to avoid visiting the dental office under any pretext.
Which is subsequently fraught with complications without timely treatment of dental caries. This includes the occurrence of complicated forms of caries with the formation of chronic foci of odontogenic infection, which contribute to the development or aggravate the course of a number of foci of conditioned diseases and pathological conditions (rheumatism, nephritis, iridocyclitis, etc.), and the occurrence of acute purulent-inflammatory processes - periostitis, osteomyelitis , phlegmon and abscesses, which are sometimes life-threatening. Therefore, pain management is one of the most pressing problems of modern dentistry. Ensuring complete painlessness is very important in the daily practice of a dentist. Imperfect treatment methods, shortage of anesthetics, lack of motivation, and often incompetence of dentists contribute to the deterioration of the quality of qualified dental care provided to the population.
The purpose of this work is to identify the effectiveness of various anesthetics during surgical interventions against the background of acute and chronic inflammatory processes.
Mechanism of action
Penetrating through the nerve fiber membrane, anesthetics bind to the receptor in the area of sodium channels on the inner surface of the membrane. Blocking the membrane's sodium channels then prevents the generation of an action potential. Accordingly, the conduction of afferent impulses from receptors in the central nervous system and impulses along the autonomic nerves, and in high concentrations along the motor nerves, is also blocked. But the transmission of nerve impulses is temporarily blocked. When the action of local anesthetics wears off, the function of sensory nerve endings and conductors is completely restored. Local anesthetics act on any part of the nervous system and on any fibers: small fibers are more sensitive to the action of anesthetics than large ones. In this case, unmyelinated fibers are more easily blocked than myelinated ones. First of all, local anesthetics relieve pain, then taste, temperature and tactile sensitivity. Complete anesthesia, i.e. anesthesia is achieved by blocking the conduction of excitation along all groups of sensory fibers. After absorption of local anesthetics into the blood, systemic and toxic effects may develop. The central nervous system and cardiovascular system are most sensitive to the action of local anesthetics[1].
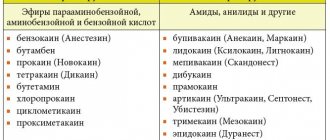
Comparative characteristics of local anesthetics
| Lidocaine | Mepivacaine | Artikain | |
| Plasma protein binding | 50% | 78% | 95% |
| Half-life in minutes | 96 | 114 | 29 |
| Anesthetic activity | 4 | 4 | 5 |
| Toxicity | 2 | 1,7 | 1,5 |
| Duration of anesthesia (in min) without vasoconstrictor | 30-60 | 45-90 | 60 |
| Duration of anesthesia (in minutes) with a vasoconstrictor | 120-130 | 120-130 | 180 |
| Maximum permissible dose (mg/kg) with vasoconstrictor | 7 | 6,6 | 7 |
| Maximum permissible dose (mg/kg) without vasoconstrictor | 4,5 | 4,5 | 5 |
| Speed of action | Fast | Fast | Very fast |
RATIONALE FOR THE CHOICE OF DRUGS FOR LOCAL ANESTHETICS
The effectiveness profile of local anesthetics is characterized by the following parameters:
– onset of anesthesia, which is defined as the time between injection and complete anesthesia;
– successful anesthesia, which is defined as the percentage of achieving complete anesthesia (electroodontodiagnosis, the patient’s reaction to the manipulation);
– effective dose - the dose that provides complete anesthesia;
– duration of anesthesia, which is defined as the duration of complete anesthesia;
– spread of anesthesia, which is defined as penetration into soft tissues and adjacent teeth (S. Malamed, 1990) [7].
Conclusion.
1. Ultracaine can be used in patients with hyperalgesia during traumatic interventions and if it is necessary to create severe ischemia to reduce bleeding during the intervention, regardless of the phase of inflammation.
2. Lidocaine is more rationally used during operations on soft tissues, periodontal disease, and removal of mobile teeth.
3. In patients with chronic inflammatory processes, local anesthesia with anesthetics with and without a vasoconstrictor did not make any significant difference.
4. In case of acute inflammation, it is more rational to use 4% ultracaine solution with a vasoconstrictor, due to the most effective anesthesia both in terms of duration and intensity.
anesthetic_activity_and_toxicity
Local anesthetics of the ester groupAnesthetics of the ester group undergo hydrolysis in tissues more quickly, since the ester bonds are unstable.
In the blood, their hydrolysis is accelerated by pseudocholinesterase. Anesthetics of this group act for a short time. DICAINE.
Synonyms: Amethocaine, Anethaine, Decicain, Felicain, Foncaine, Intercain, Medicain, Pantocain, Pontocaine hydrochloride, Rexocaine, Tetracaini hydrochloridum, Tetracaine hydrochloride, etc. Due to high toxicity (10 times more toxic than novocaine), the drug is used only for topical anesthesia of the mucous membrane membranes of the mouth and nose.
It is advisable to use 0.25%, 0.5% and 1% solutions. In some cases, most often when anesthetizing small areas, 2–3% solutions of dicaine can be used. The highest single dose of the drug for adults is 0.09 g (3 ml of a 3% solution). Since the drug is easily absorbed and a slight excess of the therapeutic dose can cause severe intoxication and even death, it is not used in pediatric dentistry. ANESTHESIN.
Synonyms: Benzocaine, Aethylis aminobenzoas, Anaesthalgin, Anaesthicin, Anaesthin, Benzocain, Ethoforme, Ethylis aminobenzoas, Ethyl aminobenzoate, Norcain, Parathesine, Rhaetocain, Topanalgin, etc. The substance is not soluble in water.
Can be used for superficial anesthesia in the form of powders or 5–20% oil solutions. For anesthesia of wound and ulcerative surfaces, it can be used in the form of a 5–10% ointment. The highest dose for adults: single dose 0.5 g, daily dose 1.5 g. NOVOCAINE.
Synonyms: Aethocain, Allocaine, Ambocain, Aminocaine, Anesthocaine, Atoxicain, Cerocain, Chemocain, Citocain, Ethocain, Genocaine, Herocaine, ISOCain, Jenacin, Maresaine Minocain, Naucain, Neocaine, Pancain, Paracaine, Planocaine, Polocainum, Procaine, Procaini Hydrochloridum , Procaine hydrochloride, Protocaine, Sevicaine, Syncaine, Syntocain, Topocaine, etc. In terms of activity, novocaine is 4–5 times inferior to dicaine.
For infiltration anesthesia, 0.25%, 0.5% and 1% solutions are used, and for conduction anesthesia, 1% and 2% solutions are used. It must be taken into account that with the same total dose of the drug, the higher the concentration of the solution used, the higher the toxicity. The drug has moderate vasodilating properties. The highest single dose for adults: when using a 0.25% solution, no more than 500 ml (1.25 g); 0.5% solution - 150 ml (0.75 g); 1% solution - 75–100 ml (0.75 g) and 25–30 ml of 2% solution (0.5 g). The total dose should not exceed 2 g. With the resorptive effect (the effect of drugs or toxic substances that manifests itself after they are absorbed into the blood) of novocaine, depression of the central nervous system, moderate analgesic, and anti-shock effect are noted. The drug has a ganglion-blocking, vasodilating, antiarrhythmic effect, and improves microcirculation. Novocaine is low-toxic, but often causes allergic reactions (stomatitis, dermatitis, Quincke's edema and even anaphylactic shock). With increased sensitivity to novocaine, the patient experiences dizziness, weakness, drop in blood pressure, collapse, shock. Therefore, when collecting anamnesis, you should pay attention to the patient’s tolerance not only to novocaine, but also to other anesthetics similar in structure to novocaine (anesthesin and dicaine), since there may be cross-allergy to them. Novocaine reduces the activity of sulfonamides, since one of its metabolites is para-aminobenzoic acid, and the antimicrobial effect of sulfonamides is based on competitive antagonism with para-aminobenzoic acid. Local anesthetics of the group of complex amides
Local anesthetics of the amide group are inactivated more slowly in the body, are not destroyed by blood cholinesterase, act longer, and therefore are more effective.
Their main advantage is that they diffuse better into the tissue at the injection site, act faster, have a larger anesthesia zone and stronger interaction with tissue, which prevents the local anesthetic from entering the bloodstream. LIDOCAINE
. Synonyms: Xycaine, Xylocaine, Lidestin, Acetoxyline, Alocaine, Anestacon, Anestecain, Astracaine, Dolicaine, Dulcicaine, Esracaine, Fastocaine, Leostesin, Lidestin, Lidocaine, Lidocard, Lidocaton, Lignocain, Maricain, Nulicaine, Octocaine, Remicaine, Solcain, Stericaine, Xycain, Xylesin, Xylocain, Xylocard, Xylocitin, Xyloton, Xylotox, etc. Lidocaine is the first amide anesthetic used in dentistry, it is four times more effective than novocaine and approximately twice as toxic, has a deeper and longer-lasting anesthetic effect than novocaine. This allowed it, in the 50s, to become one of the most popular anesthetics used in dentistry. According to its chemical structure, lidocaine is an acetanilide derivative. Unlike novocaine, it is not an ester, is metabolized more slowly in the body and acts longer than novocaine. Due to the fact that during its metabolism in the body there is no formation of para-aminobenzoic acid, it does not have an antisulfonamide effect and, unlike novocaine, can be used in patients receiving sulfonamide drugs. Along with local anesthetic activity, lidocaine has pronounced antiarrhythmic properties. Lidocaine is a strong local anesthetic that causes all types of local anesthesia: terminal, infiltration, conduction and is considered the ancestor of all amide drugs. Compared to novocaine, it acts faster, stronger and longer. The relative toxicity of lidocaine depends on the concentration of the solution. In low concentrations (0.5%) it does not differ significantly in toxicity from novocaine; with increasing concentration (1% and 2%), toxicity increases (by 40–50%). For infiltration and conduction anesthesia in dentistry, a 2% anesthetic solution is used, and for terminal (application) anesthesia of the oral mucosa, a 10% aerosol solution produced abroad (lidestin) is used; in surgery, the aerosol is used when changing dressings and opening abscesses etc. The aerosol can contains 750 doses of 10 mg lidocaine. The amount of sprayed drug depends on the surface to be anesthetized. In adults, the dose should not exceed 200 mg, i.e. 20 sprays; in children over 2 years of age, 1–2 doses of the drug are prescribed once. The aerosol should not come into contact with the eyes. Lidocaine, used in doses that do not cause seizures, has a sedative effect. The drug is contraindicated in patients with severe liver pathology. The highest single dose for adults is a 2% solution up to 20 ml. With rapid entry of the drug into the bloodstream, a decrease in blood pressure and collapse may be observed; reducing the hypotensive effect is achieved by administering vasoconstrictors. Contraindications for the use of lidocaine are as follows: sick sinus syndrome in elderly patients;
- severe bradycardia;
- cardiogenic shock;
- severe liver disorders;
- hypersensitivity to the drug.
Pregnant and lactating women should be prescribed lidocaine according to strict indications. In children under 2 years of age, the use of lidocaine aerosol is allowed only after its preliminary application to a cotton swab. In case of overdose, psychomotor agitation, tremor, clonic-tonic convulsions, collapse, and central nervous system depression are observed. To treat this complication, short-acting barbiturates and benzodiazepine tranquilizers are used. With the simultaneous administration of lidocaine and beta-blockers (drugs used for paroxysmal tachycardia, extrasystoles, angina pectoris, hypertension - Inderal, Trazicorcor), the resorptive effects (including toxic) of lidocaine may increase due to the weakening of its inactivation in the liver. In this case, the dose of the drug is reduced. It is irrational to prescribe lidocaine simultaneously with antiarrhythmic drugs - drugs used to treat paroxysmal tachycardia, atrial fibrillation and extrasystole (ajmaline, quinidine, etc.) due to increased cardiodepressive effects. Combined use with procainamide (an antiarrhythmic drug) can cause central nervous system stimulation and hallucinations. The combined administration of lidocaine with MAO inhibitors (antidepressants, for example, iprazide), polymyxin B (an antibiotic used for staphylo-, strepto-, pneumo-, gono- and meningococcal infections), diphenin (an anticonvulsant used to treat epilepsy) is also contraindicated. Storage: the drug should be stored in a place protected from light at room temperature. MEPIVACAIN.
Synonyms: Scandicain, Scandonest, Carbocain, Isocain, Mepivastesin, Mepicaton, Mepidont. Used for infiltration and conduction anesthesia in the form of a 3% solution, 2% solution with adrenaline (1/100,000) and norepinephrine (1/100,000). In terms of effectiveness and toxicity, a 2% solution of mepivacaine is approximately equal to a 2% solution of lidocaine (the drug does not cause a cross-allergic reaction with ether anesthetics). Unlike most active substances in anesthetic solutions, which have vasodilatory properties, mepivacaine has a vasoconstrictor effect, which allows the use of a solution with a reduced vasoconstrictor content. In this regard, a 3% solution of mepivacaine hydrochloride in therapeutic dentistry today is the drug of choice for patients for whom the use of vasoconstrictors is contraindicated. Contraindications for the use of mepivacaine are as follows:
- allergy to local anesthetics belonging to the same group;
- severe myasthenia gravis;
- low plasma cholinesterase levels;
- serious liver disorders: cirrhosis, hereditary or acquired porphyria.
The maximum single dose of the drug is 2.7 mg per 1 kg of body weight or 162 mg (3 carpules) for a weight of 60 kg. For children, the total dose should not exceed 1 carpule and is 1.33 mg per 1 kg of body weight. In case of overdose, clonic convulsions appear as a result of intoxication of the nervous system. ARTICAINE.
Synonyms: ultracaine, carticaine, septonest, ubistezin, etc. A drug for local anesthesia in dentistry.
Articaine is a local anesthetic of the amide type of the thiafene group. The drug provides a reliable anesthetic effect. Wound healing after surgical interventions proceeds without complications, which is due to good tissue tolerance and minimal vasoconstrictor effect. Due to the low content of adrenaline in articaine preparations, its effect on the cardiovascular system is weak: there is almost no increase in blood pressure and heart rate. Articaine preparations have low toxicity. However, articaine preparations produced by different companies under different trade names differ to one degree or another in composition: Ultracaine D-S
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 6 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, water for injection.
Ultracaine D-S Forte
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 12 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, water for injection.
Ubistezin Forte
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 12 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, water for injection
Septanest
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 10 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, EDTA, water for injection Articaine acts faster than lidocaine, the effect of the drug begins within 1–3 minutes, the duration of anesthesia is 60–180 minutes. It has a high diffusivity and degree of binding to plasma proteins (95%), low fat solubility. Articaine penetrates well into tissues, can provide anesthesia of the palate after buccal infiltration anesthesia and anesthesia of the pulp after infiltration anesthesia in the lower jaw from 35 to 45. The lipophilicity of articaine is less than that of other amide anesthetics, however, low toxicity in comparison with lidocaine and mepivacaine allows the use of this the drug in the form of a 4% solution of articaine hydrochloride with adrenaline (epinephrine) in dilutions of 1:100000 and 1:200000. Due to the fact that articaine preparations do not usually contain paraben (an antibacterial preservative), these anesthetics can be used in patients who are allergic to parahydroxybenzoates or chemically related structures. The stability of the anesthetic is achieved by high quality packaging (ampoules and carpules) and high chemical purity of the active substance. However, it should be remembered that Ultracain, produced in 20 ml bottles, contains 0.05 mg of methylparaben. The maximum single dose of the drug solution is 12.5 ml (7 carpules) for an adult weighing 70 kg (7.0 mg/kg articaine). When using articaine preparations, the following side effects are possible:
- From the central nervous system: depending on the dose used, cases of impaired consciousness up to its loss have been described; breathing problems; muscle tremors, involuntary muscle twitching, sometimes progressing to generalized convulsions; nausea, vomiting.
- On the part of the visual organs: blurred vision, transient blindness, diplopia (rare).
- From the cardiovascular system: moderately severe hemodynamic disturbances, manifested by a decrease in blood pressure, tachycardia or bradycardia.
- Allergic reactions: swelling or inflammation at the injection site; in other areas - redness of the skin, itching, conjunctivitis, rhinitis, angioedema of varying severity (including swelling of the upper and/or lower lip and/or cheeks, glottis with difficulty swallowing, urticaria, difficulty breathing). All these phenomena can progress to the development of anaphylactic shock.
- Local reactions: swelling or inflammation at the injection site.
- Other: headaches (probably associated with the presence of adrenaline in the drug). Other side effects caused by the action of adrenaline (tachycardia, arrhythmia, increased blood pressure) occur rarely, since the concentration of adrenaline is insignificant.
- Drug interactions: The hypertensive effect of sympathomimetic amines such as epinephrine may be enhanced by tricyclic antidepressants and MAO inhibitors. Interactions of this type have been described for epinephrine and norepinephrine when used as vasoconstrictors at concentrations of 1:25,000 and 1:80,000, respectively. Although the concentration of epinephrine in articaine preparations is significantly lower, this possibility should nevertheless be taken into account. Sometimes, accidental intravascular injection can lead to the development of ischemic zones at the injection site, in some cases progressing to tissue necrosis. Damage to the facial nerve, up to the development of facial paralysis, occurs only when the injection technique is violated. Comparative characteristics of local anesthetics
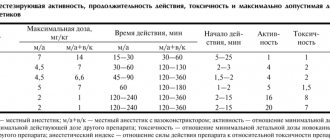
| Novocaine | Lidocaine | Mepivacaine | Artikain | |
| Plasma protein binding | 5,8 % | 50 % | 78 % | 95 % |
| Half-life in min. | – | 96 | 114 | 29 |
| Anesthetic activity* | 1 | 4 | 4 | 5 |
| Toxicity* | 1 | 2 | 1,7 | 1,5 |
| Duration of anesthesia (in minutes) without a vasoconstrictor | 15–30 | 30–60 | 45–90 | 60 |
| Duration of anesthesia (in minutes) with a vasoconstrictor | 4030 | 130120 | 130120 | 180 |
| Maximum permissible dose (mg/kg) with vasoconstrictor | 14 | 7 | 6,6 | 7 |
| Maximum permissible dose (mg/kg) without vasoconstrictor | 7 | 4,5 | 4,5 | 5 |
| Speed of action | Slow | Fast | Fast | Very fast |
The use of local anesthetics in recommended doses is relatively safe (with the exception of allergic reactions). Statistics of complications and side effects during local anesthesia are not very accurate and are more likely related to the error in the choice of drug and its dosage. The practice of using local anesthetics should take into account the individual maximum dose of the drugs used. It is usually determined according to the patient's body weight. The dentist should always strive to achieve effective pain relief using the minimum amount of anesthetic. Recommendations, in this regard, suggest using a dose not exceeding 50% of the maximum toxic dose. In cases where the volume of dental intervention requires the use of local anesthetics in a dosage exceeding 50% of the maximum dose, it is necessary to ensure the possibility of providing the patient with anesthesia, including free access for intravenous injections, oxygen inhalation, assisted or artificial ventilation. It is very important to collect the following anamnestic data before using local anesthesia:
- whether local anesthesia was previously used;
- were there any complications of local anesthesia;
- whether there were allergic reactions to local anesthetics;
- identify risk factors (chronic diseases).
Reference materials
| Indicators | [ Notes | |
| CHARACTERISTICS OF LOCAL ANESTHETICS | ||
| Action point | sensory nerve endings and conductors | |
| Chemical structure | weak grounds | |
| Solubility in water | sparingly soluble | |
| Water soluble form | hydrochloric acid salts of local anesthetics | |
| Mechanism of action | hydrolysis of the salt, release of the anesthetic base, highly soluble in fats and penetrating through the phospholipid membrane of the nerve fiber; interaction with membrane receptors; disruption of ion transport (primarily Na) across the membrane | |
| Pharmacological effect | blockade of nerve impulses | |
| Local anesthetics: | ||
| a) ester groups | novocaine, anestezin, dicaine | |
| b) amide groups | lidocaine, trimecaine, mepivacaine, articaine, bu-pivacaine | |
| Novocaine | ||
| Synonym | procaine | |
| pKa | 8,9-9,1 | |
| Hydrolysis rate | hydrolyzes slowly in tissues | |
| Advance speed anesthetic effect | the effect develops within 6-20 minutes | |
| Fat solubility | low | |
| Types of anesthesia | infiltration and conduction | |
| Duration of anesthesia | 1 5-30 minutes | |
| Effect on blood vessels | expanding | |
| Duration of anesthesia from vasoconstrictor | up to 60 minutes | |
| Effective concentrations for dental practice | 1-2% | |
| pH of solution without vasoconstrictor | 5,0-6,5 | |
| pH of solution with vasoconstrictor | 3,5-5,5 | |
| Metabolism | quickly hydrolyzed in the body by esterases in plasma, tissues and liver | |
| Indicators | Notes | |
| Local anesthetic activity | moderate | |
| Breadth of therapeutic action | big | |
| Maximum dose | 500mg | |
| Action on the central nervous system | depressing | |
| Other pharmacological effects | ganglion blocking, antiarrhythmic, antispasmodic, analgesic, antishock, antipruritic, improves microcirculation | |
| Side effects | allergic reactions, with hypersensitivity - general weakness, nausea, dizziness, hypotension, increased heart rate, collapse, allergic skin reactions, stomatitis, Quincke's edema, anaphylactic shock | |
| Overdose | dizziness, paresthesia, motor agitation, epileptic convulsions, shortness of breath, collapse | |
| Contraindications | hypersensitivity to the drug, congenital pseudocholinesterase deficiency, myasthenia gravis, hypotension, treatment with sulfonamides, purulent process at the injection site | |
| Cautions | use with caution in severe diseases of the heart, liver and kidneys | |
| Lidocaine | ||
| Synonyms | xycaine, xylodont, xylocaine, lignocaine, li-docart, luan, octocaine | |
| Chemical structure | amide derivative of xylidine | |
| pKa | 7,7-7,9 | |
| Hydrolysis rate | quickly hydrolyzes in tissues | |
| Speed of onset of anesthetic effect | the effect develops within 2-4 minutes | |
| Fat solubility | high | |
| Types of anesthesia | superficial, infiltration, conductive | |
| Duration of anesthesia | pulp anesthesia using 2% lidocaine - 5-10 minutes, soft tissue - 60-120 minutes; in dental practice, lidocaine with a vasoconstrictor is used; lasts up to 75 minutes | |
| Effect on blood vessels | actively dilates blood vessels | |
| Duration of anesthesia from vasoconstrictor | with the addition of adrenaline hydrochloride (1:50000 or 1:100000), the duration of pulpal anesthesia is 60 minutes, soft tissue anesthesia is 3-5 hours | |
| Effective concentrations for dental practice | for infiltration and conduction anesthesia in dentistry - 1-2% solution, for surface anesthesia - 4-10% solution; for terminal anesthesia of the mucous membranes, use no more than 2 ml of 10% lidocaine solution (200 mg) | |
| pH of solution without vasoconstrictor | 6,5 | |
| pH of solution with vasoconstrictor | 5,0-5,5 | |
| Metabolism | metabolized in the liver by microsomal oxidases | |
| Local anesthetic activity | is 2-4 times more active than novocaine | |
| Maximum dose | 4.4-6.6 mg/kg body weight for adults and children, but not more than 300 mg | |
| Other pharmacological effects | sedative and antiarrhythmic | |
| Side effects | headache, nausea, anxiety, dizziness, hypotension, collapse, tinnitus, blurred vision, bradycardia, allergic skin reactions, stomatitis, convulsive twitching, tremor, rarely - allergic reactions, anaphylactic shock | |
| Overdose | the phase of stimulation of the central nervous system is replaced by a phase of inhibition; drowsiness, blurred vision, pallor, nausea, vomiting, decreased blood pressure, muscle tremors, hypotension, vascular collapse, convulsions, depression of the respiratory center are observed | |
| Contraindications | hypersensitivity, weakness of the sinus node, atrioventricular block, severe bradycardia, cardiogenic shock, liver pathology, myasthenia gravis, epileptiform seizures (including history) | |
| Cautions | Use with caution during pregnancy and breastfeeding | |
| Mepivacaine | ||
| Synonyms | isocaine, mepivastezin, mepidont, scandicaine, scandonest | |
| Chemical structure | amide derivative of xylidine | |
| pKa | 7,6 | |
| Hydrolysis rate | quickly hydrolyzes in tissues | |
| Speed of onset of anesthetic effect | the effect develops within 2-4 minutes | |
| Fat solubility | less than lidocaine | |
| Types of anesthesia | infiltration, conductive | |
| Duration of anesthesia | the duration of pulpal anesthesia caused by 3% mepivacaine without a vasoconstrictor is 20-40 minutes, soft tissue anesthesia - 2-3 hours | |
| Duration of anesthesia from vasoconstrictor | addition of a vasoconstrictor (1:200,000 levonorderphin, 1:200,000 adrenaline) to a 2% solution of mepivacaine extends pulp anesthesia to 60 minutes, and soft tissue anesthesia to 3-4 hours | |
| Effect on blood vessels | does not have a vasodilatory effect | |
| Effective concentrations for dental practice | 3% solution without vasoconstrictor, 2% solution with vasoconstrictor | |
| pH of solution without vasoconstrictor | 4,5 | |
| pH of the solution with vasoconstrictor | 3,0-3,5 | |
| Metabolism | metabolized in the liver by microsomal oxidases of mixed function with the formation of inactive metabolites; Hydroxylation and M-demethylation play an important role in the biotransformation process | |
| Local anesthetic activity | is 2-4 times more active than novocaine | |
| Maximum dose | 4.4-6.6 mg/kg body weight for adults and children, but not more than 300 mg | |
| Side effects | mainly with intravascular administration of the drug: euphoria, depression, impaired swallowing, vision, bradycardia, arterial hypotension, convulsions, respiratory depression; allergic | |
| allergic reactions (urticaria, angioedema) are rare | ||
| Overdose | the phase of stimulation of the central nervous system (may not be expressed) is replaced by a phase of inhibition | |
| Contraindications | hypersensitivity, myasthenia gravis, severe liver pathology, porphyria | |
| Cautions | Use with caution in severe cardiovascular diseases, diabetes mellitus, in the elderly, during pregnancy | |
| Artikain | ||
| Synonyms | alfacaine, septonest, ultracaine, ubistezin, cytocartin, brilocaine | |
| Chemical structure | amide derivative of thiophene | |
| pKa | 7,8 | |
| Hydrolysis rate | quickly hydrolyzes in tissues | |
| Speed of onset of anesthetic effect | the effect develops within 1-4 minutes | |
| Fat solubility | lower than lidocaine | |
| Types of anesthesia | infiltration, conductive | |
| Effect on blood vessels | vasodilator effect | |
| Duration of anesthesia from vasoconstrictor | A 4% solution of articaine with a vasoconstrictor (1:100000 or 1:200000 adrenaline) provides pulp anesthesia from 45 to 75 minutes, and soft tissue anesthesia from 2 to 5-6 hours | |
| Effective concentrations for | 4% solution with vasoconstrictor (1:100000 or 1:200000 adrenaline) | |
| dental practice | ||
| pH of solution with vasoconstrictor 1:100000 1:200000 | 4,4-5,2 4,6-5,4 | |
| Metabolism | metabolized in the liver by hydrolysis; additionally, inactivation occurs in tissues and blood by nonspecific esterases | |
| Local anesthetic activity | is 3-5 times more active than novocaine | |
| Maximum dose | 5-7 mg/kg body weight for adults and children, but more than 500 mg | Not |
| Side effects | rarely: allergic reactions, swelling and inflammation at the injection site, headache, blurred vision, moderate hemodynamic and heart rhythm disturbances, diplopia, muscle twitching | |
| Overdose | the phase of stimulation of the central nervous system (may not be expressed) is replaced by a phase of depression, there is a disturbance of consciousness, respiratory depression, until it stops, muscle tremors, convulsions, nausea, vomiting, blurred vision, transient blindness, diplopia | |
| Contraindications | hypersensitivity to articaine, adrenaline, sulfites and other components of the solution, tachyarrhythmia, paroxysmal tachycardia, angle-closure glaucoma, bronchial asthma, blood cholinesterase deficiency, myasthenia gravis | |
| Bupivakaip | ||
| Synonyms | anecaine, marcaine | |
| Chemical structure | amide derivative of xylidine | |
| pKa | 8,1 | |
| Hydrolysis rate | hydrolyzes slowly | |
| Speed of onset of anesthetic effect | in 5-10 minutes | |
| Fat solubility | high | |
| Types of anesthesia | infiltration, conductive | |
| Action on blood vessels | vasodilator effect | |
| Duration of anesthesia from vasoconstrictor | A 0.5% solution of bupivacaine with a vasoconstrictor (1:200,000 epinephrine) provides pulp anesthesia from 90 to 180 minutes, and soft tissue anesthesia from 4 to 12 hours | |
| Effective concentrations for dental practice | 0.5% solution with vasoconstrictor | |
| pH of solution without vasoconstrictor | 4,5-6,0 | |
| pH of the solution with vasoconstrictor | 3,0-4,5 | |
| Metabolism | metabolized in the liver by microsomal oxidases of mixed function with the formation of inactive metabolites; Hydroxylation and M-demegylation play an important role in the biotransformation process | |
| Local anesthetic activity | is 8-10 times more active than novocaine | |
| Maximum dose | 1.3 mg/kg body weight of an adult patient, but not more than 90 mg | |
| Side effects | headache, dizziness, weakness, blurred vision, nausea, vomiting, rarely - allergic reactions | |
| Overdose | cardiac dysfunction, symptoms of central nervous system excitation, hypotension (up to collapse), bradycardia (up to cardiac arrest), ventricular arrhythmias, respiratory arrest, confusion, convulsions | |
| Contraindications | hypersensitivity to the drug or components of the solution, central nervous system diseases (meningitis, tumors, poliomyelitis), intracranial bleeding, severe hypotension, cardiac decompensation, pernicious anemia with neurological symptoms, severe hypoxia, hypercapnia, pregnancy, children (up to 1 2 years) | |
Choice of local anesthetic
articaine anesthetics are recommended and widely used (Zoryan E.V., Rabinovich S.A., Matveeva E.G., 2007; Rabinovich S.A., Vasiliev Yu.L. , 2011). This is due to a number of pharmacological properties. Articaine 4% has relatively low fat solubility compared to lidocaine and mepivacaine and passes less through histohematic barriers.
The metabolism of articaine occurs much faster compared to other anesthetics. Thus, the half-life (t1/2) of articaine is 20 minutes, t1/2 of lidocaine is 90 minutes, t1/2 of mepivacaine is 114 minutes.
Other amide anesthetics: mepivacaine, lidocaine - are the anesthetics of choice in pediatric dentistry for a number of reasons. In the Russian Federation, 2% lidocaine is not available in carpuled form and its use in pediatric practice is limited by the capabilities of outdated technology: ampoules, plastic syringes, large-sized and diameter needles.
Mepivacaine 3% does not contain preservatives or vasoconstrictors. This anesthetic is recommended for use if a child has a concomitant pathology and is intended for short-term interventions. In children with bronchial asthma, the use of 3% mepivacaine (without epinephrine) for local anesthesia is indicated (Zoryan E.V., Rabinovich S.A., Matveeva E.G., 2008). This is due to the fact that this drug does not contain sulfites (epinephrine stabilizer), which can cause an attack of bronchospasm.
Children with pathologies of the cardiovascular system, including congenital ones in the compensation stage, are at risk of developing complications. The use of vasoconstrictors in this category of patients is relatively contraindicated. If possible, non-vasoconstrictor anesthetics should be used, such as 3% mepivacaine.
Preparing for local anesthesia
If the patient is undergoing surgery with local anesthesia, the doctor should explain in advance how to prepare.
Patients should tell their doctor if they are using any medications, especially if they are blood thinning agents such as aspirin or warfarin.
Your doctor may instruct you not to eat anything for several hours before surgery. It is also important not to drink alcohol for 24 hours before taking the anesthetic.
In the doctor's office, the doctor applies a local anesthetic to the appropriate area of the body. It will start to feel numb.
The doctor will not act if the patient does not feel numb.
The anesthetic will prevent any pain, but the patient may still feel pressure during surgery.
Depending on what the procedure is and how anxious the patient feels, a sedative may be prescribed at the same time. This will help the patient feel calm and less anxious.
The doctor will monitor the amount of oxygen in your blood using a small device placed on your finger. In rare cases, a plastic nasal tube will be used to provide supplemental oxygen.
Mechanisms of action and types of anesthetics
Anesthetics are divided into:
- Local
- General: a) inhalation - volatile liquids and gases b) non-inhalation (intravenous)
Table 1
1. Local anesthetics
Local anesthetics reversibly reduce the excitability of sensory nerve endings and block the conduction of afferent impulses in the nerve trunks in the area of direct application, and are used to eliminate pain.
The first drug of this group, cocaine, was isolated in 1860 by Albert Newman from the leaves of the South American shrub Erythroxylon coca. Newman, like many chemists of the past, tasted the new substance and noted a numbness in his tongue. Professor of the Military Medical Academy of St. Petersburg Vasily Konstantinovich Anrep in 1879. confirmed the ability of cocaine to cause anesthesia. In experiments on frogs, he discovered that cocaine had a “paralyzing effect” on the endings of sensory nerves. V.K. Anrep studied the effect of cocaine on himself: an injection of cocaine in a dose of 1 - 5 mg under the skin was accompanied by complete anesthesia - a pin prick or cauterization with a smoldering match did not cause pain. A similar effect was observed when a cocaine solution was instilled into the eye and applied to the mucous membrane of the tongue.
Local anesthetics are classified into esters (anesthesin, dicaine, novocaine) and substituted amides (lidocaine, trimecaine, bupivacaine). Local anesthetics - esters are hydrolyzed by blood pseudocholinesterase and act for 30 - 60 minutes. Their effect is prolonged by anticholinesterase drugs (prozerin). The hydrolysis product, n-amino-benzoic acid, weakens the bacteriostatic effect of sulfonamides. Substituted acid amides are inactivated by the liver monooxygenase system within 2-3 hours. Bupivaquine causes local anesthesia lasting 3-6 hours, after its cessation the analgesic effect persists for a long time.
From the point of view of practical use, anesthetics are divided into the following groups:
- Agents used for superficial (terminal) anesthesia: Cocaine, Dicaine, Anestezin, Pyromecaine
- Agents used primarily for infiltration and conduction anesthesia: Novocaine, Bupivacaine
- Agents used for all types of anesthesia: Lidocaine, Trimecaine
Mechanism of action
Local anesthetics are tertiary nitrogenous bases. They consist of hydrophilic and lipophilic parts connected by ester or amide bonds. The mechanism of action is determined by the lipophilic part, which has an aromatic structure. For application to mucous membranes and skin and parenteral administration, aqueous solutions of hydrochloride salts of local anesthetics are used. In the slightly alkaline environment of tissues (pH = 7.4), salts are hydrolyzed, releasing bases. The bases of local anesthetics dissolve in the lipids of the membranes of nerve endings and trunks, penetrate to the inner surface of the membrane, where they are converted into an ionized cationic form.
Figure 1 | Mechanism of action of local anesthetics
Receptors for local anesthetics are localized in the S6 segment of domain IV of the intracellular part of sodium channels. By binding to receptors, local anesthetic cations prolong the inactivated state of sodium channels, which delays the development of the next action potential. Local anesthetics do not interact with closed channels during the resting potential period. Thus, action potentials do not develop in the area where local anesthetics are applied, which is accompanied by a block in the conduction of nerve impulses. The selective effect of local anesthetics on sensory afferent nerves is due to the generation of long-lasting (more than 5 ms) high-frequency action potentials in them.
First of all, local anesthetics block unmyelinated C and myelinated Aδ and Aβ fibers (afferent pathways conducting pain and temperature stimuli; autonomic nerves). Local anesthetics act on fibers surrounded by a myelin sheath at the nodes of Ranvier. Thick myelinated fibers (afferent pathways that conduct tactile stimulation; motor nerves) respond less well to local anesthetics. In addition, the resistance of motor nerves to anesthesia is due to low-frequency short (less than 5 ms) action potentials. In the focus of inflammation, under conditions of acidosis, the dissociation of hydrochloride salts of local anesthetics and the formation of their free lipid-soluble bases are disrupted, so the analgesic effect is lost. For example, local anesthesia may not be effective for tooth extraction in cases of severe periodontitis.
2. General anesthetics
2.1. Inhalational anesthetics
2.1.1 Volatile liquids
Theories of the mechanism of action of general anesthetics
The effects of inhalational anesthetics cannot be explained by a single molecular mechanism. Most likely, the multicomponent action of each anesthetic is realized through many targets. However, these effects converge on a limited number of changes underlying the physiological effects. At the moment, there are lipid and protein theories of anesthesia, but none of them yet describes the sequence of events occurring from the interaction of the anesthetic molecule and its targets to physiological effects.
Figure 2 | Inhalational anesthetics
The activity of inhalational anesthetics is assessed by the minimum alveolar concentration (MAC). A dose producing 1 MAC prevents movement in response to surgery in half of patients. The potency of general anesthetics correlates with their lipid solubility, suggesting the importance of interaction with hydrophilic targets. In particular, the discovery of a relationship between the strength of an anesthetic and its lipophilicity (Meyer-Overton's rule) gave rise to the lipid theory of the mechanism of action of anesthetics. The lipid theory of anesthesia states that anesthetics dissolve in the lipid bilayer of biological membranes and cause anesthesia by reaching a critical concentration in the membrane. The most sophisticated versions of the lipid theory require that anesthetic molecules cause perturbation (changes in properties) of the membrane.
Figure 3 | Meyer-Overton rule
Figure 4 | In the 20th century, it was shown that the potency of general anesthetics correlates with their ability to inhibit the activity of the soluble enzyme luciferase, which is not a physiological target of anesthetics but serves as a lipid-free model protein molecule for anesthetic binding.
Modern facts suggest that proteins, to a greater extent than lipids, are molecular targets for the action of anesthetics. The interaction of anesthetics with hydrophobic regions of proteins also explains the Meyer-Overton rule. The direct interaction of anesthetic molecules with proteins allows us to explain exceptions to this rule, since any sites of binding with a protein are determined both by the size and shape of the molecule, and by solubility. Numerous physical methods (X-ray diffraction, NMR spectroscopy) confirm that general anesthetics act by directly binding to the amphiphilic cavities of protein molecules, and the size of the bound region explains the effect of “chopping off” the properties (longer alcohols lose their anesthetic properties).
Mechanism of action
Thus, general anesthetics change the physicochemical properties of neuronal membrane lipids and disrupt the interaction of lipids with ion channel proteins. At the same time, the transport of sodium ions into neurons is reduced, the output of less hydrated potassium ions is maintained, and the permeability of chloride channels controlled by GABA-A receptors increases by 1.5 times. The result of these effects is hyperpolarization with increased inhibition processes. General anesthetics suppress the entry of calcium ions into neurons by blocking H-cholinergic receptors and NMDA glutamic acid receptors; reduce the mobility of Ca2+ in the membrane, therefore preventing the calcium-dependent release of excitatory neurotransmitters. The most sensitive to the action of general anesthetics are the polysynaptic systems of the central nervous system—the cerebral cortex (1013–1014 synapses), the thalamus, the reticular formation, and the spinal cord. The respiratory and vasomotor centers of the medulla oblongata are resistant to anesthesia.
Volatile inhalational anesthetics:
- postsynaptically enhance inhibitory transmission by potentiating ligand-gated ion channels activated by GABA and glycine;
- extrasynaptically by enhancing GABA receptors and ionic leakage currents;
- presynaptically by increasing basal GABA release.
Inhalational anesthetics inhibit excitatory synaptic transmission by reducing glutamate release and postsynaptically by inhibiting ionotropic glutamate receptors. The paralyzing effect of local anesthetics involves the spinal cord, while sedation/anesthesia and amnesia involve the supraspinal mechanisms of memory, sleep and consciousness.
2.1.2. Gas anesthesia
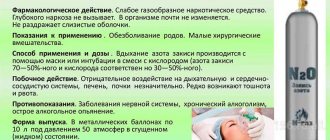
In anesthesiology, the inhalation gas anesthetic nitrous oxide (N2O) is widely used. At the end of the 1980s. The inert gas xenon entered foreign anesthesiological practice.
Nitrous oxide is a colorless gas with a characteristic odor, stored in metal cylinders under a pressure of 50 atm in a liquid state, does not burn, but supports combustion. Its mixtures with anesthetics of the group of volatile liquids are explosive in certain concentrations. In subnarcotic concentrations (20 - 30%) of nitrous oxide causes euphoria (laughing gas) and strong analgesia. At a concentration of 20% it provides pain relief to the same extent as 15 mg of morphine. Nitrous oxide does not affect GABA-A receptors. Used only in combinations, as the MAC is 104%.
The inert gas xenon is considered the best alternative to nitrous oxide, as it has a more pronounced anesthetic effect, indifference and environmental safety. The ability of xenon to cause anesthesia was discovered in connection with the practice of deep-sea diving and the development of hyperbaric physiology. Xenon is colorless, does not burn and has no odor; upon contact with the mucous membrane of the mouth, it creates a sensation of a bitter metallic taste on the tongue. It is characterized by low viscosity and high solubility in lipids, and is excreted unchanged by the lungs. A xenon-saving anesthesia technology has been developed that includes a minimum flow and a recycling system for repeated reuse of gas. This technology successfully solves the practically important problem of the shortage and high cost of xenon. In the mechanism of the anesthetic effect of xenon, blockade of cytoreceptors of excitatory neurotransmitters - H-cholinergic receptors, NMDA receptors of glutamic acid, as well as activation of receptors of the inhibitory neurotransmitter glycine are important. When interacting with cytoreceptors, xenon acts as a proton-binding cluster and forms complexes with the cations HCO+, NH2+, HNCH+. Xenon exhibits antioxidant and immunostimulant properties, reduces the release of hydrocortisone and adrenaline from the adrenal glands.
2.2. Non-inhalation (intravenous) anesthetics are divided into three groups:
Short-acting drugs (3 - 5 min)
- propanidine (epontol, sombrevin)
- propofol (diprivan, recofol)
Medium-acting drugs (20 - 30 min)
- ketamine (calypsol, ketalar, ketanest)
- midazolam (dormicum, flormidal)
- hexenal (hexobarbital sodium)
- thiopental sodium (pentothal)
Long-acting drugs (0.5 - 2 hours)
- sodium hydroxybutyrate
Figure 5 | General anesthetics for intravenous administration
Mechanism of action
The most widely used intravenous anesthetic is propofol. Its mechanism of action is associated with an increase in chloride conductivity of GABA receptors.
Methohexital is close to propofol in terms of the speed of onset and recovery from anesthesia.
Barbiturates were used for anesthesia before the introduction of propofol. Thiopental causes rapid onset and rapid recovery from anesthesia with a single injection, but it accumulates rapidly with repeated or prolonged administration and thus slows recovery from anesthesia. Barbiturates are ligands of barbiturate receptors. In small doses, they allosterically enhance the effect of GABA on GABA A receptors. At the same time, the open state of chlorine channels lengthens, the entry of chlorine anions into neurons increases, and hyperpolarization and inhibition develop. In large doses, barbiturates directly increase the chloride permeability of neuronal membranes. In addition, they inhibit the release of excitatory mediators of the central nervous system - acetylcholine and glutamic acid, and block AMPA receptors ( quisqualate receptors) of glutamic acid. Barbiturates have cerebroprotective properties and can be used for this purpose.
Benzodiazepines are used mainly as anxiolytics and for sedation with preservation of consciousness. All benzodiazepine receptors allosterically enhance the cooperation of GABA with GABA A receptors, which is accompanied by an increase in the chloride conductivity of neurons, the development of hyperpolarization and inhibition. The reaction with benzodiazepine receptors occurs only in the presence of GABA. Remimazolam is the youngest benzodiazepine and has a very short duration of action due to rapid neutralization by plasma esterases.
Ketamine is chemically a derivative of phencyclidine. The synaptic mechanisms of action of ketamine are diverse. It is a non-competitive antagonist of the excitatory brain mediators glutamic and aspartic acids in relation to NMDA receptors. These receptors activate sodium, potassium and calcium channels in neuronal membranes. When receptors are blocked, depolarization is disrupted. In addition, ketamine stimulates the release of enkephalins and β-endorphin; inhibits the neuronal uptake of serotonin and norepinephrine. The latter effect is manifested by tachycardia, an increase in blood pressure and intracranial pressure. Ketamine dilates the bronchi. When recovering from ketamine anesthesia, delirium, hallucinations, and motor agitation are possible (these adverse events are prevented by the administration of droperidol or tranquilizers). An important therapeutic effect of ketamine is neuroprotective. As is known, in the first minutes of brain hypoxia, excitatory mediators - glutamic and aspartic acids - are released. Subsequent activation of NMDA receptors, increasing the concentration of sodium and calcium ions and osmotic pressure in the intracellular environment, causes swelling and death of neurons. Ketamine, as an antagonist of NMDA receptors, eliminates ion overload of neurons and the associated neurological deficit.
The newest intravenous anesthetic is dexmedetomidine. It is a highly selective α2-adrenergic receptor agonist with sedative, sympatholytic, hypnotic and analgesic effects. Its main action is as an agonist at the a2 receptors in the locus coeruleus.
Sources:
- Theories of the mechanism of action - https://en.wikipedia.org/wiki/Theories_of_general_anaesthetic_action and https://www.esus.ru/php/content.php?id=744
- Vengerovsky A.I., Lectures on pharmacology for doctors and pharmacists 2007
- Kharkevich, Pharmacology ed. 10
- Miller's anesthesia / Ronald D. Miller; associate editors, Neal H. Cohen, Lars I. Eriksson, Lee A. Fleisher, Jeanine P. Wiener-Kronish, William L. Young. - Eighth edition. 2015
Types of Local Anesthesia
The type and dose of anesthesia will depend on many factors. These include patients' age, weight, allergies, body part being operated on, and any current health conditions.
Various drugs are used to block pain. They can be applied by injection or by applying a spray or ointment.
The drug works by targeting specific nerve pathways to prevent the nerves in the area of application from sending signals to the brain.
Typically, the drug takes effect within a few minutes and wears off within a few hours. A stronger and higher dose will last longer.
Cocaine was the first anesthetic, but is now rarely used. Lidocaine is currently the most widely used local anesthetic, but different drugs are used for different purposes.
For longer procedures, bupivacaine is more suitable, but it may be more painful when first used. Therefore, the anesthesiologist may use lidocaine first and then administer bupivacaine if numbness is required for a longer period.
Synthetic anesthetics are similar in structure to cocaine, but these drugs do not have the same potential for abuse.
METHODS OF ANESTHESIA WHEN PERFORMING DIAGNOSTIC AND TREATMENT MANIPULATIONS IN DERMATOLOGY
1Zaraday I.I., 2,3Lyutsko V.V.
1Clinical Hospital No. 1, Minsk
2FGBU DPO IPK FMBA of Russia, Moscow
3FGBU "TsNIIOIZ Ministry of Health of the Russian Federation", Moscow
The article provides a description of the basic anesthesia techniques and drugs used for pain relief in procedural dermatology. Information on the main drugs used in local anesthesia is also provided. Possible complications of anesthesia, side effects of anesthetics, and emergency care in the event of complications are described separately.
Key words: anesthesia, pain relief, procedural dermatology.
THE TECHNIQUES OF ANESTHESIA WHEN PERFORMING DIAGNOSTIC AND THERAPEUTIC PROCEDURES IN DERMATOLOGY
1Zaradey II, 2,3Lutsko VV
1Minsk city clinical hospital N.1
2FGBOU DPO IPK of FMBA of Russia, Moscow
3Federal Research Institute for Health Organization and Informatics of Ministry of Health of the Russian Federation, Moscow
The article describes the basic methods of anesthesia, prepara-ing used during anesthesia in procedural dermatology. Also contains information on the main drugs used during local anesthesia. Separately, describes the possible complications of anesthesia, side effects of anesthetics, emergency care when complications arise.
Keywords: anesthesia, pain management, procedural dermatology.
Performing therapeutic and diagnostic procedures in dermatology is often associated with pain in patients. The severity of the pain experienced depends on the nature of the manipulations and the individual reaction of the patient. Pain is always a subjective sensation and its characteristics also vary greatly from person to person. Pain becomes a serious obstacle to carrying out a particular procedure. To eliminate pain in procedural dermatology, various methods of anesthesia are used.
The term “anesthesia” implies the loss of various types of sensitivity; analgesia implies the shutdown of pain.
There are two types of anesthesia: general (anesthesia) and local (regional, local).
General anesthesia is accompanied by switching off (depression) of consciousness with loss of response to various (including painful) stimuli with the help of drugs acting in various parts of the central nervous system. The technique of general anesthesia is quite complex and requires the necessary special training, equipment and conditions. Modern general anesthesia, as a rule, is multicomponent; it uses drugs that depress consciousness (inhalational and intravenous anesthetics), narcotic analgesics and a number of others. The complex effect of various agents leads to the loss of various types of sensitivity.
Local anesthesia refers to pain relief limited to a specific topographical area within which the intervention is performed.
In dermatological practice, local anesthesia methods remain the most preferred, since they allow achieving effective pain relief in the absence of many risks and complications that accompany anesthesia. The choice of a specific regional anesthesia technique depends on the topical location, volume, duration of the intervention and the training of the specialist.
Local anesthesia, depending on the point of application of the effects of local anesthetics, is usually divided into:
- application (terminal, superficial). During topical anesthesia, a local anesthetic solution is applied in the form of a spray, gel, or cream to the surface of the skin or mucous membranes. The gradual penetration of the drug provides anesthesia lasting from several minutes to an hour;
- infiltration, in which a local anesthetic is administered subcutaneously or intradermally using a syringe. Allows you to provide pain relief when manipulating deeper anatomical structures;
- intravenous under a tourniquet - used for operations on the limbs lasting up to one and a half hours. Local anesthetics are injected into a peripheral vein after a tourniquet is applied;
- conduction (blockade of peripheral nerves, nerve plexuses, epidural, spinal). An anesthetic solution is injected into the area of passage of the peripheral nerve (conductor blockade of the nerve plexuses) or the exit of the nerve root (with spinal and epidural anesthesia). When performed correctly, it provides a reliable analgesic effect and allows you to perform large-scale surgical interventions of varying duration.
The main drugs used for regional anesthesia are local anesthetics. Local anesthetics reversibly block the generation and conduction of nerve impulses along the membranes of nerve cells.
The mechanism of action of local anesthetics is the blockade of “fast-conducting” sodium channels (during the excitation phase of the membrane) due to communication with receptors inside the channels, as a result of which the conformational structure of the channel changes, the current of Ca++ ions is blocked, the generation of the action potential is disrupted and conduction stops. In general, the molecule of local anesthetics includes 3 structural fragments:
1) aromatic ring;
2) intermediate group;
3) amino group;
The nature of the chemical bond between the aromatic ring and the amino group allows local anesthetics to be classified into “ether” and “amide”. Amide anesthetics are more stable and, unlike ether ones, practically do not cause allergic reactions. Local anesthetics with ester bonds are destroyed more quickly, since the body contains many enzymes - esterases (blood, liver, tissue fluids). The amino group is hydrophilic, polar, and determines solubility. It is assumed that an aromatic and amino group are involved in the interaction with the membrane. Fat solubility is the main property that determines the potency of local anesthetics. The membranes of neurons are a lipoprotein matrix, consisting of 90% lipids; local anesthetics with greater ability to dissolve in fats are more powerful. The lipophilicity of local anesthetics facilitates their penetration through neuronal membranes and accelerates their binding to proteins of the intracellular part of the Na channel.
Classification of anesthetics by chemical structure:
esters: novocaine (procaine), dicaine (tetracaine), anesthesin;
- amides: articaine, lidocaine, mepivacaine, prilocaine, trimecaine, bupivacaine, etidocaine.
Table 1 presents comparative characteristics of local anesthetics. Novocaine was used as a standard for anesthetic activity.
Table 1
Comparative characteristics of local anesthetics
| International name of the anesthetic | Drugs (trade names) | Maximum permissible dose (in mg/kg body weight) | Duration of action (per minute) | Anesthetic activity |
| Novocaine | Procaine | 14 | 15-30 | 1 |
| Lidocaine | Lidocaine | 7 | 30-60 | 4 |
| Mepivacaine | Scandinibsa Scandonest | 6.5 | 45-90 | 4 |
| Prilocaine | Citanest | 8 | 30-90 | 4 |
| Artikain | Septinest Brilocaine | 7 | 60 | 5 |
| Bupivacaine | Markain | 1 | 120-140 | 6 |
To reduce systemic effects, toxic effects, bleeding, and prolong the action, local anesthetics are combined in solution with vasoconstrictors. Solutions of local anesthetics are used with the addition of adrenaline to a concentration of 1:200,000, which corresponds to 0.1 ml or 1 drop of a 0.1% solution of adrenaline in 10 ml of solution. Adrenaline is added with caution to patients with severe diseases of the cardiovascular system, uncontrolled arterial hypertension, and thyrotoxicosis.
Application (terminal) anesthesia.
Topical anesthesia is a local anesthesia technique that involves soaking the mucous membrane or skin with a local anesthetic drug.
Indications: pain relief during biopsy, laser procedures, electrocoagulation of surface formations, as well as in cosmetology during hair removal, mesotherapy, and permanent makeup application.
The mechanism of action of superficial anesthesia is the penetration of local anesthetic into the deep layers of the skin or mucous membrane, which causes disruption of the function of nerve receptors and fibers, ultimately leading to blocking the perception of pain and other sensations.
The technique of superficial anesthesia is simple and consists of applying (applying, spraying) an anesthetic to an area of skin or mucous membrane.
Medicines intended for superficial anesthesia are presented in various forms - these are solutions, ointments, gels, sprays, aerosols. The active base is a local anesthetic, most often lidocaine or tetracaine.
A contraindication to surface anesthesia is the patient’s hypersensitivity to any local anesthetic included in the drug.
Almost the only complication of superficial anesthesia is the toxic effects of local anesthetics (discussed in more detail below).
The advantages of topical anesthesia are: ease of use, predictability of effect, development of minor or no edema compared to infiltration anesthesia. The disadvantages include: the length of application time when using dosage forms in the form of a cream, gel, and a short duration of anesthesia.
The main drugs used for
topical anesthesia in procedural dermatology.
Cream "EMLA" (EMLA - Eutectic Mixture of Local Anesthetics): is a water-oil emulsion of two local anesthetics: lidocaine and prilocaine in a 1:1 ratio. The mixture of these anesthetics has a melting point of 18°C, which is approximately room temperature. Thus, the term “eutectic mixture” implies that after application to the skin, both anesthetics pass into a liquid state, despite the fact that they initially have a crystalline structure, facilitating absorption processes through intact skin. The essence of the anesthesia manipulation is to apply the drug “EMLA” to the skin under an occlusive patch. After at least 1 hour for the skin or 5-10 minutes for the mucous membranes, the level of loss of pain perception in the area of cream application required for most manipulations is achieved.
"ELA-MAX" is a special liposomal form of 5% lidocaine.
"Anestol" contains lidocaine, tetracaine, and benzocaine as active ingredients. The drug quickly penetrates the skin and provides a long-lasting analgesic effect (up to 2 hours). Apply as an application 15–20 minutes before the procedure. Does not require occlusion.
“ANE STOP” , gel (contains lidocaine as an anesthetic). Apply to the underlying area as a mask for 15–20 minutes, then remove. The exposure time of the anesthetic is 1 hour, the penetration depth is 3–4 mm.
“Xylocaine” , spray (10% xylocaine solution). The drug is used for short-term superficial anesthesia: pain relief occurs 5 minutes after applying the anesthetic to the exposed skin surface.
The anesthetic " Golden rose" , containing adrenaline, provides a vasoconstrictor and, therefore, a hemostatic effect. It is applied to the skin both before the procedure and during manipulation directly to the wound surface for the purpose of local anesthesia and stopping bleeding.
The anesthetic " Rose" has a similar composition, but is available in the form of an oil, which allows it to be used in areas with hair.
Infiltration anesthesia.
Infiltration anesthesia is a local anesthesia technique that uses the injection of anesthetics intra- or subcutaneously (Figure 1).
Indications: infiltration anesthesia provides a more reliable analgesic effect when removing exophytic formations such as warts and genital warts.
Methodology.
Necessary instruments and materials for infiltrative anesthesia: standard or insulin syringes (depending on the volume of the intervention area), solutions of local anesthetics, antiseptics for treating the surgical field, gauze pads.
Figure 1. Carrying out infiltrative anesthesia.
Infiltration is performed in the direction opposite to the conduction of stimulation by sensory nerves from the central nervous system to the peripheral, interrupting the transmission of pain sensations to the central nervous system at the very beginning of anesthesia. The place where the needle is first inserted should be closest to the center (1). Then the needle is inserted deeper, with each advance a solution is introduced, an infiltrate is created in the subcutaneous tissue (2). The introduction of the solution should be slow, not creating much pressure. If it is necessary to anesthetize a long area, then with each new injection of the needle, a new intradermal nodule (3) is prepared inside, through which the injection is made, continuing infiltration. You can combine infiltration anesthesia with application anesthesia by first irrigating the injection site with an anesthetic solution.
Figure 2. Operating technique and conditions
optimal wound healing, J. Zoltan
For infiltration anesthesia, mainly 0.5-2% solutions of novocaine are used (the highest single dose of a 0.5% solution for adults (150 ml), 0.5-2% solutions of lidocaine (up to 200-300 mg for an adult, 10-15 ml of a 2% solution ), bupivacaine solutions, 0.125% trimecaine solution.
Local complications during infiltration anesthesia.
- pain and burning during injection. Depends on the physicochemical properties of the local anesthetic solution and the speed of its administration. These sensations are always short-lived and can be prevented. Slow administration of the local anesthetic increases the safety and comfort of the injection;
- paresthesia (residual anesthesia): a slight change and decrease in sensitivity, which is almost never accompanied by damage to the nerve along its entire length. No help is required, it resolves spontaneously;
- accidental injection of aggressive liquids (ammonia, hydrogen peroxide, etc.). Clinical picture: during anesthesia, the patient experiences severe pain and a burning sensation in the injection area. Help: stop the injection, determine the nature of the solution used. It is necessary to inject a 0.5% solution of novocaine or a 0.9% solution of sodium chloride into the injection area in a volume 5 times greater than the volume of the injected aggressive liquid, make an incision in the projection of the infiltrate, rinse the wound with a solution of furacillin or saline and drain the wound;
- infection. To prevent this, it is necessary to strictly act in accordance with the rules of asepsis and antisepsis
- hematoma formation. For prophylaxis, advance the needle as the anesthetic is administered and perform an aspiration test before the anesthetic solution is administered.
- Contraindications for infiltration anesthesia: allergic reactions to the anesthetic, local infectious process at the site of the intended injection.
Side effects of local anesthesia caused by the general toxic effect of local anesthetics.
The use of local anesthetics may be accompanied by side effects due to the patient's individual hypersensitivity or drug overdose.
Toxic effects on the central nervous system include drowsiness, dizziness, visual and auditory disturbances, and restlessness. At higher concentrations, any local anesthetic (including cocaine) can cause nystagmus, tremors and, finally, tonic-clonic seizures, followed by central nervous system depression and death. The best method to prevent seizures is to use the minimum dose of anesthetic required to produce anesthesia. If the use of large doses is unavoidable for the prevention of seizures, premedication with benzodiazepines, for example diazepam at a dose of 0.1-0.2 mg/kg parenterally, is advisable. Convulsions caused by local anesthetics can be treated with low doses of short-acting barbiturates, such as thiopental 1-2 mg/kg or diazepam 0.1 mg/kg intravenously.
When applied in too large doses, all local anesthetics can have a toxic effect on nerve tissue. Several cases of residual sensory and motor impairment after spinal anesthesia with the administration of too large volumes of chloroprocaine have been described. It is unknown, however, whether chloroprocaine is more neurotoxic than other local anesthetics.
The effects of local anesthetics on the cardiovascular system are due in part to a direct effect on smooth muscle and myocardial membranes and an indirect effect on autonomic nerve fibers. As indicated in local anesthetics, they block sodium channels in the myocardium and thereby suppress abnormal pacemaker activity, excitability and conductivity. All of these drugs, except cocaine, also reduce the force of the heart's contractions and cause the arteries to dilate, leading to hypotension. Cardiovascular collapse and death occur only when large doses are used.
Bupivacaine is more cardiotoxic than other local anesthetics. Several cases of seizures and cardiovascular collapse have been described after accidental intravenous injection of bupivacaine. This is due to the fact that the blockade of sodium channels by bupivacaine is enhanced by the longer duration of the action potential of myocardiocytes compared to nerve fibers. Unlike lidocaine, the blocking effect of bupivacaine occurs at normal heart rates. Studies have shown that the most common ECG change in bupivacaine intoxication is a slow idioventricular rhythm with wide QRS complexes and electromechanical dissociation. Resuscitation is carried out using conventional supportive methods (timely correction of acidosis by hyperventilation and administration of bicarbonate), as well as the active use of adrenaline, atropine and bretylium. Administration of large doses (> 10 mg/kg) of prilocaine for regional anesthesia can lead to the accumulation of a metabolite (9-toluidine, an oxidizing agent that can convert hemoglobin to methemoglobin). If there is a sufficient amount of methemoglobin (30-50 mg/l), the patient develops cyanosis. These levels of methemoglobinemia are tolerable in healthy individuals, but may cause decompensation in a patient with cardiac or pulmonary disease, requiring immediate treatment. In these cases, reducing agents such as methylene blue or ascorbic acid are used to quickly convert methemoglobin into hemoglobin.
Allergic reactions. Ether local anesthetics are metabolized to para-aminobenzoic acid derivatives. These products cause allergic reactions in some patients. Amides are not metabolized to para-aminobenzoic acid, and allergic reactions to drugs in this group are extremely rare.
A rare and life-threatening form of allergic reaction is anaphylactic shock, characterized by a sharp deterioration in the activity of the cardiovascular system with the development of acute cardiovascular failure and loss of consciousness.
Clinical picture: anxiety, pain behind the sternum and in the abdomen, itching of the face and body, hyperthermia, rash, swelling of the eyelids, mucous membranes of the nose, oral cavity, larynx (asphyxia), Quincke's edema, profuse salivation, nausea, vomiting, pallor, frequent and small pulse, dullness of heart sounds, progressive decrease in blood pressure, difficulty breathing, convulsions up to respiratory and cardiac arrest.
Urgent Care:
- stop administering the drug that caused anaphylactic shock, urgently call a resuscitator or emergency medical team;
- lay the patient down, raise the lower limbs; if the patient is unconscious, turn the head to the side, extend the lower jaw, fix the tongue to prevent asphyxia. Establish oxygen inhalation;
- administer intravenously 0.2-0.5 ml of a 0.1% solution of adrenaline in 5 ml of an isotonic solution of sodium chloride or glucose;
- administer prednisolone at the rate of 3-5 mg per 1 kg of body weight intravenously;
- administer a 2% solution of diphenhydramine 0.5 mg per 1 kg of body weight or a 2% solution of suprastin intravenously;
- to relieve bronchospasm, a 2.4% aminophylline solution is administered intravenously (10-20 ml);
- establish intravenous jet administration of saline solutions to increase the volume of circulating blood and stabilize blood pressure.
Literature
- Sanchez E.A. The use of local anesthesia in dermatocosmetology // Russian Medical Journal. – 2006. – No. 1. – P. 33–35.
- Zhigultsova T.I., Stenko A.G., Vissarionov V.A. Application anesthesia in clinical practice // Breast cancer (issue “Dermatology and cosmetology”). – 2010. – T. 16, No. 23. –P. 1570–1573.
- James Duke. Secrets of anesthesia // M.: MEDpressinform, 2005. -503 p.
- Kuzin M.I., Kharnas S.Sh. Local anesthesia // M. Medicine, 1982.
- Graham-Brown R., Bourke D., Cunliffe T. Practical dermatology // M.: MedPress-inform, 2011. - 360 p.
- Ovechkin A.M., Osipov S.A. Clinical pharmacology of local anesthetics // Regional anesthesia and pain treatment. Thematic collection. Moscow-Tver. - 2004. - From 23-34.
- Singh I, Morris AP. Performance of transdermal therapeutic systems: Effects of biological factors // Int J Pharm Investig. - 2011. - No. 1(1). — R. 4-9
The list of references
1. Sanches EA Primenenie mestnoj anestezii v dermatokosmetologii // Rossijskij medicinskij zhurnal. – 2006. – No. 1. – S. 33–35.
2. Zhigul'cova TI, Sten'ko AG, Vissarionov VA Applikacionnaja anestezija v kli-nicheskoj praktike // RMZh (vypusk “Dermatologija i kosmetologija”). – 2010. – T. 16, No. 23. –S. 1570–1573.
3. Dzhejms Djuk. Sekrety anestezii // M.: MEDpressinform, 2005. -503 s.
4. Kuzin M.I., Harnas S.Sh. Local obezbolivanie // M.Medicina, 1982 g.
5. Grjehem-Braun R., Burk D., Kanliff T. Prakticheskaja dermatologija // M.: MedPress-inform, 2011. - 360 s.
6. Ovechkin AM, Osipov SA Klinicheskaja farmakologija mestnyh anestetikov // Re-gionarnaja anestezija i lechenie boli. Tematicheskij sbornik. Moscow-Tver'. - 2004. - S 23-34.
7. Singh I, Morris AP. Performance of transdermal therapeutic systems: Effects of biological factors // Int J Pharm Investig. - 2011. - No. 1(1). — R. 4-9
Information about authors
Zaraday Igor Ivanovich – Candidate of Medical Sciences, cardiologist, Clinical Hospital No. 1, Minsk, 220013, Republic of Belarus, Minsk, Nezavisimosti Ave., 64.
Minsk city clinical hospital N.1, 220013, 64, Nezalezhnosti Ave., Minsk, Belarus
Lyutsko Vasily Vasilievich – Candidate of Medical Sciences, Associate Professor of the Department of Therapy, Geriatrics and Anti-Aging Medicine, Federal State Budgetary Institution of Further Professional Education, IPK FMBA of Russia, 125371, Russia, Moscow, Volokolamskoye Shosse, 91; Leading Researcher of the Federal State Budgetary Institution "TsNIIOIZ of the Ministry of Health of Russia", 127254, Russia, Moscow, st. Dobrolyubova, 11,
E-mail: This email address is being protected from spambots. You must have JavaScript enabled to view it.">This email address is being protected from spambots. You must have JavaScript enabled to view it.
FGBOU DPO IPK of FMBA of Russia, 125371, 91, Volokolamsk highway, Moscow, Russia
Federal Research Institute for Health Organization and Informatics of Ministry of Health of the Russian Federation, 127254, 11, Dobrolubova Str., Moscow, Russia
Risks and complications
Local anesthesia is generally considered very safe. For minor surgeries it is safer than general anesthesia.
There may be tingling and pain, and there may be bruising as you take the drug and wear it off, but this is usually minor.
A person who has had local anesthesia must be careful not to get hurt when they cannot feel pain, such as when biting their cheek after dental treatment.
Temporary side effects that affect some people include:
- blurred vision, dizziness and vomiting
- headache
- muscle twitching
- persistent numbness, weakness, or tingling
Some people may have an allergic reaction. The patient may experience hives, itching, and difficulty breathing.
Cyanosis may occur, in which the skin turns bluish due to poor circulation or insufficient oxygenation of the blood.
In very severe cases, a person may experience CNS depression, in which the central nervous system slows down too much, resulting in a decrease in breathing and heart rate. This can lead to cardiac arrest if blood stops pumping to the heart.
An overdose of local anesthetic can lead to seizures. This can be life-threatening.